The children of parents with substance use disorders, compared with reference children, have greater liability for psychopathology (i.e., mental disorders other than substance use disorders). Studies have reported increases in mental disorders among children of parents with substance use disorders
(1–
4). Such children and corresponding families have therefore been considered “high risk”
(5). Specific disorders observed at increased rates in the children of parents with substance use disorders include conduct disorder, attention deficit hyperactivity disorder (ADHD), major depressive disorder, and anxiety disorders
(1,
2,
6). These specific forms of offspring psychopathology have thus been definitively shown to be associated with parental substance use disorder.
The extent to which these mental disorders in offspring are a consequence of parental substance use disorders or more specifically associated with corresponding parental psychopathology remains an open question. Parents with substance use disorders typically have had other mental disorders. Analogous to their children, fathers with substance use disorders often have childhood histories of conduct disorder and ADHD as well as major depressive disorder and anxiety disorders
(7). Paternal-maternal concordance for specific mental disorders is common, in part due to assortative mating, and may increase risk in offspring for like disorders
(8–
10).
Several studies have examined the extent to which psychopathology in children is more closely related to parental substance use disorders or to other mental disorders. Using a high-risk design strategy similar to that for the study reported here, Merikangas and colleagues
(8,
11,
12) studied parent-to-child transmission of psychopathology risk in the children of parents with substance use disorders, anxiety disorders, or no history of psychiatric disorders. The study group included 192 offspring, age 7–17 years, from 126 families. Parents and children were directly interviewed. The results indicated a strong family aggregation for anxiety disorders. Maternal substance use disorders and paternal antisocial personality disorder were associated with offspring conduct disorder. Parent psychopathology did not predict ADHD. The study had several limitations, including lack of assessment of parental history of childhood conduct disorder and ADHD, the presence of substance use disorders in some adolescent offspring, and lack of consideration of the clustering of offspring within families in the primary statistical analyses. Including offspring with substance use disorders introduces possible contamination from the onset of substance use disorder leading to psychopathology
(13–
15).
In a study of parents (N=892) and siblings (N=1,149) of probands with cocaine and opioid disorders
(16), maternal depression and anxiety disorders were associated with these disorders in offspring. The study focused on lifetime diagnoses in adults, did not distinguish childhood from substance use disorder-induced disorders, and relied primarily on family informant data, which may be less valid than direct interviews
(17).
Another study design considered the effects of specific parental characteristics through subject selection techniques. Schuckit and colleagues
(18) examined offspring (ages 7–22) of parents with alcohol use disorders (N=37), with a family history of alcohol use disorders only in extended family members (N=68), or with no family history of alcohol use disorders (N=57). The study excluded families where either parent had antisocial personality disorder. These groups were not significantly different in terms of offspring psychopathology, indirectly suggesting that parental antisocial personality disorder may have a major impact on psychopathology in offspring. The small sample may not have yielded sufficient statistical power to reveal relevant relationships. In a report on a subset of subjects included here, Moss and colleagues
(19) reported that offspring of fathers with substance dependence and antisocial personality disorder had higher levels of psychopathology than did offspring of fathers with substance dependence without antisocial personality disorder and a comparison offspring group. Neither of these studies directly examined the relationship between parent and child on corresponding mental disorders.
The aim of this study was to determine the extent to which parental substance use disorder and other mental disorders were associated with offspring psychopathology. The hypothesis was that the strongest predictors of specific mental disorders in offspring would be the corresponding disorders in the parents. Study methodological features included 1) direct assessment of all fathers, mothers, and children; 2) assessment of childhood conduct disorder and ADHD in parents as well as offspring; 3) inclusion only of children in developmental periods before the onset of substance use disorders; and 4) a sufficiently large sample to comprehensively examine these relationships with mixed-effects ordinal regression.
Method
Participants
Children (N=1,167) from 613 families were recruited through their biological fathers. Recruitment occurred through multiple sources, including substance abuse and other psychiatric treatment programs, social service agencies, newspaper and radio advertisements, and a sampling frame purchased from a marketing firm. Written informed consent was obtained from fathers and mothers, and assent was obtained from minor children. The study was approved by the University Human Subjects Institutional Review Board.
Families were classified into two groups on the basis of paternal substance use disorder history: 1) high-risk families were those in which the father had a substance use disorder (N=294); 2) low-risk families were those in which the father had no substance use disorder (N=319). Fathers were considered to have a substance use disorder if they ever met DSM-III-R criteria for abuse or dependence involving substances other than nicotine, caffeine, or alcohol. Other mental disorders and the latter substance use disorders were not exclusionary criteria for the high-risk group. The fathers in the low-risk group had never met DSM-III-R criteria for any substance use disorder or any other major adulthood axis I mental disorder. (This sample includes additional families and sibling data not reported in prior reports [
1,
19].)
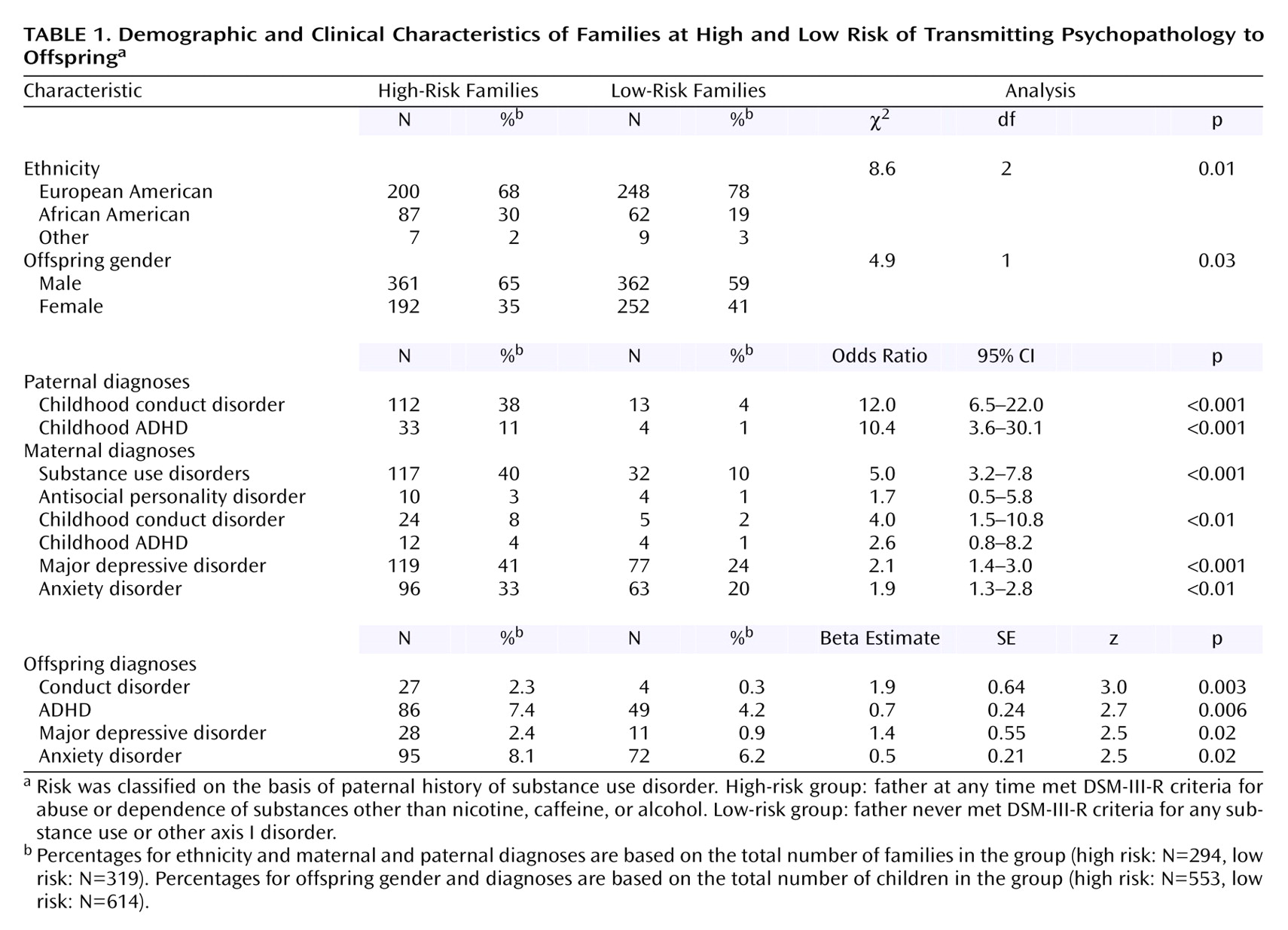
A comparison of the high-risk and low-risk groups in terms of demographic variables is presented in
Table 1. According to the Hollingshead two-factor index
(20), calculated as a continuous variable, high-risk families had lower socioeconomic status (mean=36.4, SD=12.3) than did low-risk families (mean=44.1, SD=13.8) (t=7.3, df=610, p<0.001). High-risk families also had slightly younger offspring (mean=10.7 [SD=2.0] versus 10.9 [SD=2.0]; t=2.1, df=1165, p=0.04) and, as seen in
Table 1, a lower proportion of European American parents and a higher proportion of male offspring. Subsequent analyses controlled for these characteristics. The numbers of offspring per family were as follows: one offspring (N=187 families); two (N=241); three (N=154); four (N=27); five (N=4). High-risk and low-risk groups did not differ on this variable (likelihood ratio=8.6, df=4, p=0.08).
Diagnostic Instruments
Diagnoses were made according to DSM-III-R, the most recent DSM edition when the study was initiated. For children and parents, information concerning substance use disorder was gathered by a semistructured interview developed for this project
(21), which included questions from the Structured Clinical Interview for DSM-III-R (SCID)
(22). For parents, other mental disorders were also assessed with the SCID. For children, other mental disorders were assessed with the Schedule for Affective Disorders and Schizophrenia for School-Age Children (K-SADS)
(23). Diagnoses were determined in a consensus conference by using the best-estimate diagnostic procedure
(24). Descriptions of rater training and interrater reliabilities may be found in prior publications
(1,
25).
Data Analyses
Parental psychopathology and demographic characteristics were examined in relationship to four offspring psychopathology variables: 1) conduct disorder, 2) ADHD, 3) major depressive disorder, and 4) anxiety disorders. Conventional statistics assume that each subject or “observation” is independent of other observations. This assumption is violated in studies where multiple children from a family are included, typically increasing type II error. Data with this structure are described as nested with children grouped or nested within families. Hedeker and Gibbons
(26) have developed statistical software applicable to testing hypotheses with dichotomous response variables and nested data using mixed-effects ordinal regression (MIXOR: http://tigger.uic.edu/~hedeker/mix.html). Using this procedure, family clusters of offspring mental disorders were examined by intraclass correlation coefficients (ICC). For each of the four aforementioned mental disorders, univariate and multivariate models were examined. In the univariate models, mixed-effects ordinal regression (MIXOR) models examined relationships between each individual parent mental disorder and each of the four child psychopathology variables, with family cluster and demographic variables included as covariates. For sex, female was coded 1, and male was coded 2. Note that there were an insufficient number of cases in the ethnic category “other” for these subjects to be considered as an independent group, and therefore ethnic group was summarized as a two-class variable (i.e., white=1, other=2). Socioeconomic status was included as a continuous variable. To control type I error, a Bonferroni-corrected significance level of 0.008 (0.05/6 diagnoses for each parent) was used in interpreting these univariate analyses. A multivariate MIXOR model was constructed for each offspring mental disorder by first including all paternal and maternal mental disorders and proceeding by backward elimination until only parental mental disorders with statistically significant relationships with the child outcome variable remained.
Results
Fathers in high-risk families were defined by the presence of a substance use disorder history and were characterized by high rates of antisocial personality disorder (N=73, 25%), major depressive disorder (N=85, 29%), and anxiety disorders (N=63, 21%). Among fathers in low-risk families, substance use disorder and other adulthood mental disorders were absent by definition. Other parent mental disorders in high-risk and low-risk groups were compared with standard logistic regression, with socioeconomic status, age, ethnic group, and sex included as covariates (
Table 1). High-risk fathers, compared with low-risk fathers, had higher rates of childhood conduct disorder and ADHD. Compared with low-risk mothers, high-risk mothers were characterized by higher rates of substance use disorders, conduct disorder, major depressive disorder, and anxiety disorders. Mental disorders of offspring in the high-risk and low-risk groups were compared by using MIXOR, with family cluster, socioeconomic status, age, ethnic group, and sex included as covariates. Offspring conduct disorder, ADHD, major depressive disorder, and anxiety disorders were all significantly more common in the high-risk group than in the low-risk group.
Among children, three combinations of mental disorders were present in more than one or two cases. ADHD and conduct disorder comorbidity was present in 13 high-risk children (2.4%) and one (0.2%) low-risk child. Anxiety disorder and major depressive disorder comorbidity was present in 13 high-risk children (2.4%) and six (1.0%) low-risk children. ADHD and anxiety disorder comorbidity was present in 20 high-risk children (3.6%) and five (0.8%) low-risk children. For each of these comorbid conditions, the MIXOR statistical procedures failed to converge for the comparison of the high-risk and low-risk groups with family cluster and demographic variables as covariates. This indicated that the sample size in this context was insufficient to examine other models.
Father-Mother Psychopathology Associations
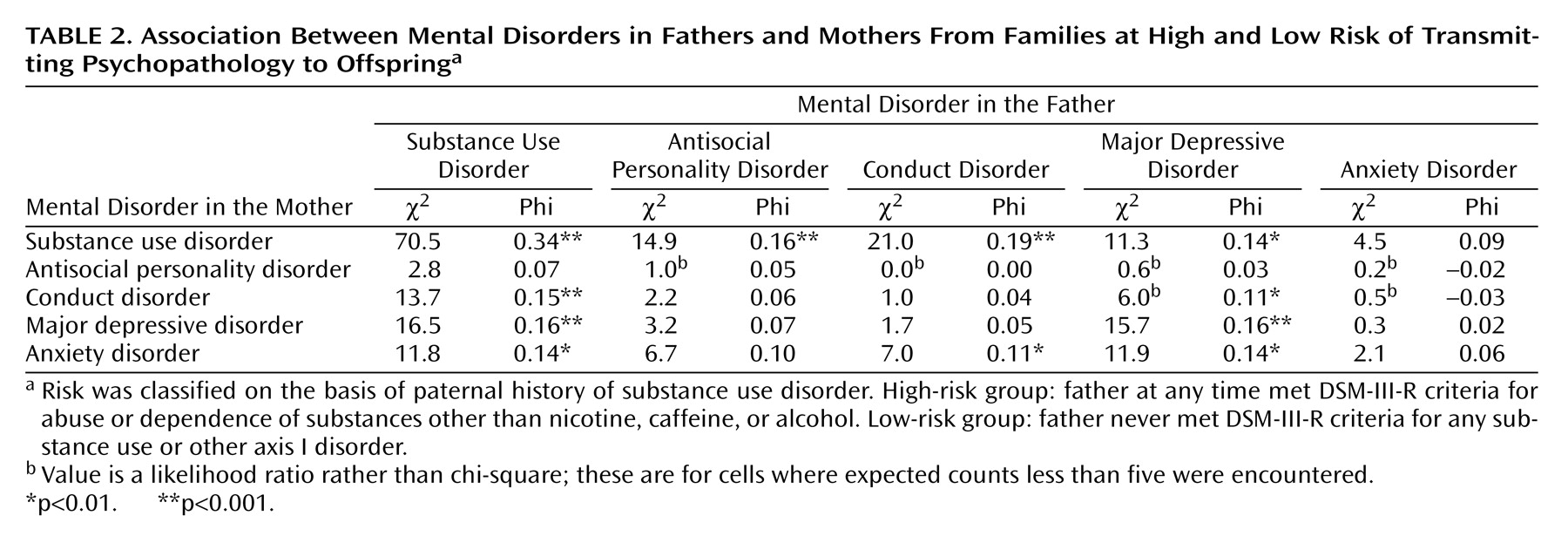
The statistical associations between father and mother on substance use disorders and their other mental disorders are presented in
Table 2. The associations between mother and fathers on mental disorders were determined by phi coefficients with Bonferroni correction for multiple tests (0.05/5=0.01). The strongest statistical relationship was between substance use disorders in the father and substance use disorders in the mother. Substance use disorder in the father was also significantly associated with conduct disorder, major depressive disorder, and anxiety disorders in the mother. Substance use disorder in the mother was significantly associated with antisocial personality disorder, conduct disorder, and major depressive disorder in the father. Major depressive disorder in the father was significantly associated with conduct disorder, major depressive disorder, and anxiety disorders in the mother. Conduct disorder in the father was significantly associated with anxiety disorders in the mother.
Parent-Child Psychopathology Associations
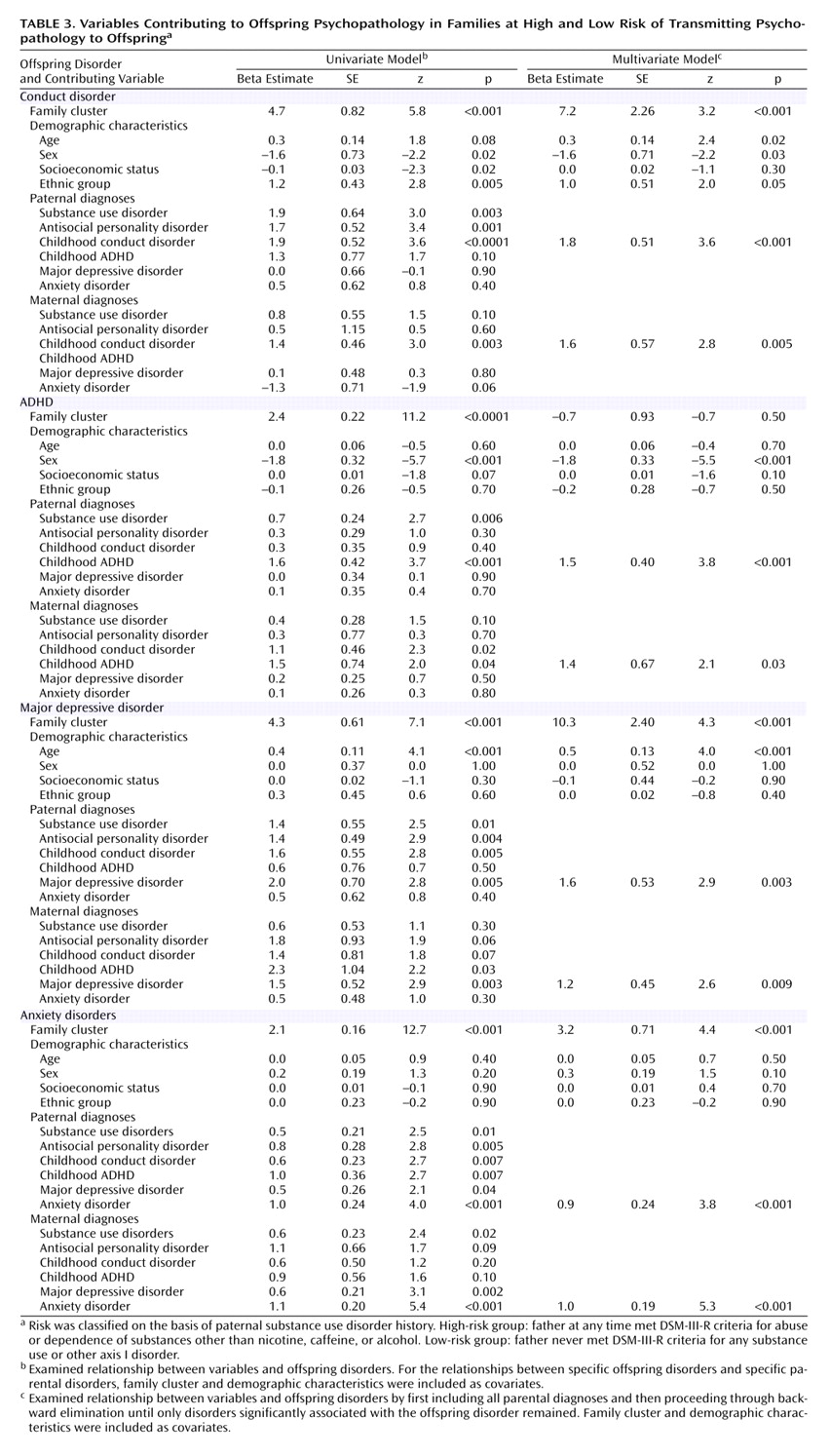
The univariate statistical associations for relationships between mental disorders in individual parents and offspring mental disorders are presented on the left in
Table 3. A multivariate MIXOR statistical model was developed for each offspring mental disorder, with the aforementioned backward elimination procedure used to develop a parsimonious model. The final models are presented on the right in
Table 3. All models included family cluster, socioeconomic status, offspring age, ethnic group, and sex as covariates.
Offspring conduct disorder clustered in families (ICC=0.45, p<0.001) and was significantly more common in male offspring. For offspring conduct disorder, significant univariate associations were noted for substance use disorders, antisocial personality disorder, and conduct disorder in the father as well as conduct disorder in the mother. The final multivariate model for offspring conduct disorder included only conduct disorder in the father and conduct disorder in the mother. In other words, after family cluster was controlled, socioeconomic status, age, sex, and conduct disorder in both the father and mother, parental substance use disorders and other mental disorders were not significantly associated with offspring conduct disorder.
Offspring ADHD clustered in families (ICC=0.26, p<0.001) and was also more common among male offspring. For offspring ADHD, significant associations were noted for substance use disorders and ADHD in the father. The final multivariate model for offspring ADHD included only ADHD in the father and ADHD in the mother.
Offspring major depressive disorder clustered in families (ICC=0.41, p<0.001) but was not significantly associated with gender. For offspring major depressive disorder, significant univariate associations were noted for antisocial personality disorder, major depressive disorder, and conduct disorder in the father as well as major depressive disorder in the mother. The final multivariate model for offspring major depressive disorder included only major depressive disorder in the father and major depressive disorder in the mother.
Offspring anxiety disorders clustered in families (ICC=0.20, p<0.001) and were not significantly associated with gender. For offspring anxiety disorders, significant univariate associations were noted for anxiety disorders, antisocial personality disorder, conduct disorder, and ADHD in the father as well as anxiety disorders and major depressive disorder in the mother. The final multivariate model for offspring anxiety disorders included only anxiety disorders in the mother and anxiety disorders in the father.
Discussion
These results provide evidence consistent with disorder-specific risk transmission for psychopathology from parent to child. For each offspring mental disorder—which here included conduct disorder, ADHD, major depressive disorder, and anxiety disorders—the corresponding diagnoses in mother and father were the only parent mental disorders significantly contributing to each MIXOR model. After considering like mental disorders and demographic variables, parent substance use disorders did not significantly contribute to explaining offspring psychopathology. Studies using other types of populations and alternate study designs have similarly indicated specificity of familial aggregation for antisocial behavior
(27), anxiety disorders
(11,
12), and mood disorders
(28,
29), as well as substance use disorders
(12). The results presented here incorporate several notable methodological refinements relative to previous studies on the transmission of psychopathology from parent to child in high-risk families and provide further evidence for disorder-specific transmission.
The genetic and environmental mechanisms through which paternal psychopathology and substance use disorders influence offspring outcomes have yet to be fully determined. Cadoret and colleagues
(27) provided evidence for a genetic pathway leading from parental antisocial behavior to childhood antisocial behavior in offspring. The finding here that the parents’ childhood antisocial psychopathology phenotype was more predictive of the analogous offspring characteristics than the parents’ adulthood phenotype suggests nonenvironmental transmission consistent with a genetic hypothesis. Parent characteristics also constitute environmental influences
(30).
The study has several limitations. Retrospective assessments of childhood and adolescent periods collected in adult samples (i.e., parents) may be influenced by recall bias. Parental perceptions of child behavior may also be influenced by parental psychopathology
(31,
32). The extent to which the children in the high-risk and low-risk families are representative of their populations was also not tested by this study, and replications of these findings will be needed with samples acquired by other methods. The characteristics of high-risk families present challenges to the accrual of the substantial samples with participation of both parents. In this sample, the numbers of subjects with specific combinations of comorbid mental disorders were insufficient for investigation with MIXOR. Further exploration of parent-child transmission of comorbid conditions may be feasible with larger samples or study designs focusing on this issue.
The statistical associations demonstrated in this study are necessary but not sufficient for inferring causal relationships
(33). Nevertheless, studies utilizing observational data may suggest likely causal models
(17,
34). While these results do not lend themselves to a definitive causal interpretation, the findings are sufficiently compelling to inform hypotheses for further study.
Improved methods for identifying high-risk children are needed. Among parents with substance use disorders, parents with psychopathology may be more likely to have offspring with corresponding psychopathology. This relationship may refine the identification of children at risk for mental disorders and later substance use disorders
(35–
37). Programs designed to avert substance use disorders likely need to focus on the prevention and treatment of childhood mental disorders to disrupt the link between childhood mental disorders and substance use initiation (
(38,
39)). This demonstration of the specific transmission of psychopathology risk from parent to child may further refine the identification of children who may benefit from preventive interventions.