The number of enrollees in managed mental health care plans has increased dramatically during the last decade. By 2000, more than 78% of Americans who had private or public health insurance were enrolled in some type of managed health care plan. The penetration of managed care into the U.S. health care system will continue because virtually every state is planning to implement managed care for persons served by the public mental health care system
(1,
2) and because private insurers seek to carve out their mental health care services
(3). One of the most controversial components of managed care is utilization management. “Utilization management” describes a set of techniques used to limit the provision of health care services
(4). Among the techniques typically used are utilization review
(5,
6), treatment algorithms, formulary restrictions
(7), and limitations on referrals to physicians and hospitals
(8).
These utilization management techniques have had a considerable impact on mental health treatment. For example, examination of data from the National Ambulatory Medical Care Survey indicated that visits to office-based psychiatric services have become shorter and that the proportion of visits that were 10 minutes or less in length has increased
(9). Also, in one study of mental health managed care, it was shown that patients were receiving fewer outpatient sessions, had less frequent inpatient admissions, and experienced shorter lengths of stay
(10).
Over the past decade, clinician perception has been that utilization management has contributed to this reduction in frequency, number, and length of mental health treatment visits and has influenced clinician decision making in the mental health setting
(8–
10). These perceptions are supported by data from two large national surveys that showed that psychiatrists are spending more time at work and seeing greater numbers of patients per week but that a larger proportion of their time was diverted from direct patient care to attend to administrative and other activities
(11).
However, there are few sources of data that permit a careful examination of whether these utilization management techniques have changed the treatments that psychiatrists would optimally like to provide. Therefore, the specific aim of this study was to use a recent survey that provides nationally representative information on U.S. psychiatrists and their patients to examine the relationship between utilization management techniques and associated changes in psychiatrists’ treatment decisions.
Method
This study used data from the American Psychiatric Institute for Research and Education Practice Research Network’s study of psychiatric patients and treatments, which in 1999 administered a mailed survey to a rotating cohort of 784 APA member psychiatrists. Demographic and practice data were collected from 615 psychiatrist members of APA who spent at least 15 hours per week providing direct face-to-face patient care (response rate=78.4%). The sample consisted of 291 responding psychiatrists selected at random from the APA membership list and 324 self-identified volunteers who responded to announcements placed in a national publication mailed to APA members. Sample weights were developed to generate nationally representative estimates and to account for the sampling design, nonresponse, and random/volunteer status.
Participating psychiatrists completed a patient log reporting general information on the first 12 consecutive unique patients seen after an assigned start time. Detailed information was collected on every fourth patient in the log (up to three patients total). The survey collected data on demographics, diagnostic information, clinical information, treatment settings, medications, treatment characteristics, financial arrangements, and utilization management and quality assurance for 1,843 patients. The survey methods and weights are described in detail by West et al.
(12) and Pincus et al.
(13).
Utilization Management Techniques
The primary independent variables for this study were responses to a question from the detailed diagnostic and treatment form that directly addressed the issue of utilization management and quality assurance techniques: “Are your treatment recommendations for this patient subject to any of the following utilization management or quality assurance techniques?” Response choices were the following:
1.
Utilization review (e.g., precertification, concurrent review, referral authorizations, administrative or utilization case management)
2.
Incentives or requirements to use specific practice guidelines or treatment algorithms
3.
Restrictions on or specification of the medications that can be prescribed (e.g., a formulary)
4.
Financial incentives or penalties to limit referrals
5.
Referrals limited to selected hospital or specialist panels
Changes in Psychiatric Treatment
The dependent variables for this study were created from responses to a question that addressed the issue of psychiatrist treatment changes: “Have financial considerations (e.g., managed care limitations, patient’s resources, or limitations of a public system) resulted in any of the following for this patient?” Response choices were the following:
Reducing the frequency of visits you would optimally like to provide
1.
Reducing the number of visits you would optimally like to provide
2.
Providing a different form of treatment than you would optimally like to provide (e.g., substituting outpatient for inpatient care or providing group rather than individual psychotherapy)
3.
Selecting or switching to a different medication than you would prefer
Responses 1 and 2 were collapsed to create the variable “reducing the frequency and/or number of visits” because both reflected overall reduced clinical time spent by the psychiatrist with each patient. Similarly, responses 3 and 4 were combined to create the variable “providing different treatment,” which was inclusive of changes in care provided at each psychiatrist-patient encounter.
Data Analysis
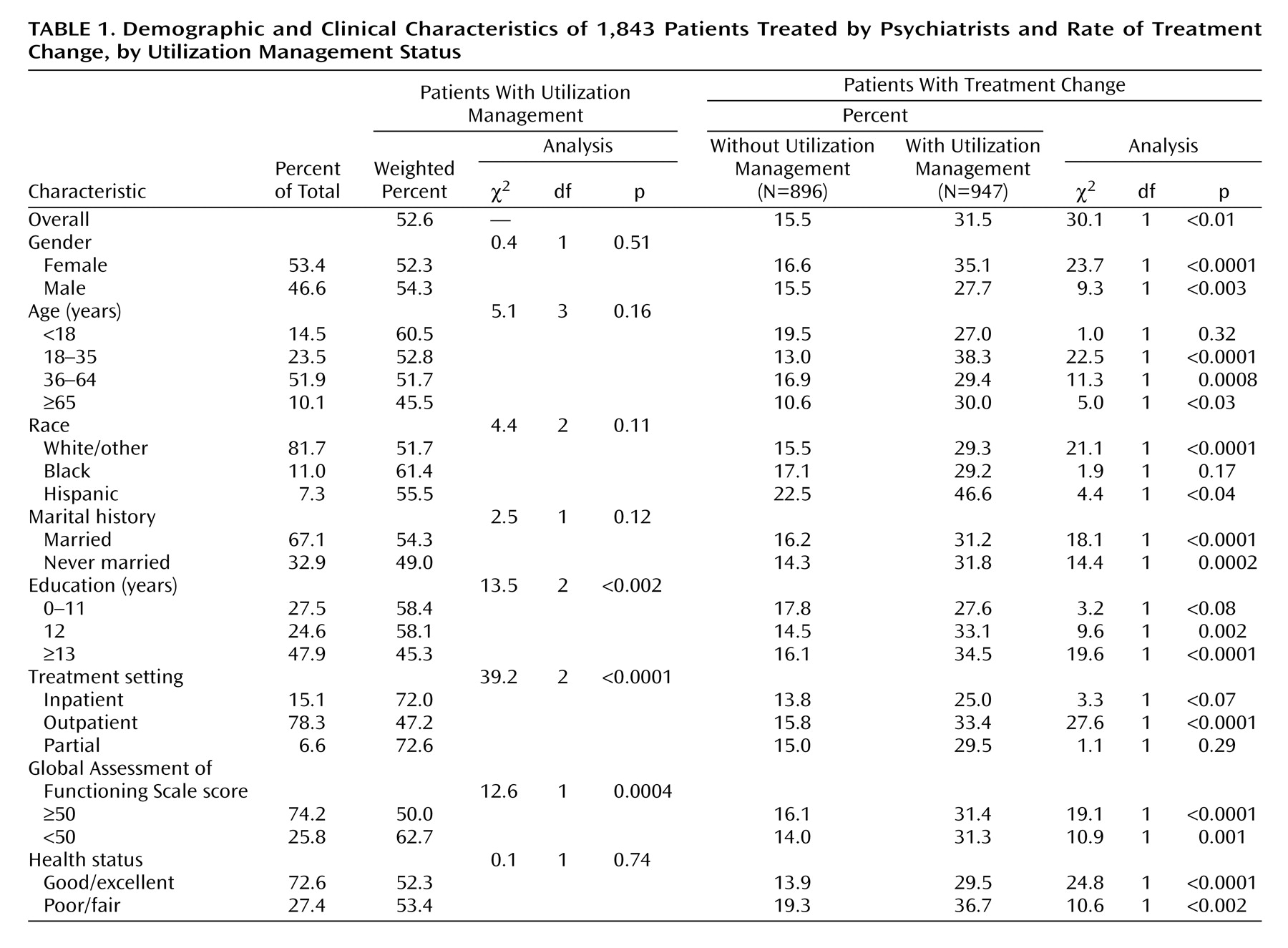
Weighted percentages of all study variables were calculated along with Wald chi-square tests of significance to examine differences in the rates of utilization management by patient characteristics. We further examined the rates of treatment change among those with and without utilization management techniques applied to their care (
Table 1). The patient characteristics included in
Table 1 were chosen because of previous research with this nationally based study group. For example, an association has been shown among psychiatric patient characteristics and health plan characteristics and having financial considerations affect optimal treatment provision as perceived by the psychiatrist
(12). Similarly, past analyses of the 1997 data from the same survey revealed significant differences by locus of care for each demographic characteristic examined, along with observed differences in health plan, source of payment, and psychiatrist reimbursement mechanisms
(13). We calculated among all patients (N=1,843) the number and percentage of patients subjected to each utilization management technique, along with the number and percentage of patients for whom each change in treatment occurred.
To examine the relative influence of specific utilization management techniques (independent variables) on physician treatment plans (dependent variables), adjusted odds ratios from separate logistic regression models were computed, including all utilization management techniques and significant demographic, clinical, and setting characteristics from
Table 1. An association between formulary restrictions and a reduced frequency and/or number of visits was not calculated because it made no sense to do so.
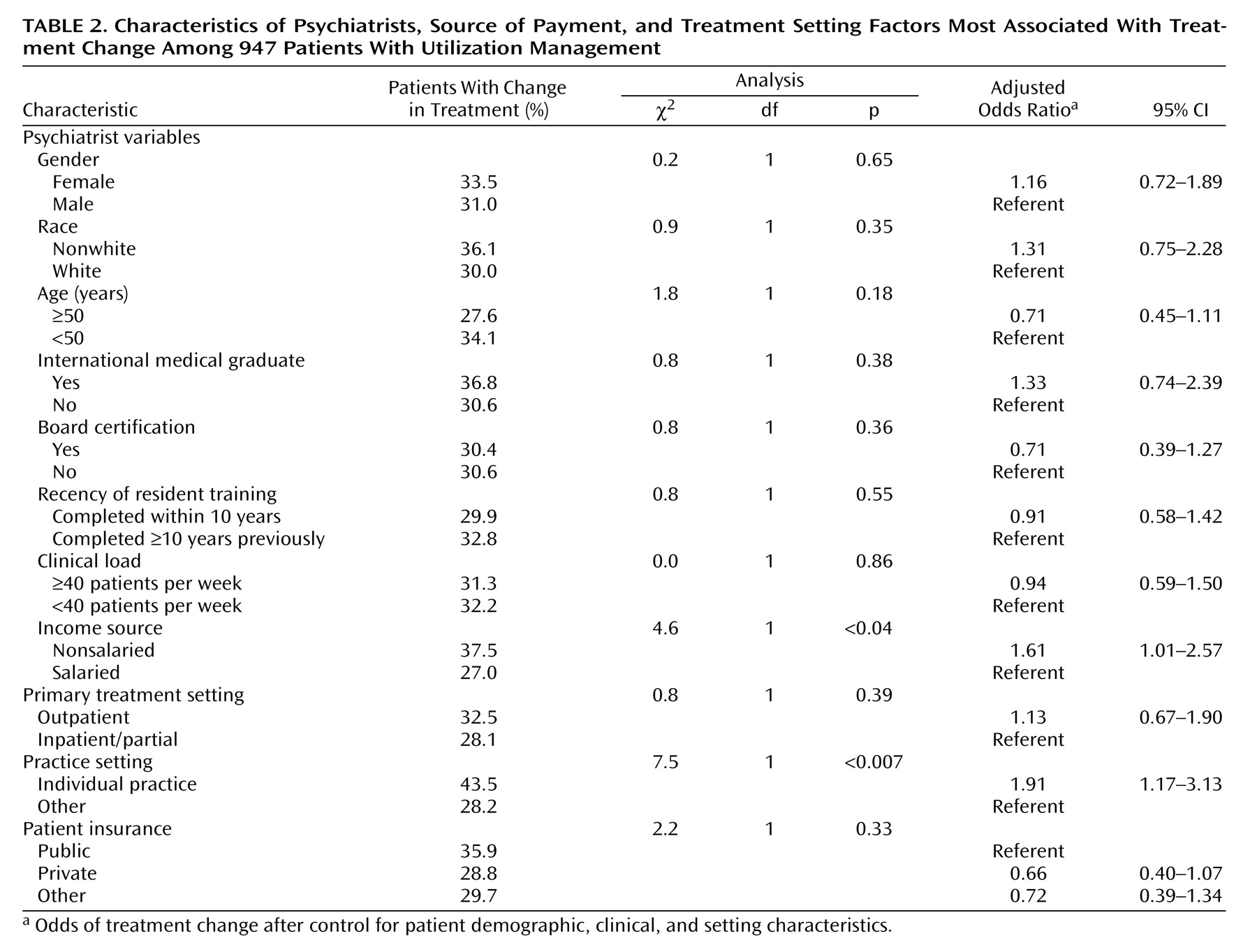
We then examined the association between psychiatrist and delivery factors of the treatment system (psychiatrists’ characteristics, source of payment, treatment setting) and treatment modifications among those with any utilization management (
Table 2). Adjusted odds ratios were computed (along with corresponding Wald F tests of significance and p values) with a logistic regression model with “any treatment modification” as the dependent variable and including all psychiatrist and treatment delivery system characteristics as the independent variables, presented in
Table 2, with control for any other significant patient characteristics (p≤0.10 from
Table 1). All analyses used the SUDAAN statistical package to account for the sampling weights and the complex sampling design of the study.
Results
The patient sample (N=1,843) was almost equally split by gender, predominantly white, and either currently or formerly married. Overall, most patients were being treated in an outpatient setting. Patients for whom utilization management techniques were in effect were less educated, had relatively more inpatient care, and received lower Global Assessment of Functioning scale scores (axis V) than patients whose care was not subject to utilization management (
Table 1).
Frequency distributions were calculated to determine the proportion of patients whose care was subject to any utilization management technique. Nine hundred forty-seven (52.6%) of the patients had utilization management applied to their care (
Table 1), of whom 309 (31.5%) had associated changes in treatment provisions reported by their psychiatrists because of financial considerations. Among those with no utilization management, only 15.5% had associated changes in treatment.
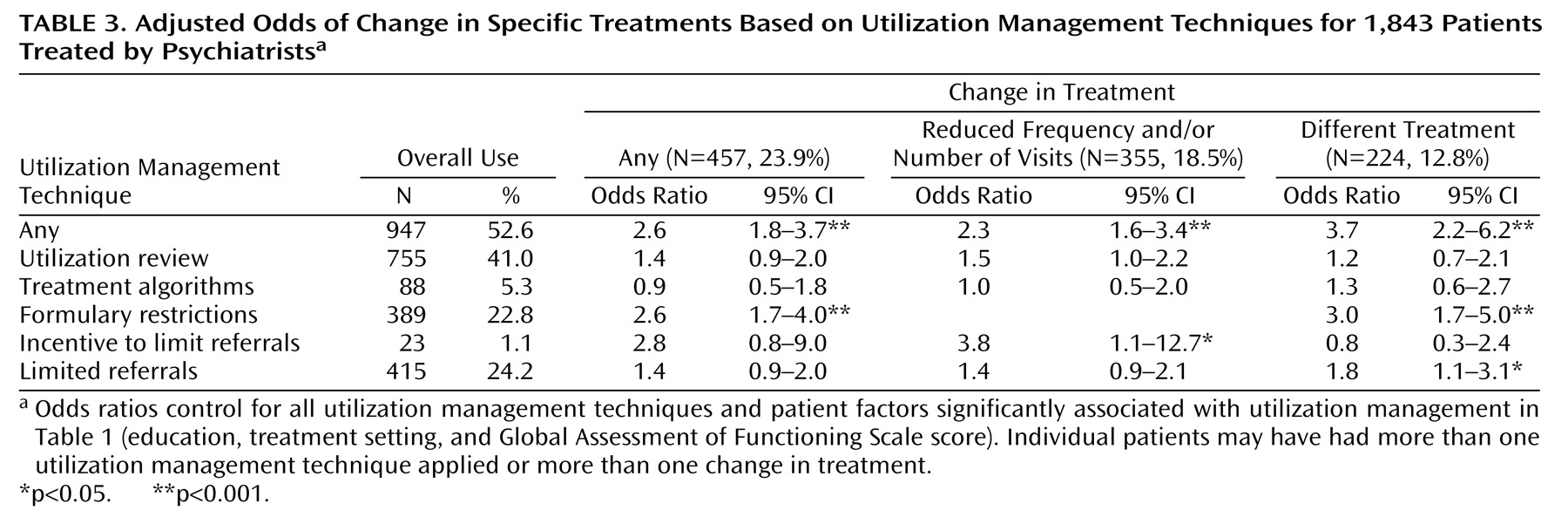
The overall odds ratio of a change in treatment when any utilization management technique was present was 2.6 (
Table 3). The odds of reducing the frequency and/or number of visits and the odds of providing different treatment when any utilization management technique was present were 2.3 and 3.7, respectively.
Table 3 also presents the odds ratios for changes in treatment in the presence of different utilization management techniques. The presence of utilization review or treatment algorithms was not associated with psychiatrists’ reported changes in treatment. In contrast, the three remaining utilization management techniques had significant associations with treatment modifications. For example, the presence of formulary restrictions was associated with a threefold increase in the odds of a physician providing different treatment. Although only 1% of the patient group had treatment recommendations restricted by financial incentives or penalties to limit referrals, when present, these techniques were associated with an increased odds of reducing the frequency or number of visits the psychiatrist would have preferred by a factor of almost four. When treatment recommendations were restricted by limiting referrals to selected hospitals or specialist panels, there was a significant increase in the odds of the psychiatrist providing different treatment than he or she otherwise would have provided.
Two psychiatrist characteristics were associated with the likelihood of modifying treatment (
Table 2). Psychiatrists who were compensated by a nonsalaried income source were 1.61 times more likely to modify their treatment plans when caring for patients under any form of utilization management, relative to psychiatrists with a salaried income source (with control for other significant patient and clinician factors). Similarly, clinicians in individual practice settings were 1.9 times more likely to change their treatment plans than clinicians in other settings.
Discussion
More than half of the patients in a nationally representative sample of psychiatric patients were receiving care that was subject to one or more utilization management techniques. Patients treated under utilization management were significantly more likely to receive a different treatment or less intensive treatment than the patients who were not treated under utilization management. Approximately one-third of these patients received a different form of treatment than their psychiatrist would optimally have liked to provide, compared to 15.5% of the patients who were not treated under utilization management. It is notable that the utilization management methods found to have the greatest association with changes in treatment were those that have financial implications: formulary restrictions, incentives to limit referrals, and limits in referrals to hospitals and specialty panels. In contrast, there was no statistical association between utilization review or treatment algorithms and psychiatrists’ reported changes in treatment provisions. Although the application of treatment algorithms is still uncommon, utilization review is commonly used in managed care. There may be two reasons for this absence of statistical significance. It is possible that psychiatrists are acting as effective advocates for their patients and have become increasingly sophisticated in requesting authorization for continued care, thereby reducing the actual impact of utilization review. Alternatively, the confidence interval of the 40% increase in the odds of treatment change in the presence of utilization review suggests that this relationship might be significant with a larger sample size. An even greater effect size was found in the association between utilization review and reducing the frequency and/or number of visits.
Two psychiatrist characteristics were associated with treatment changes. Psychiatrists in individual practice were significantly more likely to change their treatment plans relative to the psychiatrists practicing in other settings. Physicians who practice in settings other than individual practice may be more removed from the utilization management process and decisions than physicians in solo practice (e.g., a nurse or other member of the staff may be more likely to coordinate utilization management review processes). Practicing with others may provide greater bargaining power when dealing with managed care organizations that implement utilization management. Alternatively, psychiatrists in group or other nonindividual settings may be practicing in a manner that is already more consonant with managed care guidelines and may thus have less need to alter their treatment plans in response to utilization management. Similarly, psychiatrists receiving a source of income other than salary were more likely to reflect an association between treatment modifications and utilization management techniques. This is a logical association because salary is generally considered fixed and independent of either productivity or profit, whereas other types of income are often tied to the generation of income or to practice behaviors. The latter are more characteristic of a practice environment influenced by managed care techniques.
A significant association was found between the presence of formulary restrictions and the provision of different treatment. In evaluating this association, it is important to consider whether this change in psychiatrist behavior is good or bad for patient care. There is a growing body of literature addressing the influence of formulary restrictions on clinical outcomes. Randomized clinical trials have repeatedly shown that there are no significant differences in clinical effectiveness among individual selective serotonin reuptake inhibitors (SSRIs) or between SSRIs and other classes of antidepressants in the treatment of depression in outpatient settings
(14–
16). The fact that SSRI drugs are equally effective on average, however, does not mean that they are equally effective for individual patients
(17). Previous research has shown that among patients who do not respond to one SSRI antidepressant, at least half will experience benefit from another drug in the same class
(18,
19). Based on the conclusions of these studies, it would not be unreasonable to restrict formularies for the first-line treatment of depression in an outpatient setting. The restriction of other antidepressants for use as second or third-line treatments cannot be similarly supported by the literature. Furthermore, it is useful to specifically study the use of formulary restrictions in actual managed care settings. In one study examining the effect of “single-drug” formulary restrictions on the likelihood of the completion of drug therapy for new patients, it was found that patients from a health maintenance organization (HMO) with a single preferred SSRI (paroxetine) were 80% less likely to complete therapy than were patients from an HMO with two preferred SSRIs (fluoxetine and paroxetine). The formulary effect was found to be independent of the initial drug used to treat the patient
(20). These findings suggest that the use of formulary restrictions may have a substantial impact on the likelihood of patients completing therapy. Undertreated or untreated depression has well-documented adverse effects on the individual as well as on society.
Another significant association was found between the incentive of utilization management techniques to limit referrals and the likelihood of reducing the number or frequency of visits. The question remains whether reduced visits to the psychiatrist actually affect quality of care and in which direction. Although there are no specific evidence-based guidelines that reflect the influence of too few visits on care, it is worth examining some nationally accepted standards. The Health Employer Data and Information Set is used to rate health plans that cover the majority of Americans enrolled in HMOs
(21). One recent study
(22) examined the rates and correlates of mental health care performance measures in the Health Employer Data and Information Set
(22). Among the mental health care quality measures recommended by the Health Employer Data and Information Set and used for HMO “report cards” are 1) ongoing medication treatment in the 6 months after a new depressive episode and 2) optimal practitioner contact as defined by at least three follow-up mental health care visits in the 3 months after a new depressive episode. The mean rate of all mental health care performance measures was found to be significantly lower than for non-mental-health care domains. Worse quality of these domains was also predictive of poor mental health care performance. The findings suggest that commitment of resources to clinical care predicts better mental health care performance for U.S. HMOs. In this context, it is reasonable to consider that fewer visits to a psychiatrist, at least in the case of the treatment of depression, may result in a compromise of optimal care. In the aggregate, it appears that the presence of utilization management techniques is associated with changes in treatment behaviors and that these changes may result in less than optimal care. Clearly, managed care as a whole may have some benefits because it has reduced harmful practices that were common in the era before managed care, such as unnecessary hospitalization, poor follow-up after discharge, and care that was incongruent with practice guidelines. However, the specific utilization management mechanisms described in this study appear, taken together, to be associated with changes in provider treatment behavior that may have led to less than optimal care.
The strengths
(23) and generalizability
(13) of a practice-based research network for observational health services research have been documented in detail elsewhere. Particularly germane to this study is the advantage of capturing data on representative patients receiving representative treatments from psychiatrists with varying clinical backgrounds across the full range of managed and nonmanaged treatment settings. Several limitations should be noted, however. First, in the absence of a randomized design, the observed effects of utilization management may be confounded by other important health plan features, including mental health benefit designs (e.g., mental health coverage levels, copayments, deductibles)
(13). Second, both the utilization management mechanisms and psychiatrist treatment plans are self-reported by the psychiatrist. This leads to the possibility of bias in either of two directions: dissatisfied psychiatrists could overreport changes in treatment plans or, alternatively, social desirability (i.e., not wanting to believe that as physicians they would ever be affected by financial incentives) could keep them from reporting actual changes in treatment. This use of self-report also leads to the possibility that psychiatrists may have misinterpreted survey questions. For instance, they may have understood the phrase “financial considerations” in the dependent measure to either narrowly reflect only their considerations or the broader financial considerations embodied in managed care limitations, the patient’s resources, or limitations of a public system. Third, it would be erroneous to assume that the utilization management techniques included as the independent variable had a causal relationship with identified treatment changes in this sample. We have been careful to describe these relationships as associations. However, despite the limitations inherent in trying to infer what an individual psychiatrist may have been thinking when he or she answered the survey question, the associations do highlight the importance of co-occurrence of psychiatrists’ perceptions of utilization management techniques and changes in treatment.
This study’s findings demonstrate that utilization management has a substantial and significant association with psychiatrists’ treatment patterns. With the goal of ensuring care that is guideline concordant and evidence based while promoting quality of care rather than cost containment
(24), further research will have to examine the link between utilization management techniques, associated psychiatrist treatment changes, and subsequent patient and population outcome.