It is now well established that posttraumatic stress disorder (PTSD) develops in a significant minority of individuals following exposure to a traumatic experience
(1–
3). PTSD, however, is not the only psychiatric condition that may develop in the aftermath of trauma. On the contrary, comorbidity is the norm rather than the exception. Breslau et al.
(4), for example, found that 83% of her PTSD sample met criteria for at least one other psychiatric disorder, compared with 44% of those without PTSD. The National Comorbidity Survey
(3) reported that 88% of men and 79% of women with chronic PTSD met criteria for at least one other psychiatric diagnosis. A comparable Australian study
(2) found that another axis I disorder was present over the past 12 months in 85% of male subjects with PTSD and in 80% of female subjects. In each of those studies, major depression was found to be one of the most prevalent conditions occurring concurrently with PTSD.
Several possible causal pathways may explain this association between PTSD and major depression following traumatic exposure
(5). There is evidence that preexisting major depression may render individuals more vulnerable to PTSD in the aftermath of trauma
(6,
7) and, conversely, the presence of PTSD may increase the risk for first onset of major depression
(3,
6). These findings—that each disorder seems to increase susceptibility for the other—suggest the possibility of a shared vulnerability for both disorders. In support of this hypothesis is the finding that many risk factors—such as a history of depression, event severity, childhood abuse, and female gender—are risk factors for both PTSD and major depression
(1,
8,
9). Taken together, these findings suggest that comorbid PTSD and depression in the aftermath of trauma may best be conceptualized as a single general traumatic stress construct.
If PTSD and depression are, indeed, separate constructs, and exposure to traumatic events independently increases the risk for both, higher rates of depression would be expected in individuals exposed to trauma who did not develop PTSD when compared with individuals with no exposure to trauma. Regrettably, few attempts have been made to systematically examine the psychiatric impact of traumatic events in the absence of PTSD. Several studies of accident victims, however, have reported a high incidence of depression at 12 months posttrauma among individuals with no diagnosis of PTSD
(11,
12). Similarly, Shalev et al.
(13) found that 29% of trauma survivors with major depression did not have comorbid PTSD and concluded that major depression and PTSD may be independent sequelae of traumatic events. This conclusion, however, is at odds with the findings of Breslau and her colleagues
(5,
6). They found that risk for major depression following trauma only increased in the subset of individuals who developed PTSD; depression did not increase in those who were exposed to trauma but did not develop PTSD. Breslau et al. concluded that the data do not support the hypothesis that PTSD and major depression in trauma victims are influenced by separate vulnerabilities
(5).
The purpose of the current study was to investigate these issues in a population of severely injured trauma survivors. Specifically, we aimed to determine predictors of symptom severity and categorical diagnosis for each condition and their combination (PTSD, depression, and comorbid PTSD/depression). If PTSD and depression following trauma are, indeed, different constructs, then their symptom severity and diagnostic group should be a function of differential groups of predictors.
Method
Participants
A total of 363 consecutive admissions to a level 1 trauma service participated in the current study (88% participation rate). Criteria for inclusion were a physical injury requiring hospitalization for greater than 24 hours, age between 18 and 70, and either no brain injury or mild traumatic brain injury
(14). Written consent was obtained from all participants following a description of the study. Of the 363 participants who completed the intake assessment, 337 completed the 3-month follow-up, 307 completed the 12-month follow-up, and 301 completed all three assessments.
The majority of participants were male (75%), and the average age was 36 years (SD=13.43). Participants spent an average of 10.13 days (SD=9.64) in the trauma center, with 31% requiring an intensive care unit (ICU) admission. The majority of injuries were caused by motor vehicle accidents (74%). Slightly over half of the participants (56%) met criteria for a mild traumatic brain injury, and 47% were discharged to a rehabilitation facility (rather than being discharged home). These findings were generally consistent with the total population of admissions to the trauma service for the same time period, suggesting that the current sample was representative.
Assessment of PTSD and Depression
The aim of this study was to explore the relationship between PTSD, depression, and comorbid PTSD/depression, with the interest being more on distinct or overlapping constructs than on the presence or absence of a diagnosis per se. Thus, a decision was taken to include subsyndromal PTSD and minor depression. This overcame the potential problem caused by individuals meeting criteria for PTSD who also had significantly elevated depression levels but did not meet diagnostic criteria for major depression. By including minor depression, these participants were classified in the comorbid category rather than the PTSD only group.
PTSD was diagnosed by using the Clinician-Administered PTSD Scale for DSM-IV
(15), one of the most widely used structured clinical interviews for diagnosing PTSD
(16). Participants were deemed to have subsyndromal PTSD if they met criteria for the reexperiencing symptom cluster and either the avoidance or arousal symptom clusters. Frequency and intensity scores were summed to obtain a total PTSD severity score.
Depression was diagnosed using the Structured Clinical Interview for DSM-IV (SCID)
(17). Minor depression was defined according to DSM-IV criteria (the presence of either depressed mood or loss of interest and a total of two to four depressive symptoms). Depression severity was obtained using the Beck Depression Inventory
(18), a widely used, 21-item, self-report scale.
Individuals in the comorbid PTSD/depression group met criteria (full or subsyndromal) for both PTSD and depression.
Assessment of Predictor Variables
Variables selected to predict psychopathology in this study were grouped into four categories: trauma characteristics, individual characteristics, cognitive vulnerabilities, and acute stress responses. Trauma characteristics included length of time in hospital, admission to ICU, and discharge destination (rehabilitation facility or home). The severity of an individual’s injuries was measured with the Injury Severity Score
(19), and the presence or absence of a mild traumatic brain injury was noted. Assessment of objective stressor intensity was recorded by using the severity of event scale, which comprises eight items corresponding to major generic stress dimensions
(20).
Individual characteristics included age, gender, and employment status. Problematic pretrauma alcohol use was assessed with the Alcohol Use Disorders Identification Test
(21). Psychiatric history was measured by using a semistructured interview that asked about past diagnosable psychiatric conditions, psychiatric hospital admissions, and past psychiatric treatment. Trauma history was assessed with questions from the PTSD module of the Composite International Diagnostic Interview
(22).
Three posttraumatic cognitive appraisal questions were asked. These assessed perceived control in the hospital (“How much control do you feel you have over what happens to you whilst in hospital?”), anticipated effect of injury (“How much do you think your injuries will affect your life [e.g., work, leisure, relationships] over the next 12 months?”), and anxiety about injury (“How anxious does this—the effect of the injury—make you feel?”). Each of these questions was rated on a 5-point Likert scale.
The acute stress response included measures of reexperiencing, avoidance, and arousal assessed by using the relevant symptom clusters of the Clinician-Administered PTSD Scale. Current dissociation was measured with the Peritraumatic Dissociative Experiences Questionnaire
(23).
Procedure
Initial assessments were conducted in the hospital shortly before discharge (a mean of 8 days postinjury). At the time of assessment, patients were hemodynamically stable, relatively pain free, and a minimum of 24 hours post opioid analgesia.
Participants had follow-up assessments 3 and 12 months postinjury. These assessments were conducted by means of a telephone interview. Two trained mental health clinicians conducted all interviews. Thirty percent of all interviews were audiotaped, with one-third of these being randomly selected for interrater reliability. Agreement on the absence or presence of a Clinician-Administered PTSD Scale diagnosis was 100%, while agreement on the presence/absence of a SCID diagnosis of depression was 98%.
Statistical Analysis
All statistical analyses were conducted with SPSS 11.0 (Chicago, SPSS). Canonical correlation was used to examine the relationship between symptom severity and predictor variables. A canonical correlation analysis creates a pair of weighted sums (canonical variates) from each group of variables that are maximally correlated. Subsequent pairs of canonical variates are also created that are maximally correlated with one another, subject to the condition that they are uncorrelated with earlier canonical variates. In this analysis, if PTSD and depression are separate constructs, predicted by different combinations of predictor variables, it would be expected that two pairs of canonical variates would have substantial correlations. In one pair, PTSD would be expected to load highly onto one variate and the predictors of PTSD onto the corresponding variate. In the other pair, depression should load highly onto one variate and the predictors of depression onto the corresponding variate. However, if PTSD and depression are best represented as a single construct, a single pair of variates should show a substantial correlation, with both loading highly onto one variate in the pair and most of the predictor variables loading highly on the other variate in the pair.
Multinomial logistic regression was used to identify whether diagnostic categories were associated with differential groups of predictors. If PTSD and depression in the aftermath of trauma are, indeed, different constructs, it is reasonable to hypothesize that variables predicting a categorical diagnosis of PTSD would be different from those predicting a categorical diagnosis of depression. In order to examine this hypothesis, the four diagnostic groups (no diagnosis, PTSD alone, depression alone, and comorbid PTSD/depression) were used as a categorical dependent variable in a series of multinomial logistic regression analyses. Multinomial logistic regression was used because the dependent variable (diagnosis) had more than two categories. In examining whether the predictor variables could differentially predict specific diagnoses, a set of comparisons among categories was conducted. First, participants with PTSD, depression, and comorbid PTSD/depression were compared with participants with no diagnosis, with the aim of identifying predictor variables for each diagnosis relative to no diagnosis. The second set of comparisons compared PTSD and depression with comorbid PTSD/depression. Predictor variables aimed to differentiate participants with PTSD from those with comorbid PTSD/depression and to differentiate participants with depression from those with comorbid PTSD/depression. The final comparison was between PTSD and depression, with the aim of identifying predictor variables that would differentiate between individuals with PTSD alone and those with depression alone.
If PTSD and depression are, indeed, independent constructs, and if comorbid PTSD/depression is simply the conjunction of these two diagnoses, then it would be reasonable to expect that 1) PTSD and depression would be predicted by different variables and 2) comorbid PTSD/depression would share predictors with both PTSD and depression. On the other hand, if PTSD and depression in the aftermath of trauma are the same construct, it would be reasonable to expect little difference between the predictors of PTSD, depression, and comorbid PTSD/depression.
In order to reduce the number of predictor variables in the analysis, two backwards elimination multinomial logistic regressions were conducted, one for diagnosis at 3 months and one for diagnosis at 12 months. Backwards elimination allows the removal of variables that fail to make a significant independent contribution to the prediction. Variables with contributions that were significant at a level of 0.10 or less at both time points were removed from the analysis. The 10 predictor variables that remained were used in all subsequent regression analyses.
Discussion
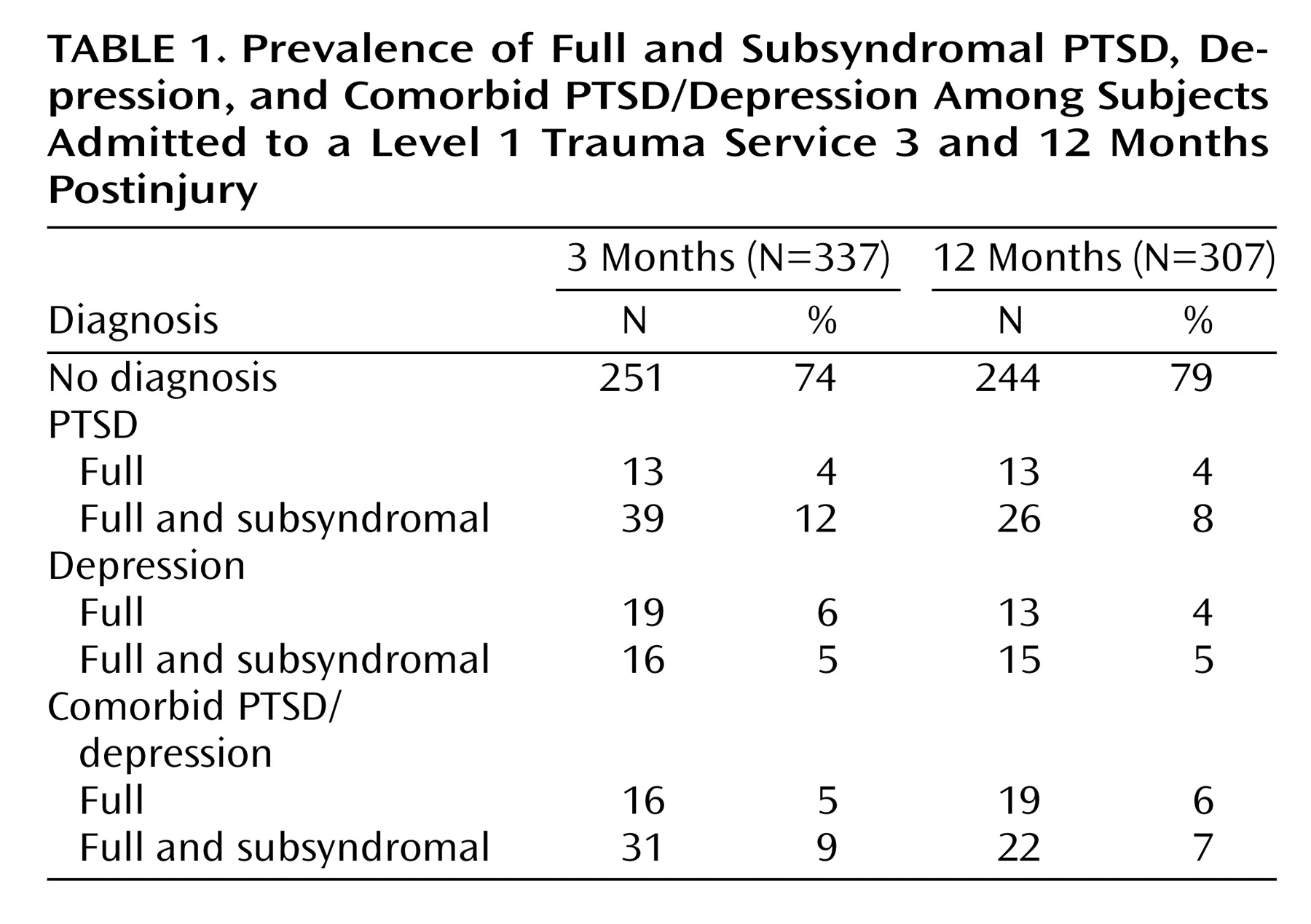
These data shed interesting light on the prevalence between PTSD, depression, and comorbid PTSD and depression in the aftermath of trauma, as well as on the relationships between these constructs. In this population of severely injured trauma survivors, full diagnostic criteria were met in almost equal numbers for each of the three diagnostic categories at 3 months (4%, 6%, and 5%) and 12 months (4%, 4%, and 6%). The addition of subsyndromal cases increased these figures considerably in PTSD (threefold) and comorbid PTSD/depression (twofold), highlighting the importance in both research and clinical settings of considering these cases that do not quite meet full diagnostic criteria.
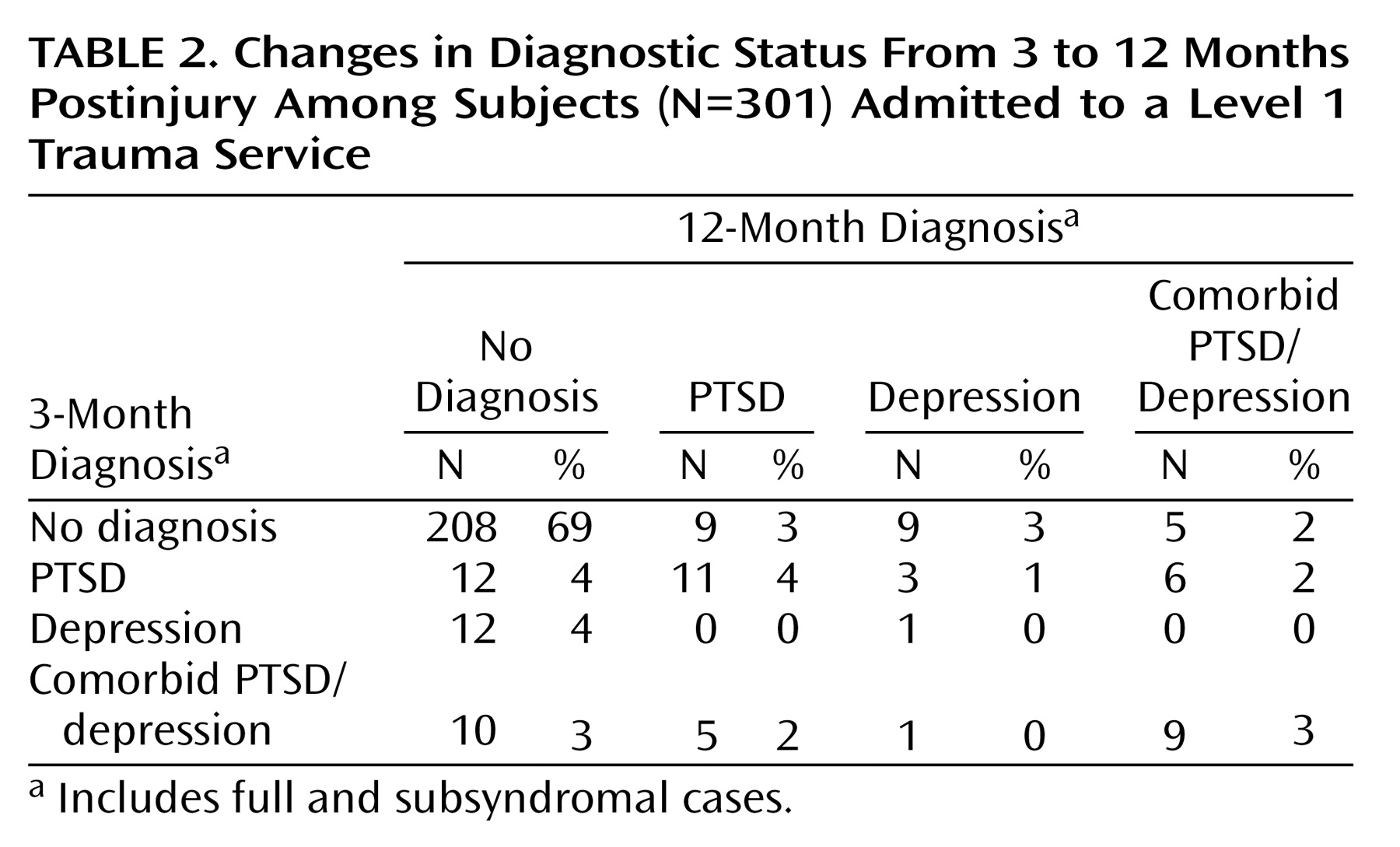
A surprising degree of movement between diagnostic categories was evident from 3 to 12 months postinjury. In particular, the finding that half of those with a diagnosis at both time points changed diagnostic categories between 3 and 12 months highlights the complex interaction and overlap between these diagnoses. The pattern of change across time was similar for the PTSD and comorbid groups, with comparable proportions of participants recovering, maintaining their diagnosis, or changing diagnostic categories. Of importance, however, is that those with depression showed a different pattern: the majority of participants with a single depression diagnosis at 3 months had recovered by 12 months. The group with depression at 12 months comprised mainly individuals with no diagnosis at 3 months. Consistent with findings from subsequent analyses, these data suggest that there may be characteristics about depression at 3 months posttrauma that differentiate it from PTSD and comorbid PTSD/depression. In contrast, the degree of movement between the PTSD and comorbid groups across time suggests a strong similarity and overlapping of constructs.
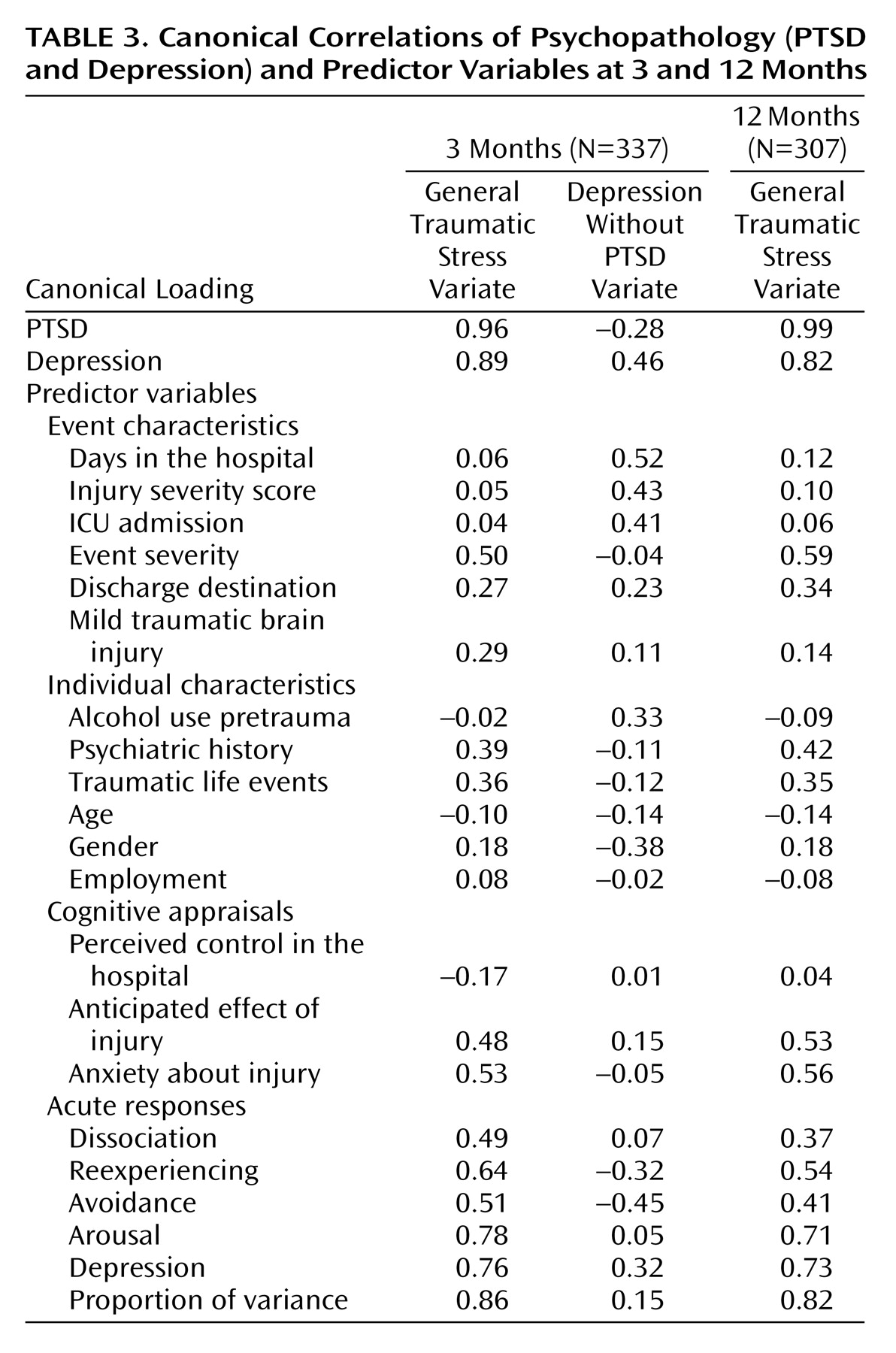
It was apparent from the canonical correlations that most of the variance in psychopathology at both 3 and 12 months postinjury is accounted for by a construct of general traumatic stress within which PTSD and depression are indistinguishable. With the exception of mild traumatic brain injury, the predictors of this general distress are consistent at both time points. They comprise a combination of event characteristics (event severity, discharge destination), individual characteristics (past psychiatric and trauma history), negative cognitive appraisals about the injury and its potential impact, and high levels of PTSD symptoms, depression, and dissociation over the first week posttrauma. However, it appears that at 3 months, depression is differentially related and is predicted by different variables to those that are correlated with more general distress. These predictors, again, include a combination of event characteristics (days in the hospital, Injury Severity Score, ICU admission), individual characteristics (high pretrauma alcohol use, male gender), and acute responses (low levels of reexperiencing and avoidance symptoms coupled with high acute depression). Although explaining only 15% of the variance, this second canonical variate is important, perhaps describing a construct of brief reactive depression that has resolved by the first anniversary of the traumatic event. Certainly, by 12 months, depression as an independent construct had disappeared and only one canonical variate was apparent, characterizing a more general chronic traumatic stress reaction.
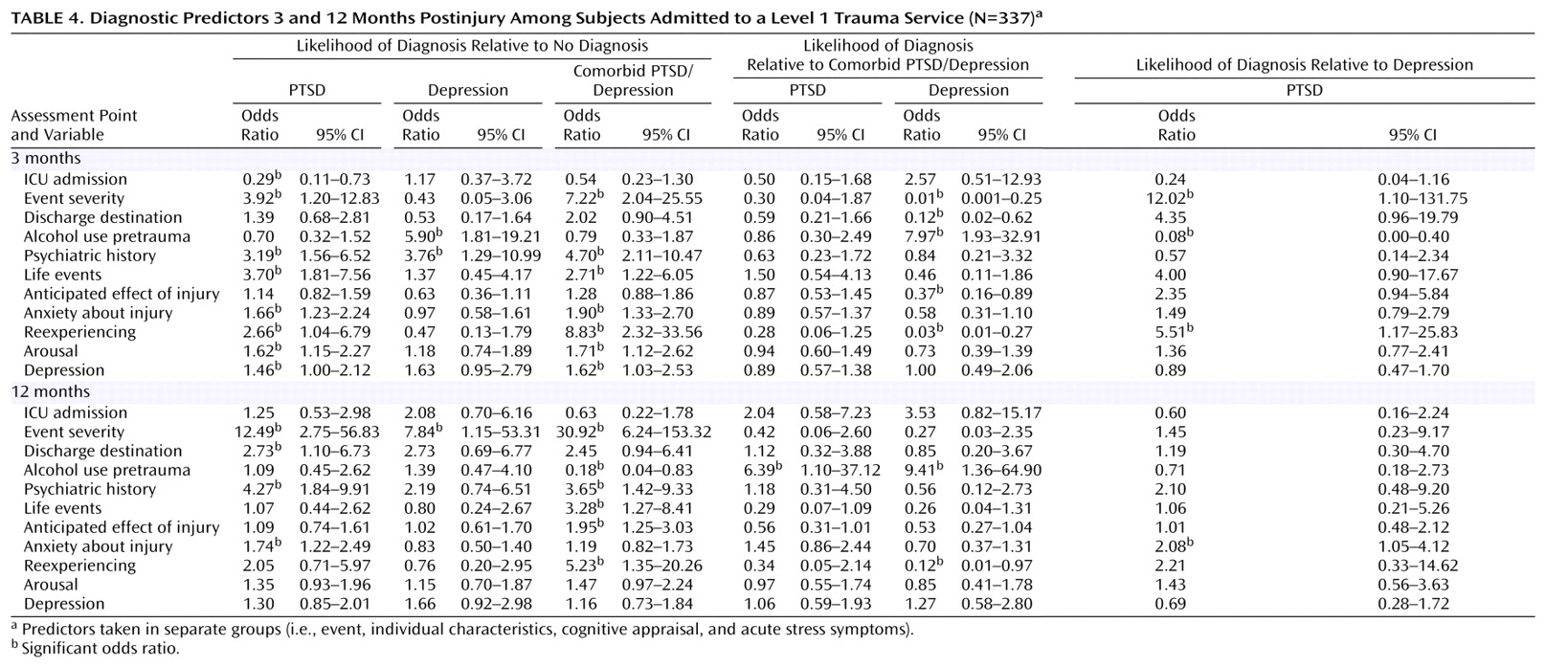
Similar findings were apparent in terms of predicting a categorical diagnosis. At 3 months postinjury, a pattern emerged that was consistent with the canonical correlations. A combination of variables was able to differentiate PTSD alone from no diagnosis, including event characteristics (ICU admission, event severity), individual characteristics (prior psychiatric and trauma history), cognitive appraisals (anxiety about the potential impact of the injury), and acute responses (reexperiencing, arousal, and depression). With the exception of ICU admission, exactly the same combination of variables differentiated between comorbid PTSD/depression and no diagnosis. This suggests that PTSD alone and comorbid PTSD/depression are one and the same construct—akin to the general traumatic stress variate identified in the canonical correlation and largely predicted by the same variables. On the other hand, depression alone was not differentiated from no diagnosis by these predictors; only prior psychiatric history and prior alcohol use were able to differentiate depression alone from no diagnosis. Consistent with these findings, no variables were able to differentiate PTSD alone from comorbid PTSD/depression. Several variables, however, including discharge home (rather than to a rehabilitation facility), prior alcohol use, negative predictions about the effects of injury, and a low level of reexperiencing symptoms, were able to differentiate depression alone from comorbid PTSD/depression. Finally, three variables (event severity, prior alcohol use, and reexperiencing symptoms) were able to differentiate PTSD alone from depression alone.
It is not surprising that the picture at 12 months is somewhat less clear. Although some similarity remains between predictors differentiating between PTSD alone and no diagnosis and between comorbid PTSD/depression and no diagnosis, the pattern is less consistent, and there is little to suggest that depression still exists as a separate construct.
Taken together, these findings generate an intriguing model. First, it is clear that the bulk of psychopathology in the aftermath of trauma is best conceptualized as a general traumatic stress factor. Consistent with the conclusion of Breslau et al.
(5), it would seem that the PTSD and depression symptoms that constitute this factor are part of a shared vulnerability and thus have the same predictive variables. PTSD and comorbid PTSD/depression are effectively one and the same thing. The data suggest that depressive symptoms are often integral to PTSD and that to separate depression out as a distinct disorder when it occurs with PTSD is a somewhat arbitrary distinction. However, there is also evidence to suggest that, in the first few months following trauma, depression may exist as a separate and independent entity, with its own unique set of predictors and its own unique course of recovery with a good prognosis. By 12 months posttrauma, as the psychopathology becomes more chronic, it also becomes less well differentiated and it is no longer possible to identify a unique construct of depression. Rather, all of the psychopathology is best explained by a more general chronic traumatic stress factor that is characterized by mixed PTSD and depressive symptoms.
Such a model has important clinical implications for facilities working with severely injured survivors. Presumably, identification of individuals in the first few months posttrauma who show only depression, in the absence of PTSD symptoms, will facilitate treatment matching. Given their good prognosis, such patients may, for example, be best managed with close monitoring through primary care providers rather than with intensive specialist interventions. The current data suggest that it may even be possible to identify these individuals in the first 10 days posttrauma. On the other hand, individuals presenting at 3 months with clear PTSD symptoms, whether or not depression is also present, may warrant more specialist interventions to modify what is otherwise likely to be a more chronic course. Awareness of issues such as event severity, psychiatric and trauma history, anxiety about the effects of injury, and acute symptoms of reexperiencing, arousal, and depression may facilitate identification of this high-risk group in the first week or so posttrauma.
In reviewing these findings, it is important to exercise caution in concluding that the two conditions are the same or different based solely on the similarities of factors predicting them. While it is the case that identification of different risk factors clearly implies that two conditions are distinct, the opposite is not necessarily true. That is, distinct conditions may share identical risk factors. However, although demonstration of similar correlates is not conclusive, it certainly serves to narrow the focus for future research designed to establish whether the conditions are, in fact, different. A further limitation, as in any longitudinal research, is that some participants were lost to follow-up. Although the number of noncompleters in the current study was small, it nevertheless serves to reduce the sample size at 12 months, with a corresponding impact on statistical power. Finally, caution is warranted in any attempts to generalize these results to other traumatized populations. This injured population has unique characteristics in terms of frequency of traumatic brain injury and the long-term impact of physical injury, which may limit the generalizability of these findings to other traumatized populations. This may particularly be the case for depression given the strong relationship in the current data set between characteristics of the injury (e.g., injury severity, ICU admission, and days in hospital) and subsequent depression. Future studies with larger populations are required before any definitive statements can be made about the structure and relationship between PTSD and depression symptoms following trauma. Nevertheless, these findings are sufficiently strong to warrant greater attention to these complex issues in future posttraumatic stress research.