There are strong indications that depression substantially increases the risk of death in adults, mostly by unnatural causes and cardiovascular disease
(1). In later life, some population-based studies did find this independent relationship
(2–
5), while others did not
(6–
8). There are good reasons to suspect that the relationship between depression and mortality changes in the oldest old. First, because the oldest old are a selection of survivors, depression may have different characteristics compared with the younger elderly
(9). Second, in the presence of many coexisting diseases, depression may not affect mortality in the oldest old. Third, depression in old age was found to be strongly associated with feelings of loneliness
(10), but the effect of loneliness on mortality is obscure. It is unknown whether depression in the fast-growing proportion of oldest old is associated with increased mortality and whether feelings of loneliness play a role in this relationship.
Therefore, we studied the relationship between depression, perceived loneliness, and all-cause mortality, especially examining the potentially distorting effect of perceived loneliness on mortality in the presence of depression.
Method
The Leiden 85-Plus Study
(11) is a prospective population-based study of the oldest old, with characteristics representative of the 85-year-old Dutch population. The study was described in detail elsewhere
(12). In short, since 1997, all members of the 1912-to-1914 birth cohort living in Leiden were enrolled in the month of their 85th birthday. No a priori selection criteria on health, cognitive functioning, or living situation were applied. Annually, medical staff and research nurses conducted structured face-to-face interviews, and blood samples were collected. The medical ethical committee of Leiden University Medical Center approved the study.
Depression was annually measured with the 15-item Geriatric Depression Scale
(13). A score of 4 points or more on the Geriatric Depression Scale was indicative of depression. This cutoff point gave good sensitivity and specificity (0.76 and 0.88, respectively) for the presence of a depressive disorder in a representative sample of the community-dwelling oldest old
(13). Feelings of loneliness, as perceived by the participants, were annually measured by the Loneliness Scale of Tijhuis et al.
(14), an 11-item questionnaire especially developed for use in elderly populations. A score of 3 points or more was indicative for significant perceived loneliness. Because the validity and reliability of the Geriatric Depression Scale and the Loneliness Scale may be reduced in subjects with impaired cognitive function, these questionnaires were restricted to those with a Mini-Mental State Examination (MMSE) score above 18 points.
Survival time (in days) was defined as the period from the 85th birthday until July 1, 2002 (censoring date) or the day of death, as obtained from the community registry. Cardiovascular disease, diabetes, chronic obstructive pulmonary disease, arthritis, malignancy, dementia, Parkinson’s disease, and stroke were assumed present as chronic diseases when either the structured interview with the general practitioner, the results of an ECG, the use of specific medication confirmed from pharmacy registries, or, in case of diabetes, a glucose level of 11.0 mmol/liter or higher so indicated.
Mortality risks and 95% confidence intervals (CIs) were estimated in a Cox proportional hazards model with the annual measurement of depression and perceived loneliness as a time-dependent covariate, with adjustment for control variables. All analyses were performed with SPSS 11 (SPSS, Chicago).
Results
A total of 599 of 705 eligible participants were enrolled (rate of response=87%). There were no significant differences for various sociodemographic characteristics between the 599 participants and the source population
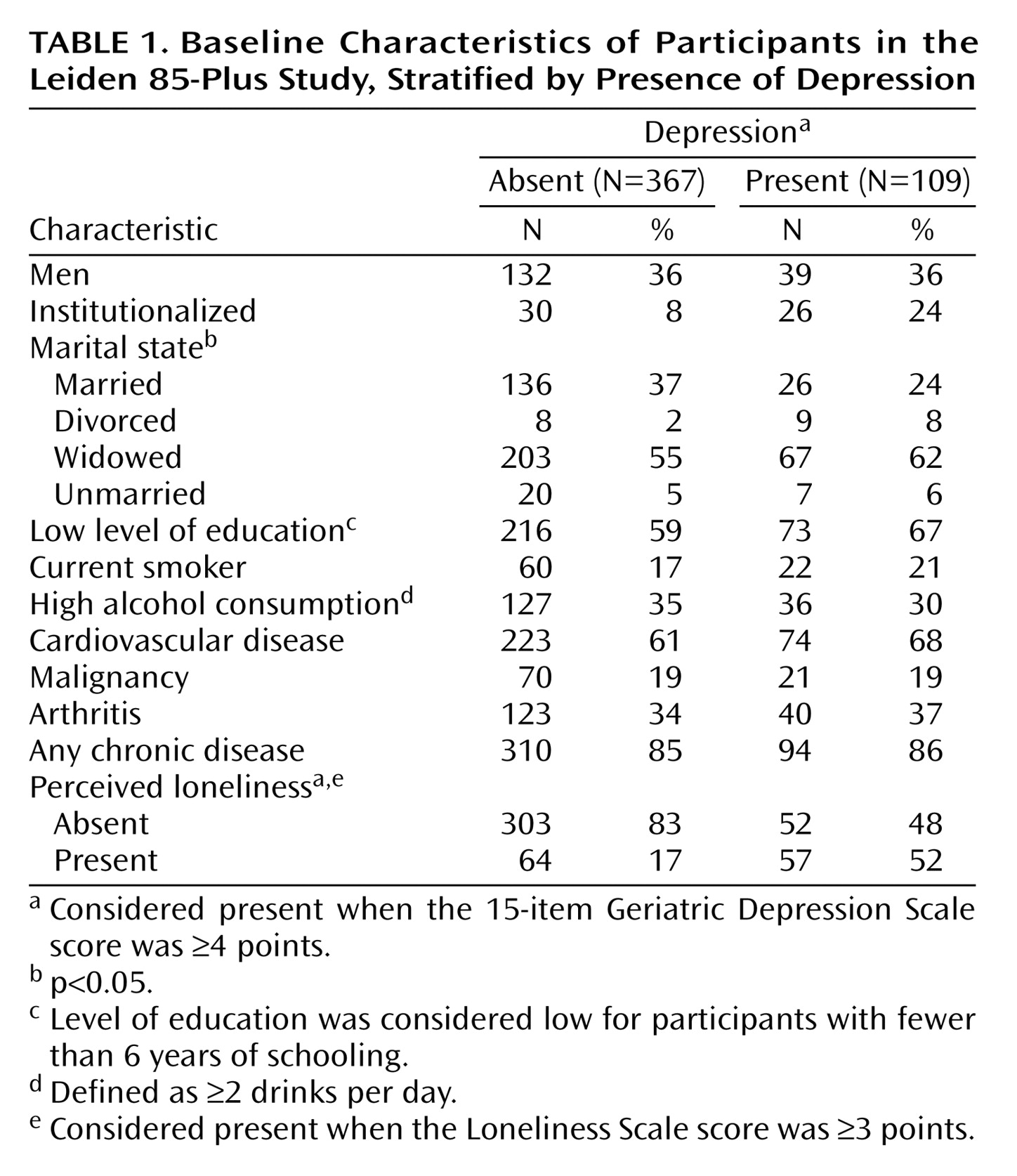
(11). Of all 500 participants with an MMSE score above 18 points, 476 participants completed both the Geriatric Depression Scale and the Loneliness Scale. The prevalence of depression, as defined by 4 points or more on the Geriatric Depression Scale, was 23% (N=109). Institutionalization, marital state, and perceived loneliness were significantly associated with depression (
Table 1). Perceived loneliness, defined as 3 points or more on the Loneliness Scale, was present in 25% of the participants (N=121) and was significantly associated with institutionalization, marital state, and depression. During follow-up, the refusal rate was below 0.5% per year. The variability of depressive symptoms and perceived loneliness was stable over time.
In total, 141 of the 476 participants died during follow-up. The participants with depression had an almost twofold increased mortality risk compared to those without depression (relative risk=1.9, 95% CI=1.3–2.8). This increased risk was unaffected after adjustments for demographic variables, smoking, alcohol consumption, and the presence of any chronic disease (relative risk=1.8, 95% CI=1.3–2.7). In contrast, perceived loneliness had no significant effect on mortality (unadjusted relative risk=1.4, 95% CI=0.9–2.1, and adjusted relative risk=1.3, 95% CI=0.8–1.9).
Because there was a strong association between depression and perceived loneliness (
Table 1), we examined the effect of perceived loneliness in depressed participants with respect to mortality. The mortality rate for participants without characteristics of depression and perceived loneliness was 59 deaths per 1,000 person-years at risk. For lonely participants, this was 50 per 1,000 person-years at risk, whereas the mortality rate was 68 per 1,000 person-years at risk for participants with depressive symptoms only. When both depression and loneliness were present, the mortality rate was 121 deaths per 1,000 person-years at risk.
We figured the unadjusted mortality risks for depression with and without perceived loneliness. Mortality risks were estimated in a Cox proportional hazards model with depression and/or perceived loneliness as time-dependent covariates, respectively. Depression was considered present when the 15-item Geriatric Depression Scale score was ≥4 points. Perceived loneliness was considered present when the Loneliness Scale score was ≥3 points. With the reference point set at 1 for the absence of both loneliness and depression, the presence of loneliness and the absence of depression had a relative risk of 0.8 (95% CI=0.4–1.6). The absence of loneliness and the presence of depression had a relative risk of 1.2 (95% CI=0.6–2.3), and the presence of loneliness and depression had a relative risk of 2.1 (95% CI=1.3–3.4).
The mortality risk of depression with perceived loneliness was two times higher (relative risk=2.1, 95% CI=1.2–3.4), but no significant effect remained in the absence of perceived loneliness. The mortality risks were unaffected after adjustment for sex, marital state, living arrangement, education, smoking, alcohol consumption, and chronic diseases (relative risk=2.0, 95% CI=1.2–3.2). When chronic diseases were introduced in the model as continuous data or as separate diseases, the mortality risks did not change.
Discussion
This is the first prospective study on the relationship between depression, perceived loneliness, and all-cause mortality in the community-based oldest old. In line with studies in younger elderly
(2–
5), the presence of depressive symptoms had a marked effect on mortality. Controlling for demographic variables, smoking, alcohol consumption, and chronic diseases did not change this association. Perceived loneliness in itself had no effect on mortality, although at baseline, depression was associated with feelings of loneliness. In the absence of perceived loneliness, there was no significant effect of depression on the mortality risk anymore. The presence of perceived loneliness, however, contributed strongly to the effect of depression on mortality. Thus, in the oldest old, depression is associated with mortality only when feelings of loneliness are present.
A possible limitation of this study is that depression was not formally diagnosed. However, it becomes increasingly clear that in the elderly, subthreshold depression and depressive symptoms have as distinct effects on mortality as depressive disorders do
(2). Moreover, our reanalyses with different cutoffs on the Geriatric Depression Scale (3 or more points, 5 or more points) yielded similar results. Major strengths of the present study are the prospective design, the representative sample, the measurement of control variables, and the yearly applied measurements of depression and perceived loneliness. In addition, loneliness was studied as perceived feelings of the participants and not as a status derived from demographic characteristics, such as institutionalization or living arrangements.
In clinical practice, the prognosis of depression in the oldest old in terms of mortality is poor when accompanied by feelings of loneliness. It may be that the nature of depression with feelings of loneliness differs from depression without feelings of loneliness. One could hypothesize that depression with feelings of loneliness leads to more pronounced motivational depletion and to “giving up.” This could have serious consequences, including social isolation, reduced self-care, decreased mobility, poor diet, and reduced compliance with a prescribed drug regimen, all possible pathways to early death. Further exploration of the clinical features of depression in the oldest old could lead to a better understanding of “how depression kills” in order to develop possible interventions.