Despite mounting evidence of psychiatric morbidity following peacekeeping operations
(1), to our knowledge no data have appeared on clinical profiles of peacekeepers who seek treatment or on their response to standard intervention models. Given increasing deployments of defense forces on peacekeeping missions, it is important to better understand the needs and treatment responses of these veterans. In the absence of such data, assumptions that peacekeepers will benefit from the same models of treatment as those used for chronic posttraumatic stress disorder (PTSD) in combat veterans should be questioned.
Treatment programs for Australian Vietnam veterans with PTSD have existed for several years. These programs report modest but clinically significant improvements, with gains maintained to 9-month follow-up
(2,
3). Although the programs are designed primarily for Vietnam combat veterans with chronic PTSD and considerable comorbidity, Australian veterans of peacekeeping deployments are increasingly participating in these programs. Differences in clinical presentation and outcome between Vietnam and peacekeeper veterans may be expected given the different nature of peacekeeping stressors (which may include witnessing violence while prohibited from intervening), the more recent onset of disorder among peacekeepers, and the differences in life stages (many peacekeepers have young families and associated stressors).
This study compares initial symptom profiles and treatment outcomes of peacekeepers and Vietnam veterans attending PTSD treatment programs. The findings may inform tailoring of treatment to the veteran’s presentation and operational history, helping to clarify the appropriateness of programmatic treatment models for peacekeeper veterans.
Method
Participants were a convenience sample of 63 Vietnam veterans and 66 peacekeeper veterans attending PTSD treatment programs. Peacekeeping deployments included Timor, Cambodia, Rwanda, and Somalia. At intake, all participants met PTSD criteria on the Clinician-Administered PTSD Scale
(4) administered by trained clinical staff.
Peacekeepers (mean age=35.68, SD=7.05) were younger than the Vietnam veterans (mean age=52.69, SD=3.02) (F=256.49, df=1, 127, p<0.001) and reported more recent symptom onset (mean=72.00 months, SD=48.45, versus mean=278.12 months, SD=130.43) (F=123.04, df=1, 127, p<0.001).
As part of a standardized assessment at intake and 3 months after treatment (6 months after intake), participants completed self-report questionnaires including the PTSD Checklist
(5), Hospital Anxiety and Depression Scale
(6), Alcohol Use Disorders Identification Test
(7), and the anger items of the War Stress Inventory used by the U.S. Department of Veterans Affairs in their PTSD programs
(8). These measures are valid and reliable and have been used in other studies. Details of these measures and the treatment programs have been reported elsewhere
(2).
The study group comprised veterans who completed treatment in groups of six to eight at one of three facilities. The treatment protocol in all programs followed a set of guidelines established by the Australian Centre for Posttraumatic Mental Health. Approximately 61% of the peacekeepers participated in programs where they represented the entire treatment group, and 39% participated in mixed treatment groups with Vietnam veterans. For treatment groups comprising only peacekeepers, the same number of Vietnam veterans from the following treatment group at the same facility were selected for comparison. For treatment groups comprising both peacekeepers and Vietnam veterans, an equal number of randomly selected veterans from the same treatment group were chosen for comparison. After complete description of the study to participants, written informed consent was obtained from all.
Multivariate analysis of variance (MANOVA) was used to compare symptom profiles of peacekeepers and Vietnam veterans at intake. Treatment effects by group were examined by using repeated-measures MANOVA and effect sizes (Cohen’s d). Finally, a hierarchical linear regression was used to explore predictors of treatment outcome for the peacekeeper group.
Results
All participants completed the treatment program, although 3-month follow-up data were missing for 17 (26%) peacekeepers and 13 (21%) Vietnam veterans. For both groups, there were no significant differences on intake measures between those who were missing or present at 3 months. Missing data were imputed by using the last observation carried forward. Application of an alterative imputation method based on pattern matching procedures
(9) did not substantively change the outcome of any analysis.
Clinician-Administered PTSD Scale severity scores were significantly higher for peacekeepers than Vietnam veterans (mean=89.73, SD=17.83, versus mean=81.70, SD=18.46) (F=5.10, df=1, 127, p<0.03). Of the three symptom clusters, only reexperiencing was significantly more severe for peacekeepers (mean=25.09, SD=7.11, versus mean=20.96, SD=8.28) (F=9.05, df=1, 125, p=0.003). This difference was not significant after symptom duration was controlled for (F=2.45, df=1, 126, p>0.05).
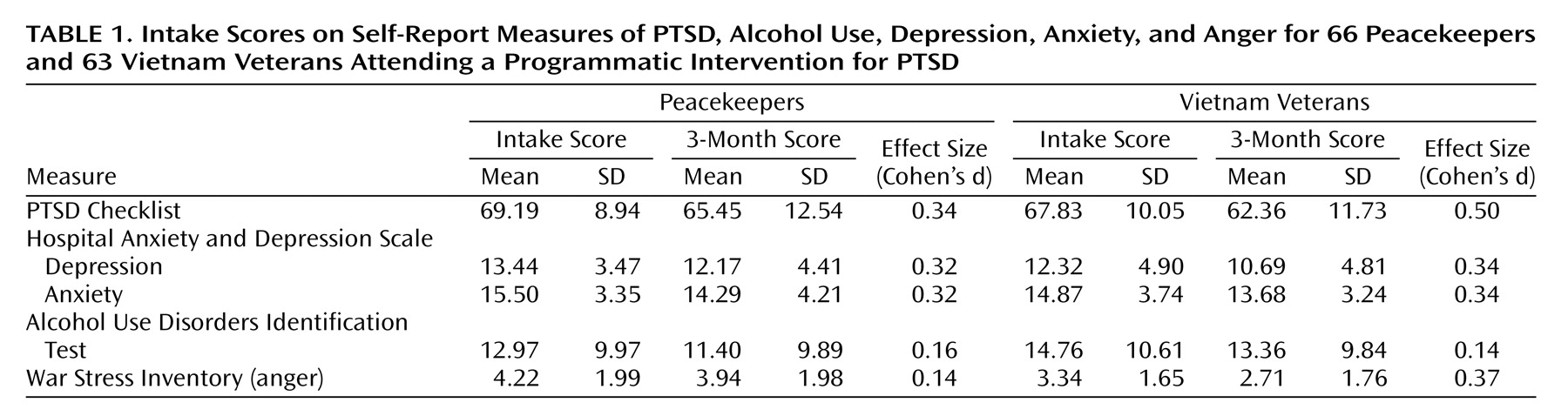
Clinical profiles from the self-report measures are shown in
Table 1. MANOVA identified no significant overall difference between groups on the five self-report intake measures (F=2.09, df=5, 115, p=0.07). Examination of univariate analyses, however, identified a significant difference for anger, with peacekeepers reporting more severe symptoms (F=7.31, df=1, 119, p<0.01). This difference was not maintained after age was controlled for (F=0.245, df=1, 118, p>0.05). Age was significantly correlated with anger (r=–0.25, p<0.01) but not with any other symptom measure. Greater age was associated with less anger.
The repeated-measures MANOVA indicated a significant main effect for time (F=8.45, df=5, 115, p<0.001) but no group-by-time interaction effect (F=0.81, df=5, 115, p=0.54), suggesting that both groups responded equally well to treatment. Controlling for age had little impact on the interaction effect. Effect size analyses using Cohen’s d identified moderate clinical improvements in PTSD, depression, and anxiety for both groups, as well as for anger in Vietnam veterans (
Table 1). Negligible change occurred for anger in peacekeepers or for harmful alcohol use in both groups.
The hierarchical regression revealed that anger but not duration of illness, alcohol use, depression, or anxiety, was a significant predictor of 3-month PTSD (controlling for PTSD at intake) for the peacekeeper group (F change=6.01, df=1, 50, B=1.56, SE=0.64, β=0.27, t=2.45, p<0.05), accounting for an additional 3% of the variance. Lower anger levels were associated with better outcomes.
Discussion
We found that the reexperiencing component of clinician-rated PTSD was more severe for peacekeepers than for their Vietnam veteran counterparts. This difference was a function of more recent symptom onset. No differences were apparent on the PTSD self-report measure. Of the two instruments, however, the Clinician-Administered PTSD Scale is considered the more reliable and valid measure.
Of the self-reported comorbidity, only anger was significantly more elevated for peacekeepers. Both groups reported improvement following treatment, albeit with relatively modest gains. These data are consistent with previous reports for Vietnam veterans (e.g., references
3,
4), but to our knowledge this is the first report on treatment effects for peacekeepers with PTSD. The outcomes remain somewhat disappointing; it had been anticipated that shorter duration of illness in peacekeepers would result in a better prognosis.
Several of the differences seem to relate to anger. Peacekeepers reported greater anger at intake and less change in anger following treatment. Of the four comorbid features examined as predictors of PTSD symptom change, only anger was significant.
There are two key implications of these findings for treatment of peacekeepers. First, treatment should ensure that adequate attention is directed at addressing reexperiencing symptoms through trauma-focused interventions. Second, improved results may result from focusing on anger before initiating PTSD treatment or in the early stages of treatment.
Clearly, the current results should be interpreted cautiously and are presented purely as a starting point for clinical research with this population. Numbers were small, precluding use of more sophisticated data analytic approaches and potentially masking important differences (such as across specific deployments). Absence of a measure for use of drugs other than alcohol is problematic given anecdotal reports of widespread use of illicit drugs among peacekeepers. Nevertheless, the findings are a crucial starting point in developing best-practice treatment models with this growing population of veterans.