Damage to the orbitofrontal cortex has been associated with disinhibited or socially inappropriate behavior and emotional irregularities
(1–
5). Prominent characteristics of several personality disorders, in particular DSM-IV borderline personality disorder, include impulsivity and affective instability. Despite the abundance of evidence linking impulsivity to frontal lobe dysfunction, evidence for underlying frontal lobe deficits in personality disorder patients with a history of impulsivity is limited, and there is even less evidence linking borderline personality disorder specifically to frontal lobe deficits
(6). Neuroimaging studies show differences in the prefrontal cortex in people with borderline personality disorder, compared to healthy subjects, at baseline
(7–
9) and in response to aversive stimuli
(10) and neuropharmacological probes associated with impulsivity
(11,
12). Some evidence from brain imaging studies suggests orbitofrontal cortex dysfunction in borderline personality disorder
(13–
16), specifically hypometabolism
(7,
8,
11) and smaller volume
(9,
13) of the orbitofrontal cortex.
In this study, our aim was to determine if certain aspects of borderline personality disorder, in particular impulsivity, are associated with orbitofrontal cortex dysfunction. We used questionnaires on personality, emotion, and impulsivity together with a number of computer-based tasks that are sensitive to frontal lobe dysfunction to assess possible underlying factors related to impulsivity in patients with orbitofrontal cortex lesions, patients with lesions in the prefrontal cortex but not in the orbitofrontal cortex, patients with borderline personality disorder and a history of self-harm, and healthy comparison subjects. This combination of tests allows for new comparisons of cognitive and behavioral traits and for identification of patterns and dissociations between different types of dysfunctions within borderline personality disorder. A unique feature of this study is the comparison of the clinical population of borderline personality disorder patients to patients with lesions in the prefrontal cortex. This study design provides an excellent opportunity to increase understanding of the biological etiology of borderline personality disorder as well as of the functions of the brain.
On the basis of previous research, we hypothesized that frontolimbic circuit dysfunction, involving both the orbitofrontal cortex and amygdala regions, may be involved in borderline personality disorder and that some aspects of borderline personality disorder may be related to dysfunction of the orbitofrontal cortex. Our goal is to provide evidence of these relationships by comparing the performance of patients with borderline personality disorder and patients with orbitofrontal cortex lesions on a number of tests. In the absence of uniquely defined and identifiable neurological damage in patients with borderline personality disorder, this study is intended to provide information about the neurobiological correlates of certain behaviors in borderline personality disorder.
Method
Participants
Ethics approval was obtained from the University of Oxford, the Institute of Psychiatry (King’s College, London), and the Oxfordshire Psychiatric Research Ethics Committee. After complete description of the study to the subjects, written informed consent was obtained.
Healthy comparison subjects
The healthy comparison group consisted of 39 participants (10 male participants) ranging in age from 18 to 71 years (mean=40.3 years, SD=20.5). The healthy comparison subjects were recruited through the subject panel at the Department of Experimental Psychology, University of Oxford. Potential participants were excluded if they had disturbed vision (despite corrective devices) or a history of current neurological illness, a current major psychiatric illness, or current substance or alcohol abuse.
Prefrontal lesion patients
The 43 prefrontal lesion patients in this study were recruited from the Department of Neurosurgery, King’s College Hospital, London (N=19); the International Subarachnoid Aneurysm Trial at the Radcliffe Infirmary, Oxford, England (N=16); and the Oxford Centre for Enablement, Oxford, England (N=8). The time since the patients sustained their lesion varied considerably, from 6 months to 20 years (mean=5.0 years, SD=4.8). Clinical information for each lesion patient and the basis for division into orbitofrontal cortex and dorsolateral prefrontal cortex lesion groups are summarized in
Table 1 of our earlier publication
(5).
Twenty patients (eight male patients) constituted the comparison patients with prefrontal cortex lesions outside the orbitofrontal cortex. The patients ranged in age from 19 to 71 years (mean=46.0 years, SD=15.1). The dorsolateral prefrontal cortex (with or without the medial prefrontal cortex) was the main site of damage in the patients included in this group.
The patients with orbitofrontal cortex lesions consisted of 23 patients (15 male patients) ranging in age from 30 to 63 years (mean=48.7 years, SD=10.0) with damage including or restricted to the orbitofrontal cortex (either bilaterally or unilaterally).
Patients with borderline personality disorder
Nineteen self-harming inpatients with DSM-IV borderline personality disorder (18 female patients) ranging in age from 19 to 49 years (mean=32.37 years, SD=8.4) were tested at the Bethlem Royal Hospital Crisis Recovery Unit, London. (About 75% of borderline personality disorder diagnoses are made in female patients.) The unit provides a rehabilitation program in which the patients are taught to seek alternatives to and gain a better understanding of self-harm and to tolerate distressing feelings. Cutting and burning were among the most common forms of self-harm in the patients who participated in the study. Self-harm provided an objective indication of impulsive behavior and was an important factor in obtaining a homogeneous patient group. Descriptive and systematic data reveal that repetitive self-mutilation is typically an impulsive act
(17). Potential participants were excluded if they had current substance or alcohol abuse. Because all of the patients were in a 6-month inpatient rehabilitation program, we knew that for at least the time they were in the program they were not dependent on substances or alcohol. (Although most patients with borderline personality disorder were taking medications intended to improve their borderline personality disorder symptoms, they still performed poorly on tasks related to impulsivity, emotion, and personality and did not perform poorly on other tasks such as spatial working memory tasks.)
Materials and Procedures
See our earlier publication
(5) for the rationale for choice of measures.
Questionnaires
The self-report impulsivity measure was the Barratt Impulsiveness Scale, version 11
(18). This 30-item, 4-point Likert-type questionnaire was used as a trait measure of impulsivity. Long-term patterns of behavior were assessed with three subscales: nonplanning, motor, and cognitive impulsivity.
The personality questionnaire was the Big Five Inventory
(19), a 44-item, 5-point Likert-type questionnaire designed to measure the five scales/domains of the Five-Factor Model of Personality
(20): extraversion, agreeableness, conscientiousness, neuroticism, and openness to experience
(21).
The frontal behavior questionnaire is a self-report 20-item, 5-point Likert-type questionnaire
(5) designed to measure types of behavioral problems believed to result from frontal brain damage
(22), e.g., disinhibition, social inappropriateness, perseveration, and cooperativeness.
The borderline personality disorder questionnaire
(23), which consists of 18 yes/no questions modeled on the DSM-III criteria for borderline personality disorder, was used for assessment of borderline personality disorder characteristics.
The subjective emotion questionnaire measures how often participants experience sadness, anger, fear, happiness, and disgust in their current daily life. Ratings are made on a 4-point Likert-type scale. The emotional change questionnaire was given only to the patients with lesions and the patients with borderline personality disorder. This questionnaire assesses change (increase, decrease, or no change) since brain injury or onset of personality disorder in the capacity to feel sadness, anger, fear, happiness, and disgust. Both questionnaires were adapted from a previously developed subjective emotion questionnaire
(1,
24).
Tests
The Probabilistic Reversal Test includes an “acquisition” task in which participants learn to touch one of two patterns on the computer screen and to avoid touching the other and a “reversal” task in which they then learn to reverse or extinguish that choice based on monetary rewards and punishers
(5). Measures of performance include 1) punishment insensitivity (the total number of consecutive touches to a stimulus after having lost a minimum of £250), which measures the extent to which participants fail to switch immediately from a stimulus on the next trial following a large loss, and 2) reward insensitivity (the total number of times a participant touched a stimulus and won a minimum of £80 but did not touch the same stimulus again on the next trial), which measures the extent to which participants fail to select the same stimulus again after a large gain was associated with that stimulus.
The Matching Familiar Figures Test
(25), a standard cognitive behavioral measure of impulsivity, measures reflection-impulsivity, a composite of two dimensions: 1) latency to first response and 2) accuracy of choice or total errors. Participants observe a standard picture and select from a set of highly similar pictures the one that is the same as the standard picture. Twelve target objects with eight variants each were administered. The mean time of the latency of participants’ first response across all trials and the number of errors made before choosing the correct item were recorded.
The Spatial Working Memory Task from the Cambridge Neuropsychological Test Automated Battery (CeNeS Ltd., Cambridge, U.K.), a standard test
(5,
26), was used as a comparison condition. The measures were 1) between errors (number of times the subject revisits a box where a token has already been found), 2) within errors (number of times a subject revisits a box already found to be empty during the same search), and 3) strategy (the number of times the subject begins a new search with the same box)
(26). A high score denotes poor use of the strategy, and a low score denotes effective use.
The time perception task
(5) has two elements: time estimation and time production. For time estimation, participants were asked to estimate time intervals (10, 30, 60, and 90 seconds; each presented twice in a random sequence) during which they were distracted by being required to read aloud from a computer screen a series of randomly generated numbers from 1 to 9 that ranged in presentation time from 100 to 2900 milliseconds in order to prevent subvocal counting. The number of seconds estimated after each interval, averaged across two runs, and the total time estimated (the sum of the average times estimated at each interval divided by 190, which was the total number of seconds that actually passed) were recorded. The procedure for time production was the same as that for time estimation (reading aloud randomized numbers) except that participants were asked to press a computer key when they thought a set number of seconds had passed. For each time interval, the time produced was compared to the actual time participants were asked to produce. The number of seconds produced at each interval, averaged across two runs, and the total time produced (sum of the average times produced at each interval divided by 190, which was the total number of seconds participants were asked to produce) were recorded.
Statistical Analyses
A one-way analysis of variance (ANOVA) was performed for each of the variables to determine if the mean scores differed significantly by group. If an ANOVA yielded a significant F value, a Fisher’s least significant difference post hoc test was performed to identify the specific source of the difference. An alpha level of 0.05 was used for all statistical tests. Kruskal-Wallis nonparametric tests were performed for variables for which normality was not present. If the Kruskal-Wallis test yielded nonsignificant results, no results are reported for that variable.
Because ANOVAs revealed between-group differences in terms of age (F=4.36, df=3, 97, p=0.006) and gender (F=7.30, df=3, 97, p<0.001), analyses of covariance were performed across all variables, and these analyses discounted any confounding effects of age or gender on the results. No significant difference in the number of years since their lesion was found between the patients with orbitofrontal cortex lesions (mean=4.94, SD=4.22) and those with lesions in the prefrontal cortex but not in the orbitofrontal cortex (mean=4.95, SD=5.40), and years since lesion did not correlate significantly with any of the test variables, with Bonferroni correction (see Results section).
The patients recruited from King’s College completed most questionnaires, but they did not complete the behavioral tests because of time constraints and did not complete the borderline personality disorder questionnaire because of sensitivity issues. A few other participants did not complete all of the tasks because of testing time constraints.
Results
When not otherwise noted, all stated differences for post hoc least significant difference analyses were significant at p<0.05, and many were significant at p<0.001.
Similarities Between Patients With Orbitofrontal Cortex Lesions and Borderline Personality Disorder Patients
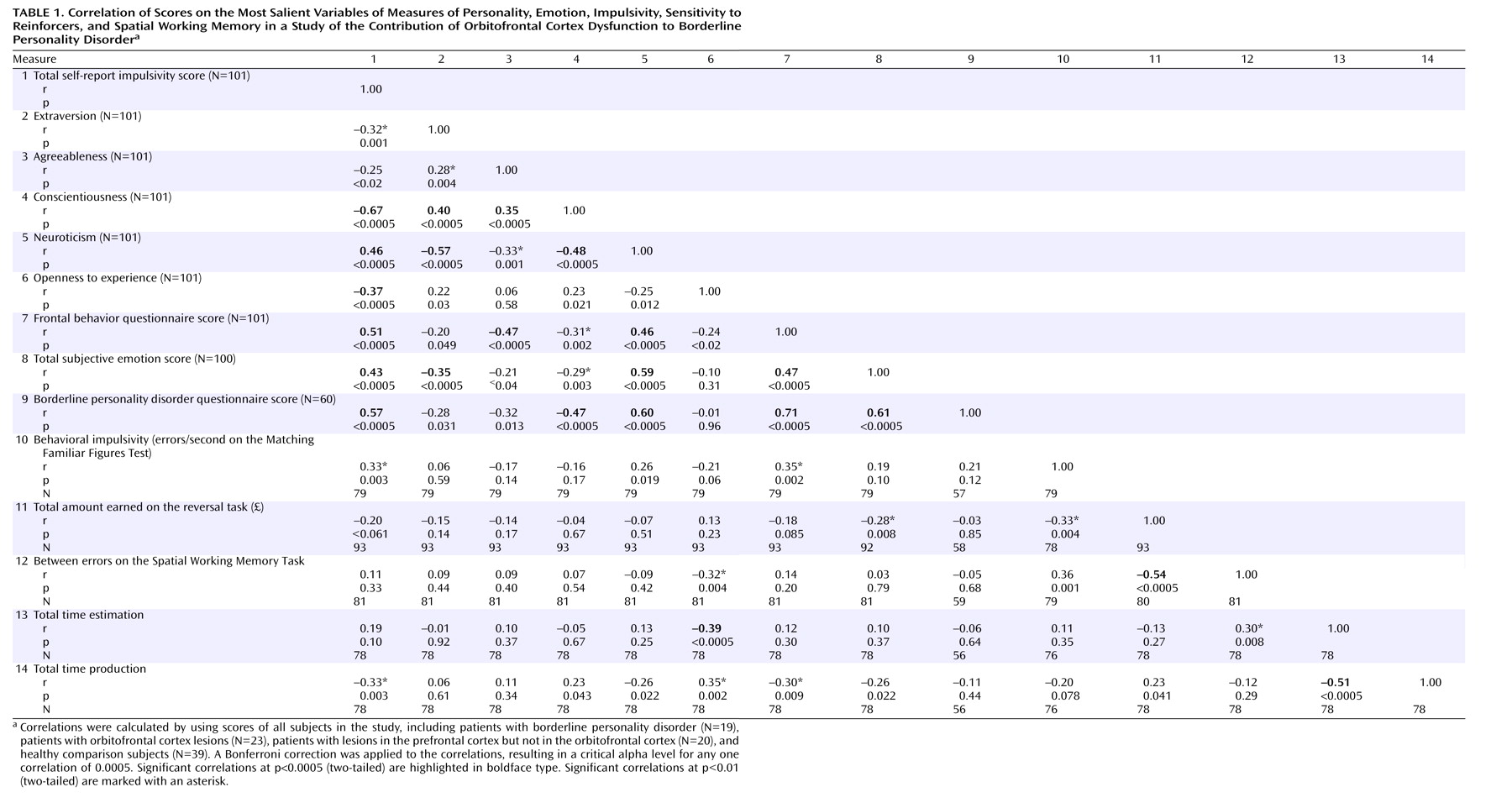
Results are presented here (and in
Figure 1,
Figure 2, and
Figure 3) for measures on which both the orbitofrontal cortex lesion group and the borderline personality disorder group were significantly impaired, compared to the healthy group (and, for some variables, compared to patients without orbitofrontal cortex lesions), regardless of whether they differed significantly from each other.
Self-report impulsivity
ANOVAs performed on the self-report impulsivity total score and on the three subscale variables were all significant (total self-report impulsivity score: F=25.89, df=3, 97, p<0.001; nonplanning impulsivity: F=20.82, df=3, 97, p<0.001; motor impulsivity: F=10.83, df=3, 97, p<0.001; and cognitive impulsivity: F=13.42, df=3, 97, p<0.001).
Least significant different post hoc tests showed that on all self-report impulsivity measures, the patients with orbitofrontal cortex lesions and the patients with borderline personality disorder were significantly more impulsive than both the healthy comparison subjects and the patients with lesions outside the orbitofrontal cortex, the patients with borderline personality disorder were more impulsive than the patients with orbitofrontal cortex lesions, and the healthy comparison subjects and the patients with lesions outside the orbitofrontal cortex did not differ significantly from each other (
Figure 1).
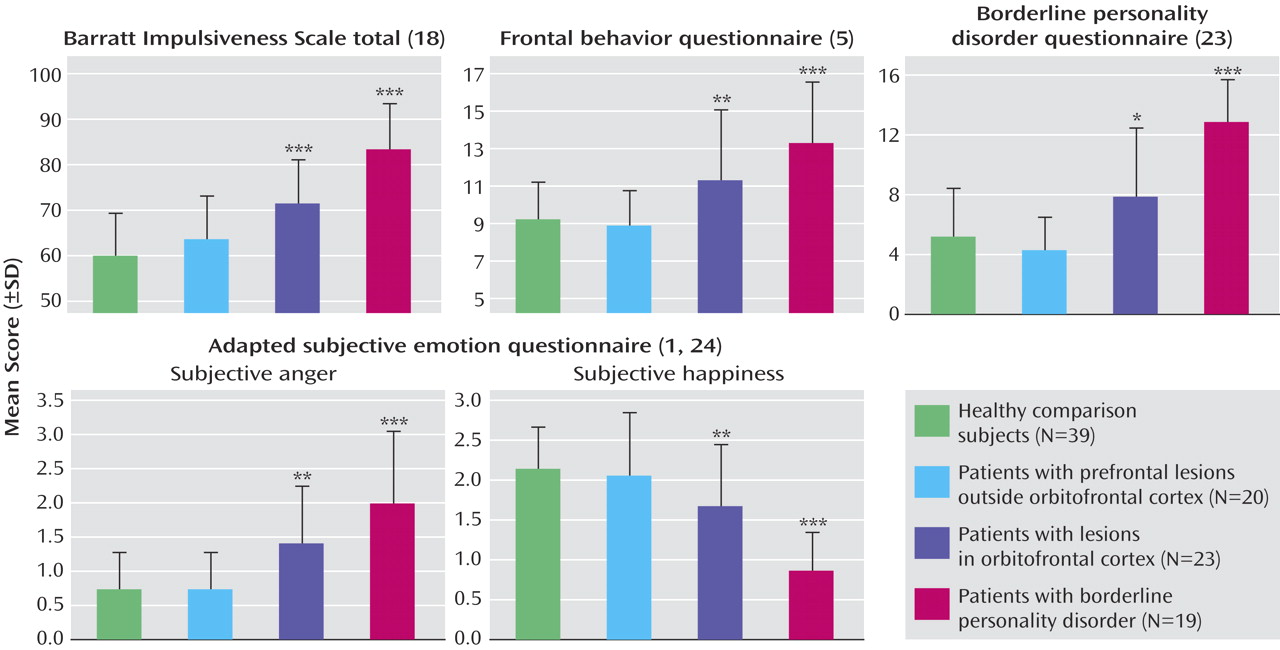
Behavioral impulsivity
ANOVAs performed on the Matching Familiar Figures Test variables (
Figure 2 and
Figure 3) showed significant differences between groups on all variables (errors per second: F=6.49, df=3, 75, p=0.001; number of errors: F=11.49, df=3, 75, p<0.001; and time latency: F=5.28, df=3, 75, p=0.002).
Post hoc analysis revealed that patients with orbitofrontal cortex lesions and patients with borderline personality disorder were more behaviorally impulsive than the healthy comparison subjects on all three measures and that the patients with orbitofrontal cortex lesions were more impulsive than the patients with borderline personality disorder on all but the time latency measure. The healthy comparison subjects and the patients with lesions outside the orbitofrontal cortex did not differ significantly from each other on the errors per second and time latency measures, but the patients with lesions outside the orbitofrontal cortex lesions were more impaired on the number of errors measure.
Frontal behavior questionnaire
There were significant differences between groups on the measure of behavioral problems believed to result from frontal damage (F=12.40, df=3, 97, p<0.001) (
Figure 1). Post hoc analysis revealed that the mean frontal behavior questionnaire total scores of the patients with orbitofrontal cortex lesions and the patients with borderline personality disorder were significantly higher than those of both the patients with lesions outside the orbitofrontal cortex and the healthy comparison subjects. Post hoc analysis showed that the mean frontal behavior questionnaire total score of the patients with borderline personality disorder was significantly higher than that of the patients with orbitofrontal cortex lesions. There was no significant difference between the healthy comparison subjects and the patients with lesions outside the orbitofrontal cortex.
Borderline personality disorder questionnaire
There were significant group differences in scores on the borderline personality disorder questionnaire (F=21.40, df=3, 55, p<0.001) (
Figure 1). Post hoc analysis revealed that the scores of the patients with borderline personality disorder were significantly higher than those of all other groups (p<0.001) and that the patients with orbitofrontal cortex lesions had significantly higher scores than those of the healthy comparison subjects and the patients with lesions outside the orbitofrontal cortex (p<0.05). There was no significant difference between the healthy comparison subjects and the patients with lesions outside the orbitofrontal cortex.
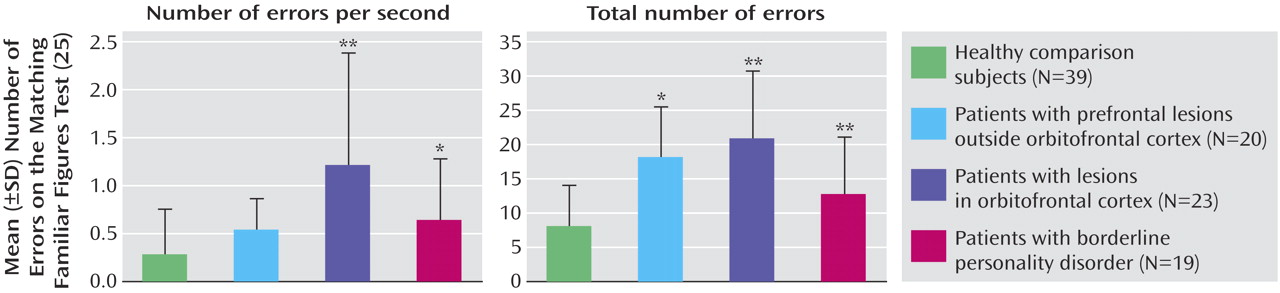
Time production
ANOVAs showed significant group differences in total time production and in time production at 60 and 90 seconds (total time production: F=2.95, df=3, 74, p<0.05; time production at 60 seconds: F=2.82, df=3, 74, p<0.05; and time production at 90 seconds: F=5.04, df=3, 74, p<0.01). Whereas all subjects overproduced time (except the patients with orbitofrontal cortex lesions at 90 seconds), least significant difference post hoc analysis revealed that the patients with orbitofrontal cortex lesions and the patients with borderline personality disorder produced significantly less time than the healthy comparison subjects (indicating a sped-up subjective sense of time) in measures of total time production (p<0.05) and of time production at 60 seconds (p<0.05) and 90 seconds (p<0.01). Underproduction became more apparent at longer time intervals (
Figure 3).
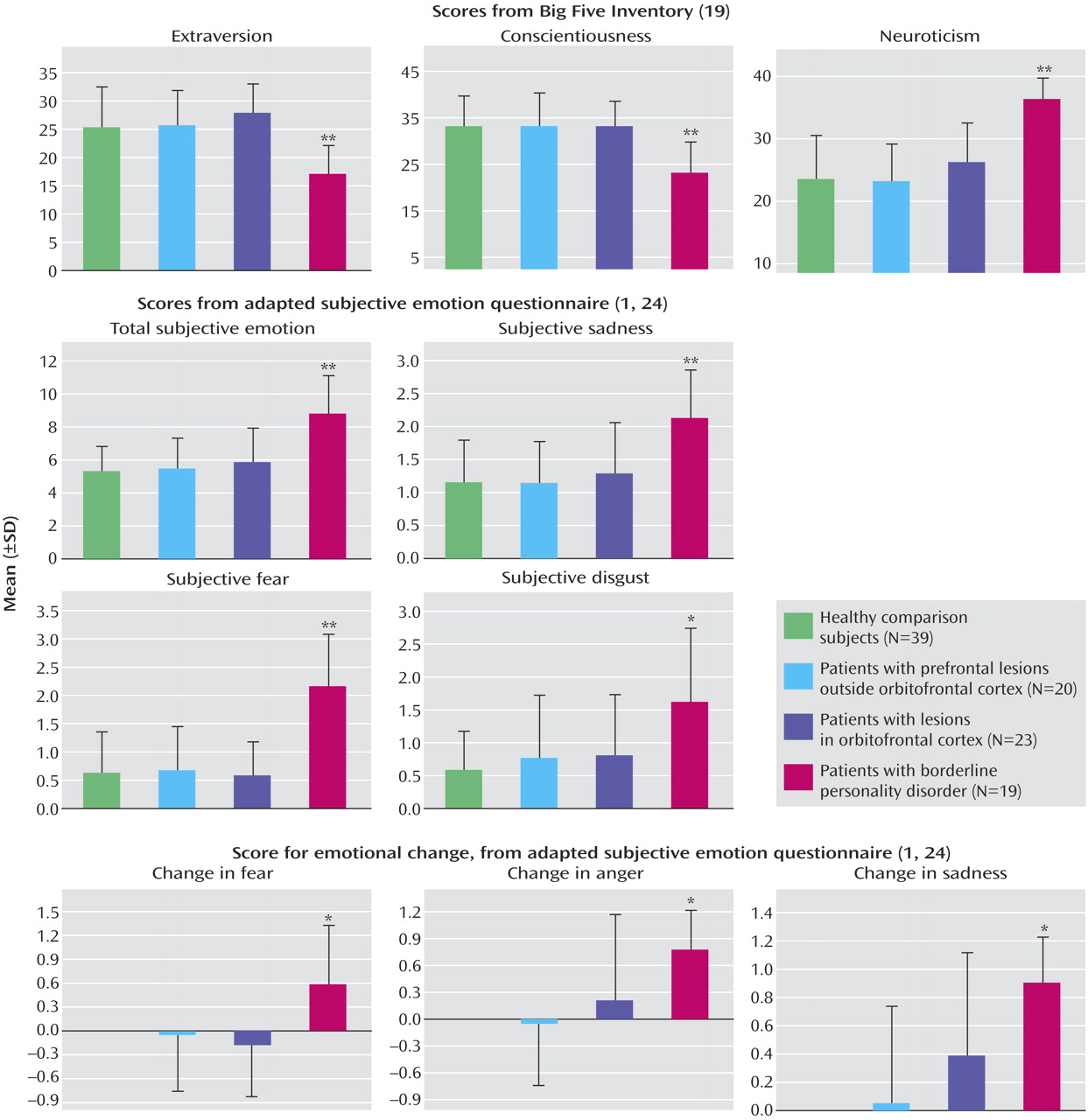
Personality
ANOVAs performed on each of the personality questionnaire (Big Five Inventory) variables indicated that participants’ scores on extraversion, conscientiousness, neuroticism, and openness to experience were significantly related to their group (extraversion: F=12.15, df=3, 97, p<0.001; conscientiousness: F=12.71, df=3, 97, p<0.001; neuroticism: F=23.00, df=3, 97, p<0.001; openness to experience: F=6.43, df=3, 97, p=0.001). However, openness to experience (
Figure 3) was the only variable on which both the patients with orbitofrontal cortex lesions and the patients with borderline personality disorder were impaired. The other variables are discussed later because only the patients with borderline personality disorder were affected. The healthy comparison subjects were significantly more open to experience than all other participants (p<0.005).
Subjective emotion questionnaire
ANOVAs performed on each of the variables (total subjective emotion score, sadness, anger, fear, disgust, and happiness) revealed that participants’ scores on all six measures were significantly related to their group (total subjective emotion: F=17.17, df=3, 96, p<0.001; sadness: F=10.84, df=3, 96, p<0.001; anger: F=14.48, df=3, 96, p<0.001; fear: F=23.78, df=3, 96, p<0.001; disgust: F=6.62, df=3, 96, p<0.001; happiness: F=19.00, df=3, 96, p<0.001).
Post hoc tests revealed that the patients with borderline personality disorder and the patients with orbitofrontal cortex lesions both had a deficit in subjective anger and subjective happiness (
Figure 1). The subjective anger of the patients with borderline personality disorder was significantly higher and their subjective happiness was significantly lower, compared to all other groups. The subjective anger of the patients with orbitofrontal cortex lesions was significantly higher and their subjective happiness was significantly lower, compared to the healthy comparison subjects and the patients with lesions outside the orbitofrontal cortex. There were no significant differences between the scores of the healthy comparison subjects and the patients with lesions outside the orbitofrontal cortex on these measures. All other variables are discussed in the next section because significant differences were found only for patients with borderline personality disorder.
Differences Between Patients With Orbitofrontal Cortex Lesions and Borderline Personality Disorder Patients
Histograms representing the means of variables discussed in this section are shown in
Figure 4 and
Figure 5.
Personality
ANOVAs for each personality (Big Five Inventory) variable indicated that participants’ scores on extraversion, conscientiousness, neuroticism (
Figure 4), and openness to experience (
Figure 3) were significantly related to their group (see statistical test results reported earlier). Post hoc tests revealed that the patients with borderline personality disorder were significantly less extraverted and conscientious and more neurotic than the participants in all other groups (p<0.001).
Subjective emotion
Post hoc analysis (conducted after the ANOVAs reported earlier) revealed that the total subjective emotion score of the patients with borderline personality disorder was significantly higher than that of all other groups (p<0.001). Furthermore, the patients with borderline personality disorder rated themselves as experiencing significantly more sadness (p<0.001), fear (p<0.001), and disgust (p<0.005) than all other groups (
Figure 4).
Emotional change
ANOVAs performed on each of the emotional change variables indicated that participants’ changes in sadness, anger, and fear (
Figure 4) were significantly related to their group (change in sadness: F=5.12, df=2, 49, p=0.01; change in anger: F=4.29, df=2, 49, p<0.05; change in fear: F=3.84, df=2, 49, p<0.05). The healthy comparison subjects did not complete this questionnaire.
Post hoc analysis revealed that the sadness of the patients with borderline personality disorder increased significantly more than that of the patients with lesions outside the orbitofrontal cortex (p<0.01). There was a significant difference in the change in anger between the patients with borderline personality disorder and the patients with lesions outside the orbitofrontal cortex (p<0.01). The anger of patients with borderline personality disorder increased, and that of the patients with lesions outside the orbitofrontal cortex decreased. The patients with borderline personality disorder showed a significant difference in change in fear, compared with both the patients with lesions outside the orbitofrontal cortex (p<0.05) and those with orbitofrontal cortex lesions (p<0.01). The fear of the patients with borderline personality disorder increased, whereas that of the patients with lesions outside the orbitofrontal cortex and of the patients with orbitofrontal cortex lesions decreased. The patients with orbitofrontal cortex lesions did not differ significantly from those with lesions outside the orbitofrontal cortex on any measure.
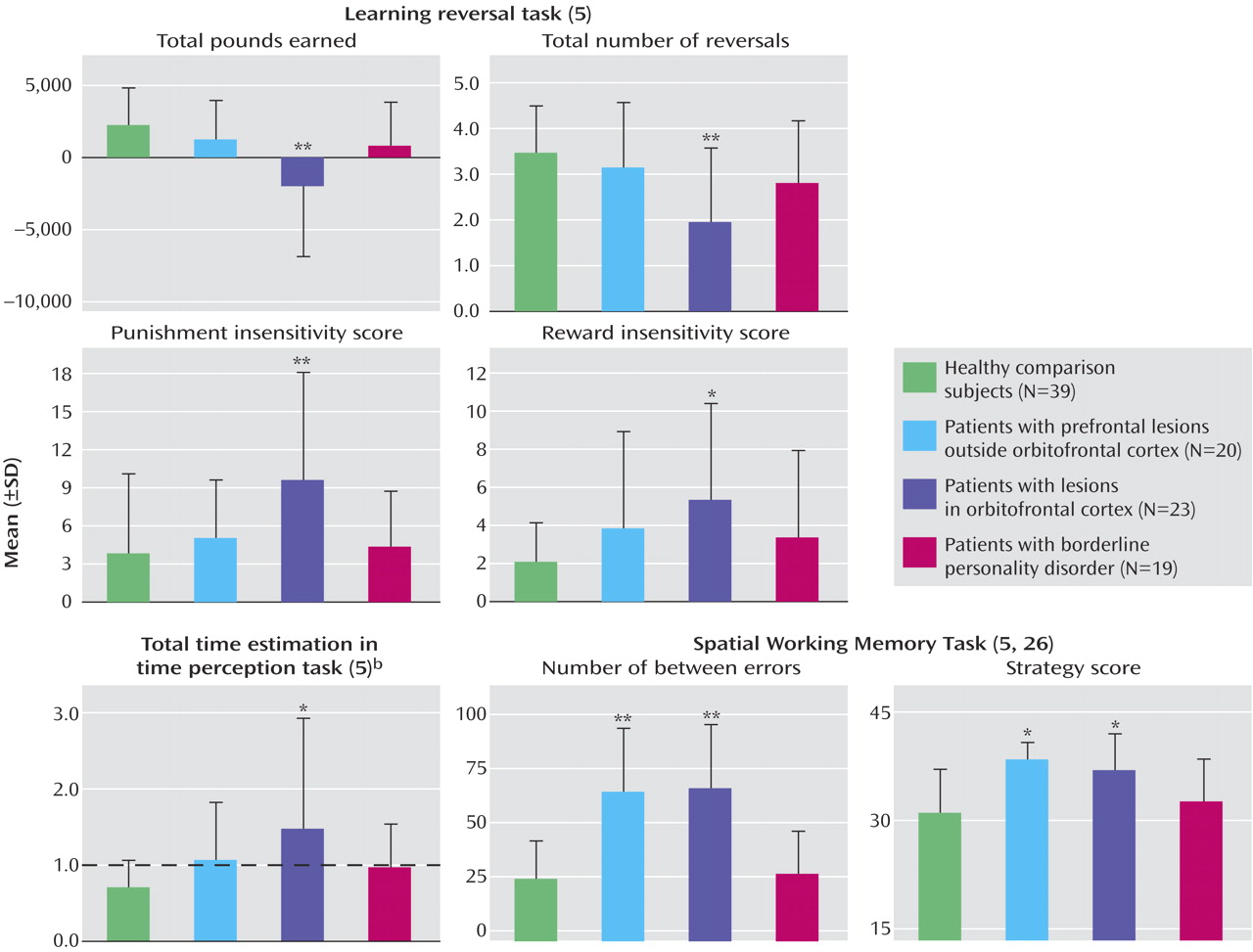
Probabilistic reversal
ANOVAs indicated that the participants’ scores differed significantly by group (
Figure 5) in terms of the total pounds accumulated by the 100th trial, total number of reversals achieved by 100 trials, and punishment insensitivity variables (total pounds: F=7.05, df=3, 89, p<0.001; total reversals: F=6.60, df=3, 89, p<0.001; punishment insensitivity: F=3.85, df=3, 89, p<0.05). (The King’s College neurosurgical patients were not included in the reversal analysis; their data are published elsewhere
[4].)
The patients with orbitofrontal cortex lesions were markedly impaired on the reversal tasks, compared to all other groups. The patients with borderline personality disorder were not impaired on these tasks, compared to the other groups. The groups also differed in reward insensitivity (F=3.22, df=3, 89, p<0.05), and the patients with orbitofrontal cortex lesions were significantly more reward insensitive than the healthy comparison subjects (p=0.003) only when outliers were included.
Time estimation
ANOVAs for each time perception variable indicated that participants differed significantly by group in terms of total time estimation (F=3.45, df=3, 74, p<0.05) (
Figure 5). Post hoc analysis revealed that the patients with orbitofrontal cortex lesions estimated that significantly more time had passed than did the healthy comparison subjects (p=0.002). Although the patients with orbitofrontal cortex lesions overestimated time, indicating a faster subjective sense of time, the healthy comparison subjects underestimated time, indicating a slower subjective sense of time. The patients with borderline personality disorder did not differ from the healthy comparison subjects on this variable.
Spatial working memory
Participants’ scores differed significantly by group on all three spatial working memory measures (
Figure 5) (between errors: F=19.27, df=3, 77, p<0.001; within errors: F=3.65, df=3, 77, p<0.05; strategy errors: F=6.69, df=3, 77, p<0.001).
Both the patients with lesions outside the orbitofrontal cortex and those with orbitofrontal cortex lesions (most had dorsolateral prefrontal cortex damage) made more between errors than did the healthy comparison subjects and those with borderline personality disorder (p<0.001). The patients with lesions outside the orbitofrontal cortex made significantly more within errors than did the healthy participants and those with borderline personality disorder (p<0.01). There were no significant differences in within errors between the healthy comparison subjects, the patients with orbitofrontal cortex lesions, and the patients with borderline personality disorder. Finally, the patients with lesions outside the orbitofrontal cortex and those with orbitofrontal cortex lesions both had more strategy errors, compared with the healthy subjects (p<0.01 and p=0.001, respectively) and with patients with borderline personality disorder (p<0.05).
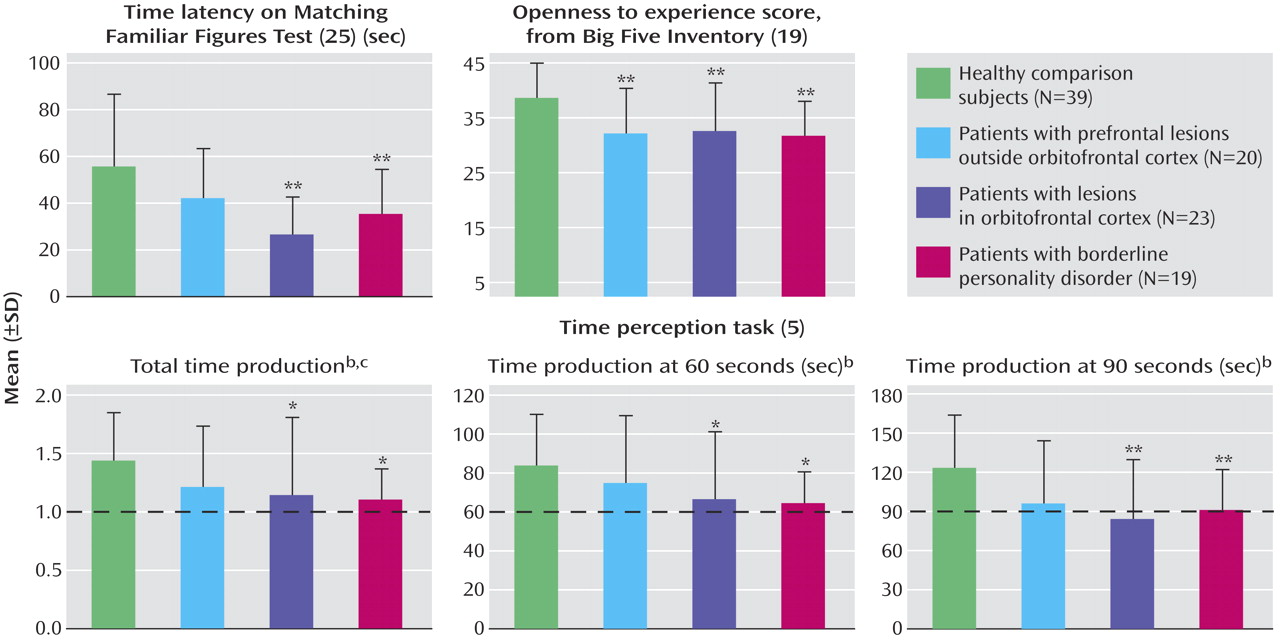
Correlations
To investigate the relationships between the different measures, Pearson’s correlations (two-tailed) were performed across the data for all participants (
Table 1). To compensate for the large number of comparisons, only the total score or main variable for each measure (all variables within each measure were significantly correlated with each other) was used in this analysis. A Bonferroni correction was applied, which resulted in the critical alpha level for any one correlation becoming 0.0005. Some correlations for which the alpha level was 0.01 are mentioned if they were deemed a priori to be interesting. (The emotional change questionnaire was not included in the correlation analysis because it was not administered to the healthy subjects.)
Discussion
This investigation used a relatively new approach of comparing the psychiatric population of patients with borderline personality disorder to neurological patients with orbitofrontal cortex brain lesions.
Patients with orbitofrontal cortex lesions and patients with borderline personality disorder performed similarly on some tests in that they were more impulsive and reported more inappropriate behaviors, more borderline personality disorder traits, more anger, and less happiness than subjects in both of the comparison groups (patients with prefrontal lesions outside the orbitofrontal cortex and healthy comparison subjects). They were also less open to experience and had a faster perception of time (in terms of time production) than the healthy comparison subjects. These findings suggest that orbitofrontal cortex functions may be related to these aspects of borderline personality disorder but not to the other borderline personality disorder characteristics that were measured, including levels of extraversion, conscientiousness, neuroticism, and emotion. Furthermore, patients with orbitofrontal cortex lesions but not patients with borderline personality disorder were impaired at reversing stimulus-reinforcer associations, suggesting that this orbitofrontal cortex dysfunction is not an essential part of borderline personality disorder.
Because the patients with borderline personality disorder were not impaired on the spatial working memory task and because the patients with lesions outside the orbitofrontal cortex and those with orbitofrontal cortex lesions did not perform poorly on the same tests, the neuropsychological deficits of the patients with borderline personality disorder and the patients with orbitofrontal cortex lesions could not be attributed to spatial working memory deficits or dorsolateral prefrontal cortex dysfunction.
Similarities Between Patients With Orbitofrontal Cortex Lesions and Borderline Personality Disorder Patients
Impulsivity
A major finding is that patients with orbitofrontal cortex lesions and patients with borderline personality disorder are similar in that they are both significantly more impulsive, as assessed with both behavioral and self-report measures, than healthy subjects and patients with prefrontal lesions outside the orbitofrontal cortex. Although it is well established that patients with borderline personality disorder are impulsive (impulsivity is one of the diagnostic criteria), the direct comparison with findings in patients with orbitofrontal cortex damage shows that patients with orbitofrontal cortex lesions are as impulsive as patients with borderline personality disorder. This finding suggests that this aspect of borderline personality disorder could be related to orbitofrontal cortex function.
It is interesting to note that both the patients with borderline personality disorder and those with orbitofrontal cortex lesions had significantly lower time latencies on the behavioral impulsivity task, compared with the healthy subjects. This result may be related to a desire to complete the task fast, combined with a lack of sensitivity to punishment in the patients with orbitofrontal cortex lesions and perhaps with the desire for the reward of finishing sooner in patients with borderline personality disorder.
Frontal behaviors and borderline personality disorder characteristics
Other important findings are that the patients with orbitofrontal cortex lesions performed similarly to the patients with borderline personality disorder on the borderline personality disorder questionnaire and that the patients with borderline personality disorder performed like the patients with orbitofrontal cortex lesions on the frontal behavior questionnaire. Support for a relationship between frontal behaviors and borderline personality disorder characteristics comes from the highly significant positive correlation between scores on the frontal behavior questionnaire and the borderline personality disorder questionnaire both within the healthy comparison group and across all participants (p<0.0005). Analysis of responses on individual frontal behavior questionnaire items (see reference
21) for the borderline personality disorder group showed that the correlations were highest (0.22–0.53) for the questions concerned with inappropriate behavior; being uncooperative, aggressive, abusive, angry, or irritable; not worrying about oneself; being listless; stopping to help others in need; stopping to think before acting or making a decision; and gambling and taking risks when gambling.
On both the frontal behavior questionnaire and the borderline personality disorder questionnaire, the scores of the patients with borderline personality disorder were significantly higher than those of the patients with orbitofrontal cortex lesions. It is interesting to note that the patients with borderline personality disorder experienced significantly more inappropriate frontal behaviors than the patients with orbitofrontal cortex lesions. The borderline personality disorder patients may have other dysfunctions (perhaps related to amygdala function), in addition to orbitofrontal cortex dysfunction, that make their emotional deficits and socially inappropriate behaviors more severe than those of patients with orbitofrontal cortex lesions.
Subjective emotion
The patients with orbitofrontal cortex lesions and those with borderline personality disorder both reported being significantly less happy and more angry than the patients without orbitofrontal cortex lesions and the healthy comparison subjects. This finding suggests a common underlying cause, namely orbitofrontal cortex dysfunction. In general, the borderline personality disorder group was more emotional than all other groups, and the orbitofrontal cortex group approached the emotional scores of the borderline personality disorder group in just these two aspects of emotion. Thus, although orbitofrontal cortex dysfunction could contribute to the changes in emotion in patients with borderline personality disorder, other factors and brain regions also appear to be involved.
Time production
Both the patients with orbitofrontal cortex lesions and the patients with borderline personality disorder produced less time than the healthy comparison subjects. A common cause for these two groups could be a higher level of frustration in waiting for the time to elapse. This study supports the evidence that impulsivity and time perception are related
(27,
28). The frustration in waiting and/or the faster cognitive tempo that may cause patients with orbitofrontal cortex lesions and patients with borderline personality disorder to underproduce time may also be related to some of the inappropriate social and emotional behaviors they display, as demonstrated by their higher scores on the borderline personality disorder, frontal behavior, and emotion questionnaires, compared to the healthy comparison subjects and the subjects with prefrontal cortex lesions outside the orbitofrontal cortex. In support of this relationship, lower levels of time production correlated with higher levels of frontal behaviors and lower levels of openness to experience across all subjects.
Personality
Both the patients with orbitofrontal cortex lesions and the patients with borderline personality disorder were less open to experience than were the healthy comparison subjects. There was no significant difference in this measure between the patients with orbitofrontal cortex lesions and the patients with borderline personality disorder.
Differences Between Patients With Orbitofrontal Cortex Lesions and Borderline Personality Disorder Patients
Personality
Patients with borderline personality disorder were more neurotic, less extraverted, and less conscientious than all other groups. Our evidence suggests a strong relationship between certain personality traits and emotions, which may be related to the same underlying neurological correlates that are affected in patients with borderline personality disorder. This interpretation is supported by the fact that the patients with borderline personality disorder had both personality and emotional abnormalities and by the strong correlations between total subjective emotion scores, borderline personality disorder traits, and measures of neuroticism, conscientiousness, and extraversion across all subjects. Since the patients with orbitofrontal cortex lesions did not differ from the healthy comparison subjects in measures of neuroticism, conscientiousness, extraversion, and subjective emotion, some brain region other than the orbitofrontal cortex (perhaps the amygdala) may be related to the personality and emotional abnormalities of patients with borderline personality disorder
(21).
It is interesting to note that the borderline personality disorder subjects reported a higher level of introversion, relative to the healthy comparison subjects, but that the patients with orbitofrontal cortex lesions did not. In borderline personality disorder patients, impulsivity (of the type measured here), interacting with introversion and high levels of emotionality, may cause self-harm, whereas self-harm may not develop in the patients with orbitofrontal cortex lesions, who are impulsive but not introverted or extremely emotional. In addition, the patients with orbitofrontal cortex lesions were not found to have an abnormally high level of extraversion, which, combined with impulsivity, could lead patients to harm others
(29).
Subjective emotion
The patients with borderline personality disorder were more emotional than all other groups, consistent with the fact that a major criterion for the diagnosis of borderline personality disorder is emotional instability (DSM-IV). Conversely, the patients with orbitofrontal cortex lesions did not report being very emotional. These findings suggest that the higher level of emotionality of the patients with borderline personality disorder cannot be ascribed to orbitofrontal cortex dysfunction of the type produced by a lesion.
Reversal
Of all the study groups, only the patients with orbitofrontal cortex lesions had deficits on the reversal task
(5), and punishment insensitivity was a prominent feature in this group. It may be that patients with borderline personality disorder, who are in some ways hyperemotional, are actually more sensitive to reward and punishment and thus perform well on the punishment sensitivity task. A lower level of punishment sensitivity in the patients with orbitofrontal cortex lesions could lead to impulsivity because subjects with this characteristic may not care about the consequences of their actions. In borderline personality disorder subjects, increased sensitivity to punishment might make subjects more emotional, and the higher level of emotionality might then contribute to their impulsive behavior
(30).
Time estimation
The results suggest that the same underlying brain dysfunction, perhaps related to higher levels of frustration in waiting for the time to elapse, may cause both patients with borderline personality disorder and patients with orbitofrontal cortex lesions to underproduce time, although a different dysfunction, perhaps related to a greater cognitive pace
(5), may cause patients with orbitofrontal cortex lesions to overestimate time.
Conclusions
The results support the view that impulsivity, affective dysregulation, and personality abnormalities are core aspects of DSM-IV borderline personality disorder and that borderline personality disorder can be thought of in dimensional terms, with each patient having a unique neurobiological profile. Environmental and genetic factors may lead to brain alterations that result in specific presentations, such as self-harm
(31). An implication of the findings is that new light may be shed on the etiology of borderline personality disorder by considering how the syndrome can be fractionated and how different brain systems, each with different functions, contribute to the different symptoms of borderline personality disorder. The similarities and differences found between the patients with borderline personality disorder and the patients with orbitofrontal cortex lesions may lead to a better understanding of the functions of the orbitofrontal cortex, which could have implications for rehabilitation
(5,
21).
In support of the main hypothesis, the patients with borderline personality disorder had deficits that were similar to those of the patients with orbitofrontal cortex lesions and dissimilar to those of the patients with lesions outside the orbitofrontal cortex. One implication of this finding is that some of the core characteristics of borderline personality disorder, in particular impulsivity, are similar to the effects of orbitofrontal cortex damage, suggesting that orbitofrontal cortex dysfunction may contribute to some of the deficits in borderline personality disorder. On the other hand, the patients with orbitofrontal cortex lesions and the patients with borderline personality disorder performed differently on some tasks, suggesting that other characteristics of borderline personality disorder, such as high levels of emotionality and the borderline personality profile (high levels of neuroticism and introversion and a low level of conscientiousness), do not appear to be related to the type of dysfunctions produced by orbitofrontal cortex damage and are perhaps related to other brain systems (e.g., the limbic system). Patients with borderline personality disorder may have a neurochemical imbalance or a hyperactive/responsive amygdala
(10), which is not present in patients with orbitofrontal cortex lesions and which may exacerbate the emotional and personality disturbances of borderline personality disorder.
The orbitofrontal cortex, with its extensive reciprocal connections with the amygdala (which is implicated in emotional behavior [
32,
33]), may play a role in correcting/regulating emotional and behavioral responses
(1,
3,
4,
24,
34). Limbic-orbitofrontal circuit dysfunction may be involved in borderline personality disorder, at least in a subgroup of patients
(35). Borderline personality disorder may conceivably involve higher levels of limbic discharge, lower levels of orbitofrontal cortex function, and/or hypoactive frontolimbic circuitry. The findings reported here suggest that the orbitofrontal cortex is involved with the impulsivity evident in patients with borderline personality disorder. Our findings relate well to the hypothesis that the amygdala and orbitofrontal cortex act as part of an integrated neural system, as well as alone, in guiding decision making and adaptive response selection based on stimulus-reinforcement associations
(2,
10,
13,
32,
36).
In summary, patients with borderline personality disorder have some deficits that can be related to the functions performed by the orbitofrontal cortex. These deficits might be related to smaller volume of the orbitofrontal cortex or to lower levels of activity in the orbitofrontal cortex. Because patients with borderline personality disorder may be hypersensitive to reinforcers, positive feedback should be emphasized in rehabilitation. More studies are needed to investigate the involvement of the orbitofrontal cortex and amygdala in patients with borderline personality disorder, as these areas, in conjunction or in isolation, may contribute to some of the behavioral and emotional disturbances observed in these patients.