Anorexia nervosa is associated with serious medical complications and high mortality rates, and it often requires inpatient hospitalization. Studies have suggested that inpatient treatment may not be the most effective approach
(1). However, other studies have suggested that there are characteristics of hospitalizations that make them more or less effective and that some of those are changing in potentially detrimental ways. One such study examined inpatient hospitalizations for eating disorders over time and found increasing first admissions, total admissions, and readmissions and decreased lengths of stay
(2). Factors linked to poor treatment outcome include the following: long duration from illness onset to hospital admission
(3); inadequate inpatient weight gain, particularly during first hospitalizations
(3,
4); rapid inpatient weight gain; and periods of inpatient weight loss
(5,
6). Conversely, a period of weight maintenance before discharge may improve outcome
(6). The goals of this study were 1) to compare hospitalization practices for treating anorexia nervosa in the 1970s to those in the 1990s and 2) to assess whether any changes in hospitalization practices affected patient outcomes.
Method
Hospital charts were examined for all inpatients with eating disorders at the University of Minnesota Hospital and Clinic during 1975–1980 (early) (N=59) and 1990–1995 (later) (N=127). The subjects had a discharge diagnosis of anorexia nervosa and, to provide more diagnostic rigor, an admission body mass index ≤17.5 kg/m2 (ICD-10). Data collected included age, age at onset of eating disorder, length of admission, admission and discharge weights, height, comorbid diagnoses, and number of prior and subsequent hospitalizations at the University of Minnesota Hospital and Clinic. Admission and discharge body mass indexes and average rate of weight gain (lb/day) were calculated. The two cohorts were compared with independent-group t tests (when necessary, equal variance was not assumed) and chi-square tests. The variables associated with rehospitalization were determined with forward stepwise conditional logistic regression. Institutional review board approval was obtained before the study was initiated.
Results
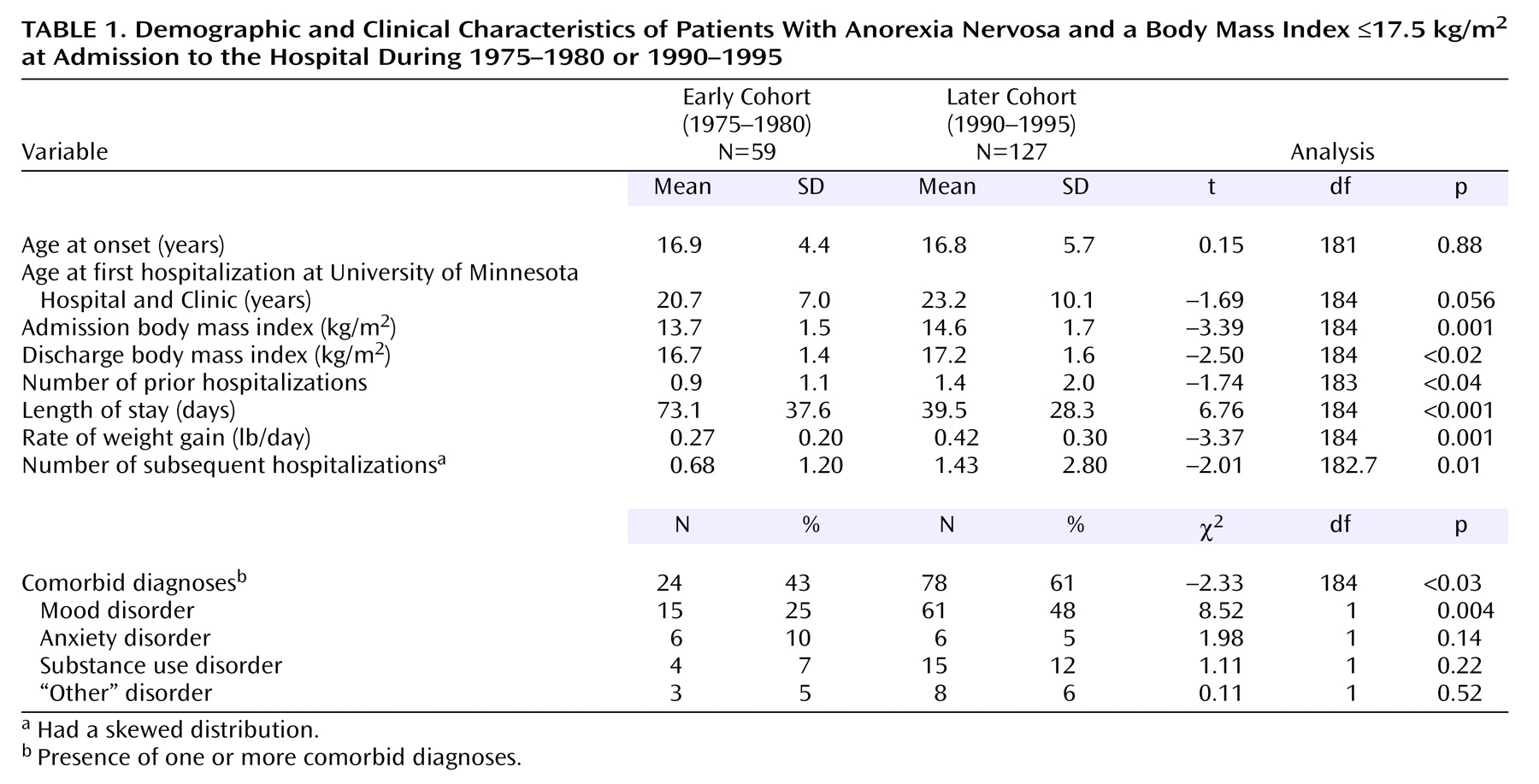
Demographic variables and comparisons between the cohorts are presented in
Table 1. No demographic variables differed significantly between the cohorts, except for a longer duration from illness onset to treatment (t=–2.28, df=163.52, p<0.03) and higher rates of comorbid diagnoses, both in the “later cohort.” Over time, the body mass index at admission increased, and the discharge body mass index decreased; both cohorts were discharged while still meeting the weight criterion for anorexia nervosa. Finally, length of stay decreased significantly, whereas the rate of weight gain and subsequent hospitalizations increased significantly.
To develop a model of variables associated with readmission, regression analyses were performed separately for each cohort with the following variables included as potential predictors of outcome: length of stay, rate of weight gain, body mass index at admission, body mass index at discharge, number of comorbid diagnoses, and presence of prior hospitalizations. In the “early cohort,” no variables were significantly associated with readmission. In the later cohort, three variables were significantly associated with rehospitalization: increased length of stay (B=0.022, Wald χ2=5.91, odds ratio=1.02, 95% confidence interval [CI]=1.00–1.04, p<0.02), more rapid rate of weight gain (B=1.716, Wald χ2=4.76, odds ratio=5.56, 95% CI=1.19–26.03, p<0.03), and having prior hospitalizations (B=1.505, Wald χ2=13.15, odds ratio=4.51, 95% CI=2.00–10.16, p≤0.001).
Discussion
This study suggests that hospitalization for anorexia nervosa changed between the 1970s and 1990s in ways that affect outcome. Patients in the 1970s stayed in the hospital longer and gained weight more slowly, and although they left at a lower discharge body mass index, they were less likely to be rehospitalized. By the 1990s, a more rapid rate of weight gain, having even one prior hospitalization, and longer lengths of stay were all associated with rehospitalization.
The association between longer hospital stays and rehospitalization in the later cohort was unexpected. Wiseman et al.
(2) found that a decreasing length of stay was concomitant with an increase in managed care; this is likely the case for our group, too. Thus, our findings may be attributable in part to changes in payment, which require that patients have a more chronic condition before they are allowed coverage for longer inpatient stays. This hypothesis is supported by further analyses showing that longer length of stay is correlated with more prior hospitalizations (r=0.24, p=0.007) and a lower body mass index at admission (r=–0.36, p≤0.001) but not the rate of weight gain or the number of comorbid diagnoses. Given the very high likelihood of readmission with prior hospitalizations, requiring more chronic anorexia nervosa before lengthier inpatient treatment, rather than intensive treatment when anorexia nervosa is first problematic, may not be the most cost-effective approach
(7).
In contrast to these results, one study found that slower weight gain is a negative outcome predictor
(8). The authors suggested that the effect of the rate of weight gain depends on the patient’s attitude toward treatment: if the patient is willing to gain weight, then rapid weight gain is a positive prognostic indicator; if the patient is resistant to treatment, slower weight gain is a negative indicator
(8). Therefore, for patients willing to gain weight, more rapid weight gain may be adequate; for those unwilling to gain weight, the high caloric intake required to achieve normal weight
(9) may require more gradual weight gain to address related psychological variables.
This study has several limitations. First, chart diagnoses were used rather than structured interviews. Therefore, a body mass index ≤17.5 kg/m2 at admission was added as an inclusion criterion. Other limitations include the differing lengths of follow-up and treatment philosophy changing over time (from behavioral to more cognitive-behavior oriented). However, these limitations should bias the results toward more readmissions in the early cohort (the opposite of these results).
These findings suggest that it is critical to maximize recovery in the first hospitalization for anorexia nervosa to prevent readmission. It appears that for those who are amenable to weight gain, a shorter inpatient stay with more rapid weight gain may be adequate. For those who are less psychologically amenable to treatment, a longer length of stay, a less rapid rate of weight gain, and a period of weight maintenance before discharge may be a more effective approach.