The criteria for substance use disorders have evolved greatly over the years, including important changes during the last two decades
(1–
4). In 1980, DSM-III continued the historical approach of focusing on physiological aspects of dependence, while DSM-III-R in 1987 broadened the concept to include elements of the dependence syndrome proposed by Edwards and Gross
(1,
5,
6). A parallel evolution in definitions of dependence occurred in ICD-10, with the result that the criteria are quite similar to those in DSM-IV
(7).
There has been more disagreement about the importance of the second, less intense, substance use disorder, a syndrome labeled as “abuse” in DSM and noted as “harmful use” in ICD-10. Historically, substance abuse was not introduced as a diagnosis until DSM-III, where it indicated the development of repetitive problems with alcohol when the difficulties did not include withdrawal or tolerance. Subsequently, the framers of DSM-III-R considered dropping abuse in light of the marked expansion of the scope of dependence but decided to maintain the category of abuse, which was defined as the presence of either of two specific dependence items (use in hazardous situations and continued use despite problems) in the absence of full-blown dependence
(1,
6,
8). Because the overlapping criteria for substance abuse and dependence made it difficult to evaluate the potential independence of the two labels, in 1994 DSM-IV defined abuse through repeated instances of at least one of four criterion items, including failure to fulfill major role obligations at work, school, or in the home; use in hazardous situations (e.g., driving while intoxicated); legal problems; and continued substance use despite persistent or recurrent related social or interpersonal problems in the absence of dependence
(1). The authors of ICD-10, however, pursued a different course, reserving the syndrome of harmful use for nondependent individuals who demonstrated physical or psychiatric alcohol-related problems.
Alcohol abuse appears to be moderately prevalent in the general population but, reflecting the less intense problems associated with alcohol abuse, compared to dependence, is not often seen among individuals entering treatment
(9–
11). The lifetime rate was estimated to be between 4% and 8% in a large national study and in regularly drinking individuals residing near New York City
(7,
9,
12). The lifetime prevalence of alcohol abuse is likely to be higher among individuals with family histories of alcoholism, although not all studies agree. A rate of approximately 15% was reported for 30-year-old men taking part in a prospective study of matched pairs of individuals with and without family histories of alcohol use disorders
(9,
12,
13). Most studies report higher lifetime rates of alcohol abuse among men than among women
(7,
14,
15).
Data are also available on the relationship between a diagnosis of alcohol abuse and the future risk for developing alcohol dependence. The follow-up of a group of more than 450 30-year-old men in San Diego revealed that only 11% of those with a lifetime diagnosis of alcohol abuse went on to develop alcohol dependence during the subsequent 5 years
(16,
17). Another general population study indicated a 1-year rate of 6% for conversion of alcohol abuse to alcohol dependence
(18). However, the rate of future alcohol dependence for those with abuse is not always higher than for comparison subjects with no baseline alcohol use disorder
(9,
17).
Individuals with alcohol abuse are likely to continue to have alcohol-related problems over time. In the San Diego Prospective Study, almost 50% of men with alcohol abuse at age 30 years continued to meet the DSM-IV criteria for that disorder over the next 5 years, a rate of problems that was significantly greater than the 15% risk for abuse onset for those with no diagnosis at baseline and less than the 63% rate for repetitive problems for those with alcohol dependence
(16). A 1-year follow-up of another group of subjects reported that 27% of those with alcohol abuse still maintained that diagnosis 1 year later, a rate that was six times higher than for comparison subjects without alcohol abuse at baseline
(9,
18). Data from the six-center Collaborative Study on the Genetics of Alcoholism indicated that 55% of individuals with a lifetime diagnosis of alcohol abuse at initial evaluation continued to meet the criteria for abuse during a 5-year follow-up
(17).
The coherence and distinctive nature of the criteria for alcohol abuse have been supported by most factor analytic studies that included both abuse and dependence items
(19–
22). In addition, the clinical characteristics of individuals with alcohol abuse have been compared to those with no diagnosis or to those with alcohol dependence; typically the parameters relating to abuse tended to fall midway between the two extremes
(3,
7,
23). These parameters include indicators of the usual quantity and frequency of drinking, histories of having received prior treatment for alcohol use disorders, and the rates of alcohol-related problems (e.g., blackouts) that are not part of the alcohol abuse criteria.
The test-retest reliability of alcohol abuse diagnoses tends to be lower than that for alcohol dependence, with kappas for abuse generally around 0.5
(10,
11,
24–26). Finally, regarding validators, several investigators have compared the diagnostic concordance between DSM-IV and ICD-10 alcohol diagnoses and have reported high levels of similarity for the diagnostic criteria for alcohol dependence, but much lower rates for abuse versus harmful use
(12,
27). The latter finding is not unexpected in light of the large differences in how abuse and harmful use are defined across the systems, compared to the marked similarities of the criteria for dependence.
Few investigations have evaluated the relative performance of individual DSM-IV alcohol abuse criteria. Most reports indicate that the majority of individuals with abuse are likely to endorse only one of the four relevant DSM-IV items; in more than two-thirds of cases this item is criterion 2, repetitive use of alcohol in hazardous situations, such as driving after drinking
(12,
16,
27). There may be differences between individuals who endorsed only the item related to driving while intoxicated, compared to those who relate histories of other abuse items. According to one study, the former are more likely to be older, to have used drugs, to have relatives with alcoholism, and to have received treatment
(12). However, whether defined by driving while intoxicated or by other criterion items, a diagnosis of alcohol abuse was equally related to the persistence of alcohol-related problems and to the chances of developing dependence.
Our research group has reported data regarding the 5-year course and clinical correlates associated with each of the seven alcohol dependence criteria in the Collaborative Study on the Genetics of Alcoholism sample
(28). For comparison, additional information was presented regarding the diagnosis of alcohol abuse, including the finding that more than three-quarters of subjects with this diagnosis (in the absence of dependence) endorsed only one criterion. The analysis also supported the high prevalence of hazardous use (in 92% of those with abuse), compared to interference with social functioning (23.1%), impaired role functioning (6.8%), and alcohol-related legal problems (1.6%). However, that study did not evaluate the performance of a diagnostic threshold of one versus two or more abuse criteria for a diagnosis, a question of some importance as the latter is more consistent with the DSM-IV emphasis on syndromes. Furthermore, few, if any, studies have compared the relative performance of each of the four abuse diagnostic items or evaluated any combinations of criteria regarding cross-sectional characteristics or future course. This report evaluates aspects of the DSM-IV category of abuse. We relate data from an expanded Collaborative Study on the Genetics of Alcoholism sample, focusing on a comparison across the four abuse items and an evaluation of the relative attributes of a diagnostic threshold of one versus two or more endorsed criteria.
Method
All subjects gave informed consent to participate in the protocol in accordance with Collaborative Study on the Genetics of Alcoholism procedures approved by human subjects committees at the universities involved. The original probands were alcohol-dependent individuals from alcohol and drug treatment programs at each of the six original centers who were selected if they met both the DSM-III-R dependence criteria and the Feighner alcoholism criteria, regardless of the presence of additional psychiatric diagnoses
(17,
28,
29). For ongoing participation, probands were required to have multiple family members with alcoholism; additional exclusions were an inability to speak English, the presence of a severe medical condition, and recent heavy intravenous drug use. Comparison subjects were selected by using different methods across centers, including random searches of driver’s license records, advertisements in general medical and dental clinics, and mailed questionnaires.
At entry into the protocol, all initial subjects were evaluated with the Semi-Structured Assessment for the Genetics of Alcoholism interview
(30,
31). Using this valid and reliable instrument
(30,
31), trained personnel asked about 17 DSM-III-R axis I diagnoses and recorded details about the clinical course of alcohol- and drug-related problems. The same interview was used to gather appropriate information for satisfying other diagnostic criteria for substance use disorders, including the DSM-IV criteria. Family history data were recorded through the family history assessment module of the Semi-Structured Assessment for the Genetics of Alcoholism. This module focuses on an individual’s report about substance use syndromes and psychiatric conditions among close and more distant relatives
(32). The same procedures were repeated through direct evaluations of available first- and second-degree relatives.
Five years after enrollment in the study, all original probands and comparison subjects, younger offspring in the families, and appropriate additional relatives were recontacted. Approximately 70% of those who were contacted agreed to participate (with rates ranging from approximately 60% to 80% in different centers). The follow-up evaluation used a slightly modified Semi-Structured Assessment for the Genetics of Alcoholism instrument that gathered additional details about substance use, related problems, and psychiatric syndromes occurring during the interval since initial evaluation.
As of January 1, 2003 (master file 128), follow-up evaluations had been completed for 4,313 subjects (including probands, comparison subjects, and relatives) age 18 years or older. This group included 1,528 individuals who fulfilled the criteria for DSM-IV alcohol dependence at the initial interview and an additional 189 persons who met the criteria for antisocial personality disorder. Because early-onset repetitive antisocial behaviors are associated with a more severe clinical course of alcohol-related difficulties, and based on our focus on the clinical course of alcohol abuse, subjects with either alcohol dependence and/or antisocial personality disorder were excluded from the analyses. The remaining 2,596 men and women either met the criteria for alcohol abuse or demonstrated no alcohol use disorder at intake.
The subjects were assigned to one of several groups on the basis of their endorsement, at baseline, of repetitive (i.e., three or more) experiences with at least one of the four DSM-IV alcohol abuse criterion items. For all data tables, group A included 1,881 individuals (72.5%) who did not manifest alcohol abuse at intake. Group A subjects were compared with the remaining persons, who were assigned to groups on the basis of whether they met any one of the four abuse criteria, regardless of their endorsement of any other items. We also explored the implications of having endorsed each of the four abuse criteria but focused on the subjects who reported only one criterion item, as these subjects represented the majority of persons with abuse.
Statistical comparisons across groups were carried out by using chi-square tests for categorical data, and continuous variables were compared across groups by using t tests or analysis of variance, with Tukey’s or Dunnett’s post hoc analyses, where appropriate. Multiple regression analyses were conducted to evaluate the combination of baseline characteristics and diagnostic items that best predicted outcomes.
Results
The 2,596 subjects included 785 men (30.2%) and 1,811 women (69.8%), reflecting the higher rate of exclusion of men for antisocial personality disorder and alcohol dependence. Only 0.4% of the subjects were original probands with DSM-IV alcohol abuse who had originally fulfilled the criteria for the less restrictive DSM-III-R diagnosis of alcohol dependence, 70.5% were relatives of probands, and the remainder were from comparison families. Overall, the subjects were a mean of 37.7 years old (SD=13.6) and had 13.5 years of education (SD=12.1).
Among the 715 individuals with a lifetime history of alcohol abuse at the time-1 interview, 565 (79.0%) met only one abuse criterion, 132 (18.5%) endorsed two criteria, 18 (2.5%) endorsed three criteria, and none endorsed all four criteria. Regarding the specific criteria, criterion 1 (role interference) was endorsed by 56 individuals (2.2% of the 2,596 subjects overall and 7.8% of those with alcohol abuse), criterion 2 (hazardous use) was reported by 653 (25.2% of the total population and 91.3% of those with abuse), criterion 3 (legal problems) was noted by nine (0.3% of the total and 1.3% of those with abuse), and 165 endorsed criterion 4, social problems (6.4% of the entire population and 23.1% of those with abuse). These proportions add up to more than 100% because subjects could endorse more than one item.
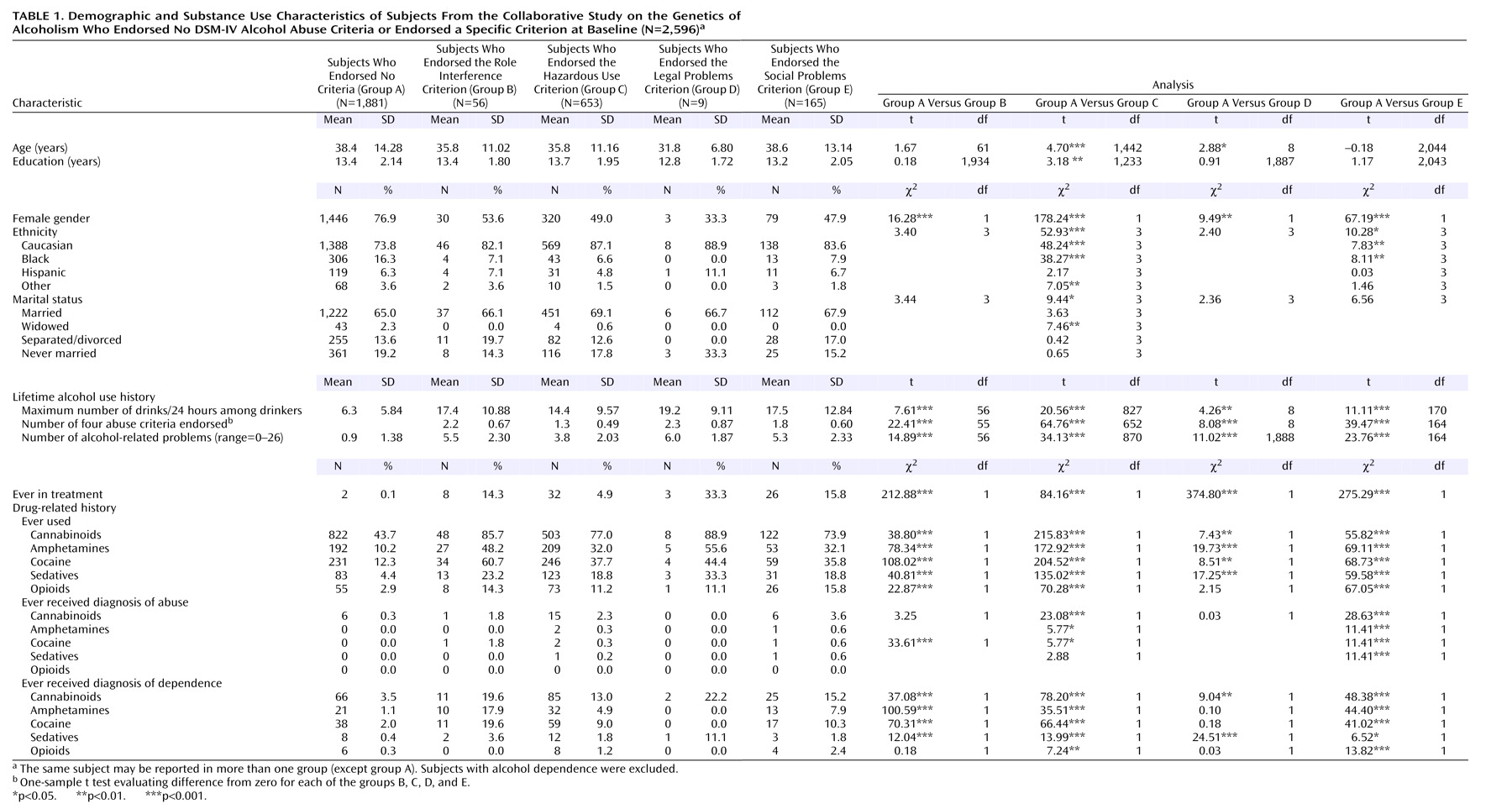
Table 1 reports the baseline demographic characteristics as well as the lifetime alcohol- and other substance-related histories (i.e., clinical validators) for five groups structured to reflect whether an individual reported ever having repeatedly (i.e., three or more times) experienced one of the four DSM-IV abuse criteria. Reflecting the manner in which the groups were structured, the statistical analyses compared subjects who endorsed each diagnostic criterion with group A (subjects with no baseline abuse). Because subjects could endorse more than one abuse criterion, groups B, C, D, and E are not statistically independent and thus pairwise group comparisons were made. For the multilevel variables of ethnicity and marital status, an overall group comparison was conducted first, with individual levels (e.g., black, Caucasian) evaluated only if the overall statistic was significant. There were a number of group differences in demographic characteristics, including younger ages for subjects who endorsed hazardous use (group C) and legal problems (group D), compared to those with no abuse diagnosis at baseline (group A), and higher levels of education for subjects who endorsed hazardous use. Not unexpectedly, the proportions of women were lower in groups B, C, D, and E, compared to group A. Differences in ethnicity in comparisons with group A were observed for those with hazardous use or social problems, with groups C and E including a higher proportion of Caucasians than group A. There were few noteworthy differences on marital status.
Table 1 also reports the group comparisons in relation to alcohol and drug intake patterns and alcohol problems at baseline. Here, as might be expected, subjects who endorsed each of the four abuse criteria had higher levels of alcohol intake and related problems as well as prior experience with alcohol-related treatment, compared to subjects in group A. The 26 alcohol-related problems included items that either were not part of the diagnostic criteria for alcohol abuse or dependence or were alcohol-related difficulties that occurred less frequently than three times. Higher rates for subjects who endorsed each abuse criterion, compared to group A, were noted for most categories of drug use, abuse, and dependence.
These analyses were repeated after subjects who endorsed more than one criterion item were excluded. The remaining 565 subjects constituted 79.0% of the subjects reported on in
Table 1, including 12 persons in group B, 506 in group C, two in group D, and 45 in group E. Because of the small number of subjects with abuse at baseline who had only legal problems, group D was not included in these analyses. An overall statistical comparison across all four of these independent groups was conducted, with post hoc analyses used only if the overall comparison was significant.
The evaluations of subjects who endorsed only one abuse item supported the general conclusions noted for the data reported in
Table 1. Regarding age, group C (mean=35.0 years, SD=10.9) and group B (mean=29.3 years, SD=4.5) were younger than group A (mean=38.4 years, SD=14.3) and group E (mean=40.1 years, SD=14.96) (F=7.97, df=3, 2140, p<0.001), with post hoc analyses revealing differences for A versus B, B versus C, and B versus E. More years of schooling were reported for group A (mean=13.4, SD=2.1) and group C (mean=13.8, SD=2.0), compared to group B (mean=12.1, SD=1.88) and group E (mean=13.2, SD=2.14) (F=7.45, df=3, 2439, p<0.001), with post hoc differences for A versus B, B versus C, and B versus E. The proportions of women were lower for groups A (76.9%), C (51.2%), and E (71.1%), compared to group B (91.7%) (χ
2=131.59, df=3, p<0.001), with post hoc analyses supporting differences for A versus C, B versus C, and C versus E. Ethnic differences across groups were significant overall (χ
2=56.19, df=3, p<0.001), reflecting a higher proportion of Caucasians in group C (87.2%), compared with 66.7%–73.7% in the remaining groups, with significant post hoc differences between group C and the remaining groups. Regarding baseline alcohol use, all parameters continued to support the lowest rates of alcohol problems in group A (group A: mean=0.9, SD=1.4; group B: mean=4.3, SD=2.2; group C: mean=3.3, SD=1.6; and group E: mean=3.5, SD=1.5) (F=400.02, df=3, 2440, p<0.005), with significant post hoc differentials for group A versus each other group, as well as for B versus C and B versus E. A similar differential was seen for maximum number of drinks in 24 hours (group A: mean=6.6, SD=5.8; group B: mean=11.8, SD=7.0; group C: mean=13.1, SD=7.7; and group E: mean=13.1, SD=9.9) (F=146.70, df=3, 2341, p<0.001), but post hoc tests supported only the differences between group A and each of the remaining groups. Values for history of drug intake were also lowest for group A overall, and post hoc tests revealed that the only significant additional differential occurred for cocaine use, reported by 12.3% of group A, 58.3% of group B, 35.6% of group C, and 24.4% of group E. A post hoc difference was noted for group B versus group E.
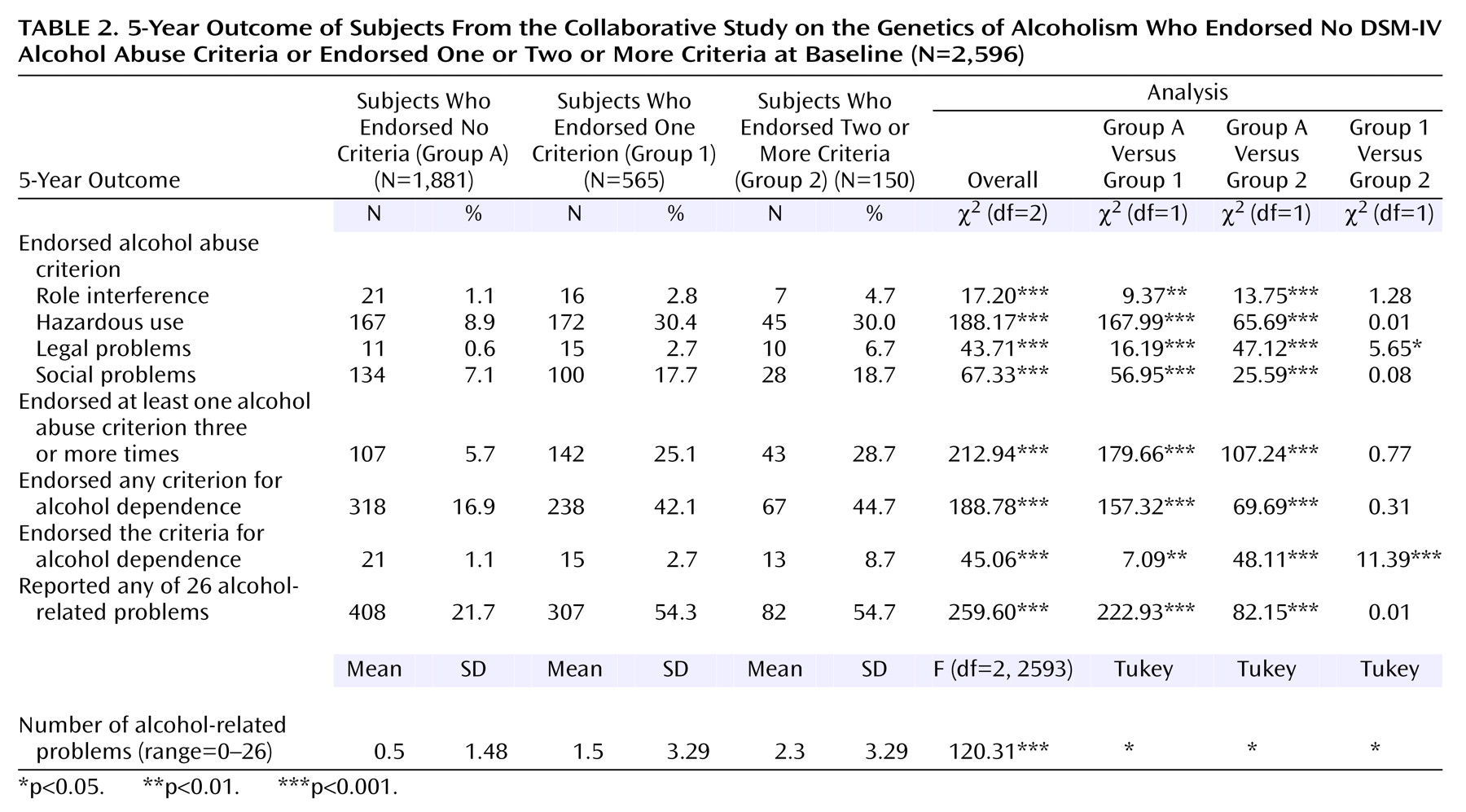
Table 2 compares the 5-year course for subjects who endorsed one abuse criterion (group 1: 565 subjects) versus two or more criteria (group 2: 150 subjects) at the time of the initial interview, in relation to the 1,881 subjects with no baseline alcohol abuse criteria endorsements (group A). Subjects who endorsed one criterion at baseline and those who endorsed two or three criteria differed from members of group A in almost all outcomes. At the 5-year interview these outcomes included experiencing each of the four abuse criteria at least once during the 5-year follow-up, continuing to meet the full criteria for abuse, having endorsed one or more dependence criteria, meeting the full criteria for dependence at some point during the follow-up, experiencing one or more of the 26 additional alcohol-related experiences during the follow-up, and having a higher mean number of the 26 problems. The final column in
Table 2 reports a direct comparison of groups 1 and 2. The lack of significant difference for most outcomes supports the general equivalence of each threshold in predicting the alcohol-related outcomes assessed. Exceptions were the greater likelihood for group 2 to report legal problems or dependence and the greater number of the 26 problems reported by group 2. The outcomes for men and women were generally similar (data not shown).
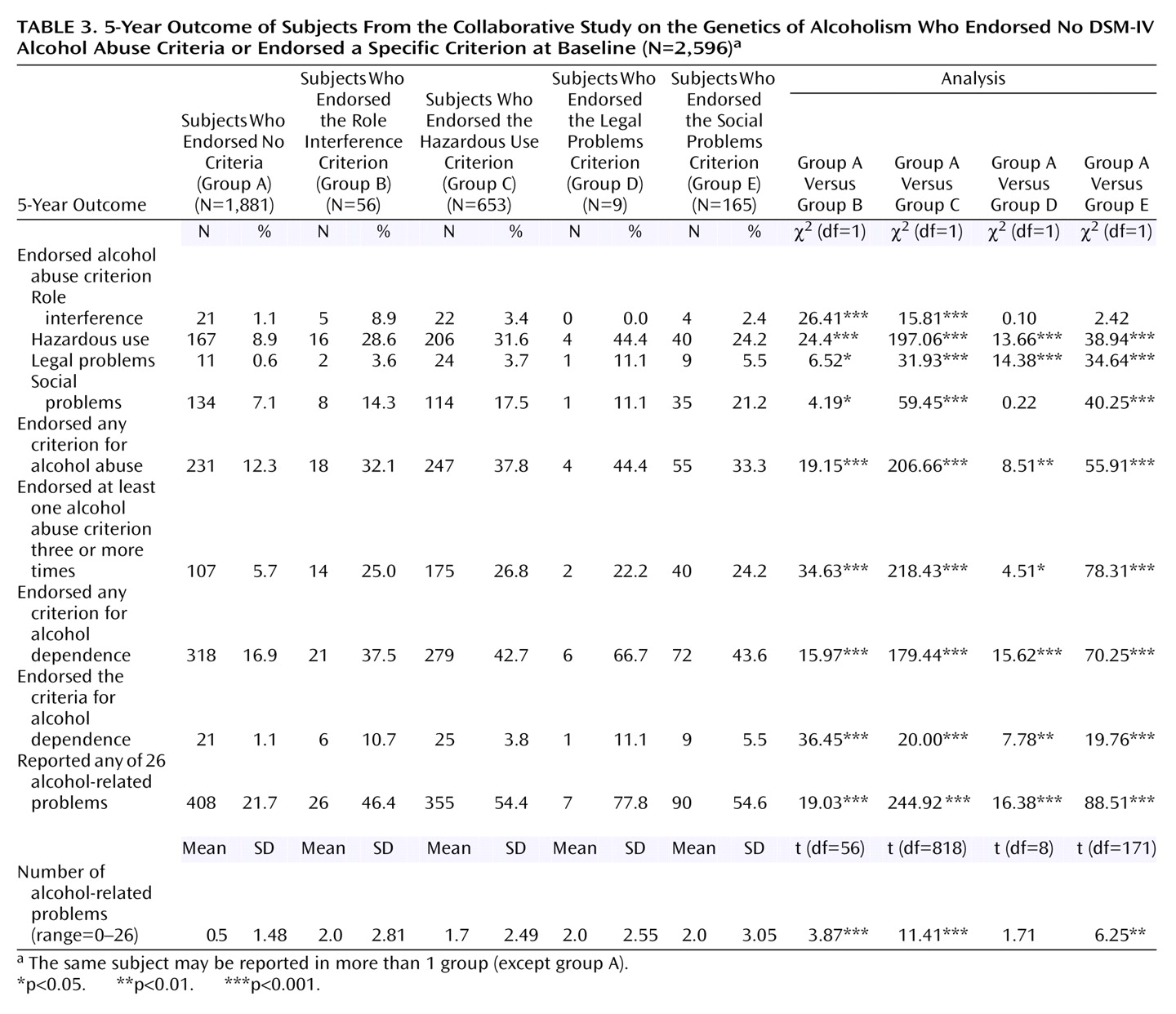
Table 3 presents the 5-year follow-up outcomes for the groups presented in
Table 1, which were based on whether a subject had endorsed any DSM-IV abuse criterion at baseline, regardless of what other criteria were reported. Because the same person might have endorsed more than one item (i.e., groups B, C, and E are not independent), statistical analyses compared results for subjects who endorsed each criterion with the subjects who reported no alcohol abuse at baseline (group A). For all outcome measures, the reports of the alcohol-related role interference group (group B) and the hazardous use group (group C) were associated with different 5-year outcomes, compared to those with no baseline criterion endorsements. This difference was generally significant for both men and women (data not shown), except for the rate of the development of dependence during the follow-up, which was in the same direction for both men and women but was not different from the rate for subjects of the same gender in group A. The endorsement of social problems at baseline (group E) also predicted a more problematic outcome overall, with similar results in each gender for most items. Evaluation of outcomes associated with the endorsement of legal problems was made tenuous by the small number of subjects in that category, although most outcomes for those subjects were significantly worse, compared to outcomes for group A.
The analyses reported in
Table 3 were repeated for the subjects who endorsed none or only one abuse criterion when first evaluated. Although this step facilitates the comparison of the relative performance of each item, it was necessary to omit the data for the two subjects who had reported legal problems as a sole criterion at intake. Similar to results reported in
Table 3, the overall evaluations across the four remaining groups were all significant. Post hoc results indicated that outcomes for subjects with hazardous use (group C) were different from those in group A for all outcome items, while those with only role interference (group B) or social problems (group E) at baseline were different from those in group A on most items. Although the numbers of male and female subjects were often too small for meaningful comparisons, group differences were generally similar for the two genders.
Because the utility of the hazardous use criterion as the sole diagnostic item has been questioned in the literature
(12), the analyses also explored the relative ability of this criterion at baseline to predict outcome, compared to the two other diagnostic criteria. In general, in these evaluations of subjects who had endorsed none or only one of the abuse items at time 1, hazardous use performed in a similar manner to the other criteria, with the exception of follow-up endorsement of hazardous use, which was more likely in group C (32.2%) than in the combined groups B and E (19.3%) (χ
2=5.06, df=1, p<0.05).
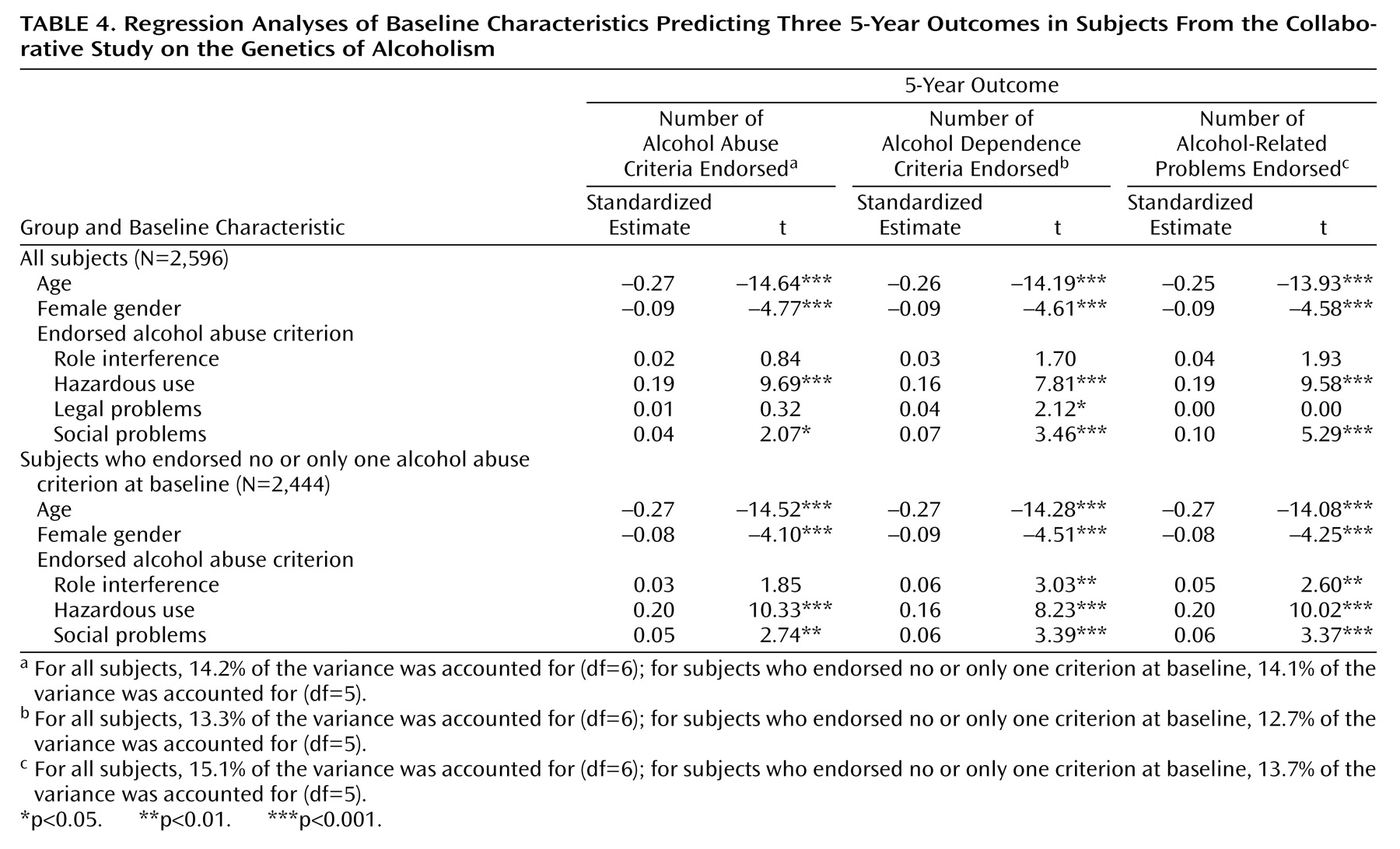
The data were also used to explore the overall performance of DSM-IV abuse items when used together in the context of gender and age. The results of three regression analyses involving data for all 2,596 subjects are reported at the top of
Table 4. In these analyses, baseline data were used to individually predict: 1) the number of abuse items endorsed at least once during the 5-year follow-up, 2) the number of dependence items reported, and 3) the number of 26 additional substance-related problems reported. Simultaneously entered into each regression were age, female gender, and whether or not at baseline the individual had indicated repetitive (i.e., three or more times) problems with each of the four alcohol abuse items. Both younger age and gender contributed significantly to all three regression equations, as did time 1 hazardous use and social problems. Legal problems at baseline were significantly related to the number of alcohol dependence items observed during the follow-up, but alcohol-related role interference did not contribute to any of these regressions. The three equations each explained between 13.3% and 15.0% of the variance in the three outcomes. These analyses were repeated by using data for the 2,444 individuals who either had no alcohol abuse at baseline or who endorsed only one abuse criterion. The results, presented in the bottom part of
Table 4, were similar to those reported for the full sample. The one exception was that role interference contributed to prediction of both the number of dependence items and the number of the 26 miscellaneous alcohol-related problems that were reported. The proportions of the variance explained ranged from 12.7% to 14.1%.
Discussion
Alcohol abuse is a moderately prevalent disorder that is associated with higher levels of alcohol intake and with an enhanced risk for future alcohol-related difficulties. As defined in DSM-IV, this label appears to be a relatively independent diagnosis, with fewer than 10% of those with abuse developing dependence
(9,
17,
18).
A unique aspect of DSM-IV alcohol abuse is that, although repetitive problems in a given area are required, abuse might not be considered a syndrome by some because only one of four potential diagnostic criteria must be present. Consistent with our results, most studies indicate that 70%–80% of those with abuse only endorsed repetitive problems in one area
(12,
16,
27). However, few investigations have evaluated the relative performance of a threshold of one of four potential items endorsed versus two or more. Our analyses describing several types of 5-year outcomes for subjects with one versus two or more abuse criteria at baseline generally support the conclusion that both thresholds are associated with higher risks for each outcome, relative to the presence of no criteria at baseline. However, subjects who endorsed two or more items reported a higher number of potential problems during the follow-up, were more likely to encounter legal difficulties, and were three times more likely to go on to develop alcohol dependence. Because one might expect that the more items endorsed at time 1, the greater the likelihood of future problems would be, the overall similarity of groups 1 and 2, as shown in
Table 2, was a bit surprising.
Recognizing that almost 80% of the subjects with abuse endorsed only one criterion and that repetitive problems in only one area were associated with a greater risk for alcohol problems over the next 5 years, we suggest that maintaining the diagnostic threshold at one criterion would be appropriate. Although subjects with more problems at baseline had a higher risk of future alcohol dependence, it might be more clinically relevant to continue to use a threshold of one item in order to identify a much larger group of individuals at risk for future problems.
The current study is also one of the few studies to evaluate the cross-sectional relationships and prognostic values associated with each of the diagnostic criteria for abuse. At baseline, individuals with any of the four criteria were found to have higher cross-sectional levels of alcohol intake and use of illicit substances and associated problems. Furthermore, each diagnostic criterion was also associated with an enhanced risk for future problems, and these generalizations held for both men and women regardless of the endorsement of other criteria. These results are consistent with prior investigations that have examined the ability of an abuse diagnosis overall to predict both cross-sectional and future clinical problems
(3,
16,
18).
One diagnostic criterion, use in hazardous situations, stands out because of its exceptional rate of endorsement in this and other studies
(12). The high prevalence of this item has led some investigators to question whether patients who endorse hazardous use as their only diagnostic criterion might differ from those who note the experience of repetitive problems in other diagnostic areas. One prior study indicated that the sole endorsement of hazardous use was likely to occur in individuals who appeared to be more stable, older, more likely to be married, and less likely to have had problems with other drugs
(12). However, in the current study, hazardous use appeared to perform as well as the other diagnostic criteria for abuse. Subjects endorsing this criterion tended to be in the mid-range for age, were not more likely to be married, and were not significantly less likely to have a drug use disorder. The only indication of possible enhanced life stability was a higher level of education for those subjects. Most important, subjects who endorsed only hazardous use at baseline had a risk for future problems that was similar to those who endorsed the two other more prevalent items (role interference or social problems). Therefore, hazardous use appears to have performed relatively well both cross-sectionally and longitudinally within this investigation. The disparity in findings, compared with the earlier report, might reflect the inclusion of different study populations, as the subjects in the Collaborative Study on the Genetics of Alcoholism are generally less educated, have lower levels of job skills, and come from families with high concentrations of alcohol use disorders, relative to other groups of persons with alcohol use disorders
(33).
The presence of legal problems is another specific DSM abuse criterion that stands out, but in this instance because of a low rate of endorsement. When evaluated in the context of other criteria, the nine subjects with legal problems at baseline reported relatively high rates of future problems and differed on all outcomes from those with no baseline abuse symptoms. However, seven of the nine subjects with this item also endorsed other criteria and would have been identified as having alcohol abuse even if legal problems had not been part of the definition of abuse. Thus, the importance of this criterion for future definitions of abuse is not clear from the current study, and more work in additional subject groups is required.
The data reported here also allowed the evaluation of combinations of abuse criteria. Despite the relatively large sample, only 20% of the subjects with abuse had endorsed more than one criterion. Thus, analyses focused on comparing subjects with hazardous use with the two other most populous groups combined. The results do not highlight any specific combination of criterion items that are clearly superior to any other.
Our data indicate a higher rate of alcohol abuse than had been noted in other studies. Almost 28% of the entire group met the criteria for alcohol abuse, compared to less than 10% in several studies of the general population and compared to a lifetime risk of about 15% in a highly functional group of families, half of which had histories of alcohol dependence
(7,
9,
12,
13). This high rate of alcohol abuse occurred despite the fact that the diagnosis required repetitive occurrence for an endorsement of a criterion item. Perhaps the rate of abuse reported here reflects the recruitment requirement that families continuing in the Collaborative Study on the Genetics of Alcoholism have a relatively high density of alcohol abuse or dependence, the use of lay interviewers who might not screen out less serious problems, or the fact that prior studies of the general population tended to use DSM-III-R criteria while this report focused on DSM-IV criteria.
The analyses reported here considered the performance of each of the four DSM-IV abuse criteria in a specific population. They were not structured to address the broader question of whether the concept of a second, less severe substance-related syndrome (abuse) is justified overall in DSM-IV. Nor did the evaluations turn to the broad and complicated question of whether DSM-IV diagnoses should be dimensional or categorical. A dimensional approach (e.g., listing a large number of criterion items and recording the number endorsed) has the asset of using a full range of information but the liability of not addressing the need to develop relatively straightforward syndromes that can be used for treatment or reimbursement decisions. It seems likely that a dimensional diagnosis would in reality be converted by clinicians and administrators into score-based categories that might not be greatly different from those used in the current categorical approach. Of course, limiting diagnostic categories to abuse and dependence has its own difficulties, not the least of which involves the cases of individuals who endorse one or two dependence items but who do not meet the criteria for abuse (diagnostic “orphans”)
(34). These issues and many others are being addressed in additional analyses and are important potential considerations for the DSM-V process.
These considerations underscore the need to note several caveats in interpreting the current results. The most important caveats relate to the unique aspects of the Collaborative Study on the Genetics of Alcoholism families, including the fact that the original alcoholic proband was an inpatient in treatment for alcoholism, the general blue-collar culture of the group, and the high density of alcohol use disorders. Also, the Collaborative Study on the Genetics of Alcoholism is a study of families, and the results might have been affected by the nonindependence of relatives. It may also be relevant that only a diagnosis of alcohol abuse was evaluated, and no data are offered regarding abuse of other substances. In addition, diagnostic symptoms were evaluated by nonclinical interviewers across six different centers, and it is possible that clinician interviewers might have documented a different rate of abuse by placing more or less emphasis on the clinical relevance of the reported problems.
Nonetheless, this report is among the first to evaluate the clinical relevance of each of the diagnostic criteria for alcohol abuse and to compare a threshold of one versus two or more abuse problems in establishing a diagnosis. Although more research is needed in different populations and across different drugs of abuse, these findings offer general support for the clinical usefulness of the criteria for alcohol abuse in DSM-IV.