The Remission in Schizophrenia Working Group was convened in April 2003 to develop a consensus definition of remission as applied to schizophrenia. The need for such a definition is timely because of recent insights into and expectations around the long-term course of schizophrenia, including the evolution of psychosocial and pharmacological therapies for psychotic disorders, variable definitions of treatment outcome in schizophrenia, and evidence that traditional predictions of generally poor outcome may have been overstated. In addition, the potential utility of a consensus definition of remission in schizophrenia has been reinforced by the successful application of remission and recovery concepts to the treatment of patients with mood and anxiety disorders.
The working group sought to develop operational criteria for remission, using as a model consensus work in mood and anxiety disorders conducted over the past decade
(1–
3). In this consensus, remission was defined by using an absolute threshold of severity of the diagnostic symptoms of schizophrenia, rather than percentage improvements from a particular baseline. This shift in characterizing improvement through means of threshold criteria will permit direct cross-trial comparisons. The real-world interpretability of change scores as a primary outcome measure is limited because of the variability of baseline symptom intensity across interventional trials. Specifically, the proposed remission criteria define remission as a low-mild symptom intensity level, where such absent, borderline, or mild symptoms do not influence an individual’s behavior. Such symptom thresholds have sometimes also been augmented by functional improvement criteria in a variety of previous definitions of remission or recovery in schizophrenia
(4–
7), but this working group chose to focus solely on symptomatic remission for reasons described subsequently.
Precedents for remission criteria exist for both psychiatric and nonpsychiatric illnesses. Traditionally, remission criteria in nonpsychiatric illnesses have been characterized by the abatement of disease symptoms. For example, complete remission in non-Hodgkin’s lymphoma requires the patient to be in normal health without evidence of lymphoma, with no lymph nodes larger than 1.5 cm in the long axis on computerized tomography scans, although this node size is larger than normal in a person without lymphoma
(8). Similarly, remission in rheumatoid arthritis is defined as the absence of fatigue, as well as negligible morning stiffness, and a lack of joint pain, tenderness, and soft tissue swelling, accompanied by a normal erythrocyte sedimentation rate
(9). Comparatively, remission may be characterized by the complete absence of symptoms in illnesses for which treatment is clinically oriented toward “cure,” versus illnesses for which treatment is oriented toward “remission-recovery” as the clinical goal.
In the case of noncurable, progressive illnesses with psychiatric and nonpsychiatric components, such as multiple sclerosis, consensus on remission as an absence of symptoms has not been achieved. Here, the majority (85%) of “relapsing-remitting multiple sclerosis” is termed secondary-progressive multiple sclerosis, where remissions are often associated with some symptomatic residual dysfunction
(10). To date, remission in psychiatric illnesses, such as anxiety disorders, has been objectively defined not by the complete absence of anxious or depressive symptoms but rather by minimal symptoms with mild disability
(11). One consensus challenge regarding remission in schizophrenia surrounds the recognition that although the symptoms of many anxiety and depressive disorders coexist with normal life experience, the commonly recognized symptoms of schizophrenia lie outside this experience. However, there is some evidence for the continuity of psychotic symptoms (e.g., delusions and hallucinations) with “normal” experience
(12,
13), and negative symptoms (e.g., avolition, alogia) clearly are on a continuum with normality.
In recent years there has been an appropriate increase in emphasis on clinical outcomes that are meaningful to patients, families, and clinicians, as well as a greater focus on functional recovery. For a disorder such as schizophrenia, complete recovery implies the ability to function in the community, socially and vocationally, as well as being relatively free of disease-related psychopathology. Recovery is conceptualized, therefore, as a more demanding and longer-term phenomenon than remission, consistent with the work of various research groups
(7,
14). Remission is a necessary but not sufficient step toward recovery. The working group chose to define remission as a state in which patients have experienced an improvement in core signs and symptoms to the extent that any remaining symptoms are of such low intensity that they no longer interfere significantly with behavior and are below the threshold typically utilized in justifying an initial diagnosis of schizophrenia. The working group struggled with the decision of whether the complete absence of any core signs and symptoms should be required, but on balance the group felt that the proposed threshold described herein was the most appropriate, on both clinical and heuristic grounds.
Consensus regarding operational criteria for recovery, which might include improvements in cognition or psychosocial functioning, was considered outside the scope of the working group, because more research is needed on this topic. As mentioned earlier, such criteria are the focus of ongoing multidisciplinary efforts seeking to incorporate the viewpoints of patients, caregivers, and clinicians
(7), as well as an evolving appreciation for the relationship between improvements in symptoms, cognition, and functionality. Because cognitive impairments in schizophrenia are of a continuous nature (in contrast to the episodic intensity of psychotic symptoms) and because the association of specific symptoms with specific cognitive deficits remains under active investigation, it is not yet possible to incorporate an extensive knowledge base regarding psychosocial or cognitive dysfunction into definitions of remission or recovery in schizophrenia.
Remission Criteria in Mood and Anxiety Disorders
In developing criteria for remission in schizophrenia, the working group used as a model the development of criteria for disease state and change criteria in mood and anxiety disorders, particularly major depressive disorder. Early clinical trials of antidepressant therapies were characterized by inconsistent definitions of change criteria, leading in turn to inconsistent evaluations of therapeutic approaches
(1). The development of the Hamilton Depression Rating Scale in 1960, its refinement over succeeding years, and its gradual incorporation as a standard measure in clinical trials provided clinical researchers with a consistent tool to assess change in symptoms over time
(14). However, despite the use of standardized, validated rating scales for symptom and disease severity, inconsistent use and application of terms such as recurrence, relapse, response, remission, and recovery remained widespread. Response, in particular, was used as the defining measure of treatment efficacy in clinical trials of most new pharmacological agents, resulting in a therapeutic focus on short-term improvements and providing little guidance to clinicians regarding long-term disease management.
Recognizing the clinical need for consistency in defining outcomes, particularly for chronic mental illness, a task force on the psychobiology of depression was convened by the MacArthur Foundation in 1988 to evaluate historical descriptions of change criteria and to develop internally consistent, empirical definitions, as well as operational criteria, for response, remission, and recurrence in major depressive disorder
(1). This effort was based on a “conceptualization” approach that moved from the recognition of change criteria as a valid construct, through definitions of these change criteria, to operational criteria for their assessment
(1). In addition to developing definitions for these clinical concepts, this task force suggested methods through which their utility could be assessed, including reanalysis of existing data and prospective studies using outcomes guided by the new criteria
(1).
The task force examining major depressive disorder incorporated criteria for both disease severity and duration of improvement and suggested that the instruments used for symptom severity assessments be test-retest reliable, easily completed in a clinical setting, and able to provide value in establishing a prognosis for future disease course
(1). The task force proposed a definition for remission, based on the 17-item Hamilton depression scale total score, as maintenance of an endpoint score of ≤7 for at least 2 but less than 6 months. To facilitate broader acceptance of the remission concept, criteria based on the Schedule for Affective Disorders and Schizophrenia and the Beck Depression Inventory were also proposed.
During the past decade, the definition of symptomatic remission in major depression has been incorporated into clinical studies of treatment efficacy, confirming that remission is a more stringent standard than response and suggesting that remission can be used in conjunction with, or even to replace, other outcomes in efficacy evaluations
(15). In addition, the remission concept has facilitated comparisons of therapeutic success not only between pharmacological agents but also across a wide spectrum of treatment modalities, encompassing psychosocial and biological approaches, alone and in combination
(16,
17). Recent updates by the Depression and Anxiety Working Group have resulted in expansion of the remission concept to encompass sustained symptom remission during the maintenance phase, in order to support clinical emphasis on extending and maintaining clinical improvement. To this end, specific time frames have been applied to the remission definition during these phases
(18).
The successful implementation of the conceptualization approach to defining change criteria in major depression has led to similar efforts in panic disorder
(18), treatment-resistant depression
(19), generalized anxiety disorder
(20), and eating disorders
(21). In general, these efforts initially emphasized symptomatic improvements, rather than functional improvement, as the primary criteria for defining remission; the evaluation of functional improvement has generally been incorporated into definitions of recovery and “wellness.” In generalized anxiety disorder, for example, response and remission are defined, respectively, as a reduction in and sustained control of symptoms rated with the Hamilton Anxiety Rating Scale. In contrast, the definition of recovery requires sustained symptom remission along with return of function to near-normal levels (with some disease vulnerability); “wellness” is further defined as functional normality in the absence of disease
(20).
In summary, the development and use of remission criteria in mood disorders is instructive for the development of similar criteria as applied to schizophrenia. The applicability to schizophrenia is based on the proven utility of operationalized remission criteria in redefining treatment expectations to “raise the bar” for existing and novel therapies, in enhancing study design and facilitating cross-study comparisons, in providing a single benchmark for longitudinal assessments of disease course, and in recasting concepts of long-term care of patients with mood disorders in terms of a positive, attainable outcome. In considering possible definitions of remission in schizophrenia, important features include applicability to clinical practice across a wide range of treatment settings, utility in research settings, and incorporation of both symptom severity and time components.
Application of the Conceptualization Approach to Schizophrenia
Schizophrenia and other psychotic disorders differ substantially from mood disorders in both disease character and disease course, and any definition of remission in schizophrenia should reflect these characteristic differences. For many years, schizophrenia was regarded as a lifetime chronic illness with little or no hope of recovery. In fact, dramatic improvement in a patient with a diagnosis of schizophrenia was regarded by many clinicians as evidence of original misdiagnosis
(4). The refinement of knowledge regarding the clinical course of schizophrenia, improvements in psychotherapeutic techniques, and the introduction of antipsychotic medications began to alter this view, with consideration of possible parameters to define recovery appearing in the literature as early as 1983
(22).
Psychosocial and vocational therapies have also played a critical role in improving long-term outcome. The effectiveness of family treatment, cognitive behavior therapy, and rehabilitation models has been demonstrated in a range of settings and clinical trial models
(23–
25). In addition, assertive case management has received increased attention as a mechanism to prevent and resolve major social needs and crises
(26). In the United States, however, the availability of such key supports varies substantially between localities, and social and vocational interventions are seldom applied in a manner consistent with optimal clinical outcome
(23,
25,
27).
There also now exists a range of pharmacological and nonpharmacological interventions with proven effectiveness, but with variable effect on specific disease features; pharmacological treatments are also characterized by substantial differences in the nature and severity of adverse effects
(28–
30). This variability highlights the need for and importance of establishing criteria for clinical improvement that can be applied across multiple treatment modalities and specific therapies.
In addition to the development of improved therapeutic options, the disease course of schizophrenia has been more fully characterized in recent years. Although schizophrenia exhibits substantial heterogeneity with respect to severity and course over time, typical features of disease course have been summarized, with support from models presenting schizophrenia as a neurodevelopmental disorder with a substantial hereditary component
(31). From a premorbid stage characterized by nonspecific cognitive, motor, and social impairments, patients move into an extended prodromal stage during which mood, cognitive, psychosocial, and even mild psychotic symptoms of varying severity and duration may appear. The targeting of these early stages for therapeutic intervention, however, has been frustrated by the nonspecificity of the symptoms and their lack of predictive value
(31). Attempts at early treatment have highlighted the substantial duration of time commonly elapsing between symptom onset and diagnosis in first-episode schizophrenia. Although most patients improve significantly after their first episode is treated, the majority experience subsequent episodes, with only a small fraction being able to regain premorbid levels of functionality
(32).
The cycle of relapse, often accompanied by noncompliance with treatment or suboptimal treatment, produces incomplete or unsustained symptom remission in many patients. This condition may subsequently lead to chronic illness characterized by substantial morbidity and persistent deficits in cognition and psychosocial function. Although this progressive “downward spiral” is characteristic for some patients, others may experience a relatively circumscribed deterioration early in the illness, with symptomatic and functional status stabilizing thereafter
(31). Practice guidelines developed by the American Psychiatric Association codified a three-phase model of schizophrenia disease course, with the recognition that these phases “merge into one another without absolute, clear boundaries between them”
(33). In this model, the “acute phase,” characterized by florid psychosis and severe positive and/or negative symptoms, is followed by a “stabilization phase,” during which symptoms recede and decrease in severity, and a subsequent “stable phase” with reduced symptom severity and relative symptom stability. According to these guidelines, “the majority of patients alternate between acute psychotic episodes and stable phases with full or partial remission”
(33), although the operational criteria for remission remain undefined. Also unclear is the extent to which symptomatic remission must occur in order to achieve improved functioning and ultimately recovery and autonomy. Regardless of clinical course, it can be argued that current treatment perspectives are constrained by a view of schizophrenia focused on preventing relapse, in contrast to therapy goals for which long-term symptom remission serves as a foundation for building functional gains.
In light of substantial improvements in understanding schizophrenia and its treatment options, the working group posited that symptomatic remission is a definable concept and an increasingly achievable stage in the treatment of schizophrenia, serving to expand the current ceiling of patient progress beyond “stability.” Further, the importance of defining a remitted state is highlighted by the observation that psychosocial therapies and rehabilitation are most effective when positive and negative symptoms are adequately controlled. The working group concluded that progress toward an operational definition of remission in schizophrenia is warranted at this time because of
•
the emergence of nuanced insights into the etiology, pathophysiology, and disease course in schizophrenia, based on extensive longitudinal research and recent genetic findings;
•
the availability of increasingly effective psychotherapeutic and pharmacological options for treating schizophrenia, including oral and long-acting atypical antipsychotic medications;
•
the need to facilitate standardized comparisons across treatments and therapeutic modalities, especially given the ongoing lack of clinically relevant clarity in comparing different treatments on the basis of clinical trials that use “percent improvement from baseline” as an efficacy measure; and
•
the opportunity that such a definition provides to elevate and more clearly articulate expectations on the part of patients, caregivers, and mental health providers for positive long-term outcome in schizophrenia.
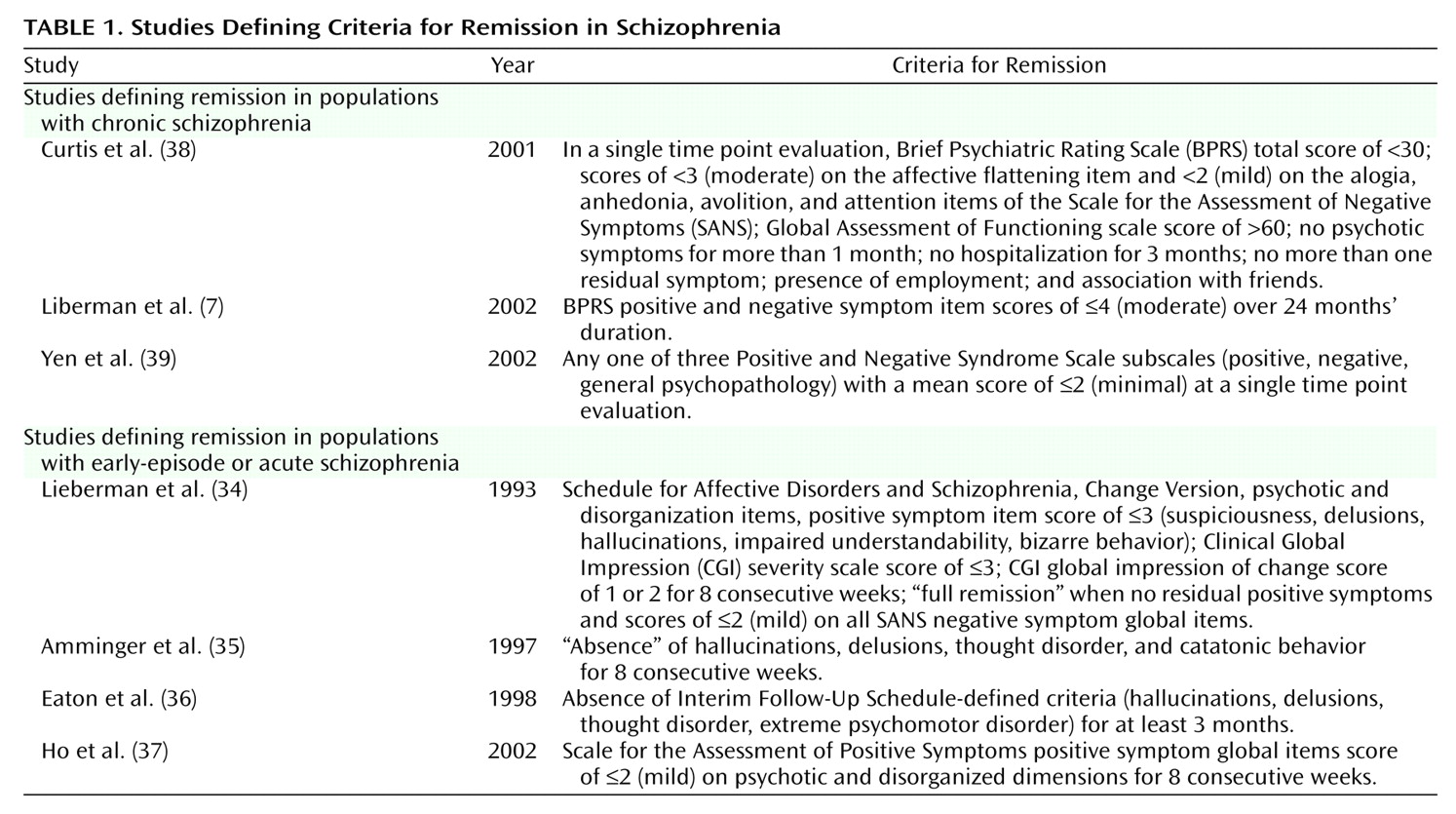
Additional impetus for working toward a consensus definition of remission is provided by prospective and retrospective studies
(7,
34–39), many of which are recent, that define remission and recovery using a range of criteria (
Table 1). Although the symptom-based criteria used in these studies are a marked improvement over the generalized descriptions (such as “mild illness” or “no active psychosis”) that predominated in earlier literature, the lack of consistent definitions prevents cross-study comparison and limits the generalizability of results.
Current Research in Remission and Recovery in Schizophrenia
Recent efforts to describe remission in schizophrenia have been based on longitudinal symptom evaluation combined with a defined time threshold in early-episode or acutely ill populations. However, most of these studies were designed with the goal of identifying prognostic factors for the likelihood of remission, rather than establishment of operational remission criteria
(34–
37). Studies of individuals with chronic schizophrenia have used more variable criteria for remission, including time without hospitalization, decreased delusional thought, and improved insight into illness, with these definitions less often including a time threshold
(7,
38,
39) (
Table 1). However, the widespread use of continuous symptom-based assessment instruments to characterize degree of improvement in patients with schizophrenia suggests that it is an appropriate time to define categories of achieved clinical status based on those instruments.
The working group concluded that any definition of remission in schizophrenia should include a significant time component and be applicable to patients across stages of disease course. This approach suggests that assessment instrument(s) used in the definition of remission should be objective and consistent with regard to test-retest reproducibility. A symptom-based, validated assessment instrument provides the necessary objectivity, consistency, and independence to enable clinicians and researchers to define remission after a first episode and subsequent psychotic episodes and throughout periods of chronic, nonacute illness. In addition, such instruments can be used to evaluate longitudinal status and to support a shifting focus from acute treatment to the continuation and maintenance phases in long-term care.
The working group explicitly considered the incorporation of symptomatic, functional (activities of daily living, social relationships, employment, quality of life), and cognitive outcomes into the definition of remission. The parallel work conducted in mood and anxiety disorders, and the observation that longer-term symptomatic quiescence is a common, but not absolute, prerequisite for functional improvement, suggest that a two-phase model for patient outcomes (remission followed by recovery) may characterize these illnesses well and may potentially be applicable to schizophrenia as well at some time in the future. However, as described earlier, an adequate knowledge base is not yet available concerning the long-term course of cognitive and psychosocial outcomes in schizophrenia and their relationship to changes in symptom patterns and severity. Further, working group consensus recognized that the course of schizophrenia may often be quite complex and present significant challenges to creating a criterion-based definition incorporating function and cognitive components. That is, functional improvement can occur in some patients in parallel with ongoing moderate symptoms, with some individuals developing coping mechanisms that enable them to function despite their illness. The working group therefore concluded that a consensus definition of symptomatic remission, followed by broad dissemination and use in both research and clinical settings, would in turn facilitate the subsequent development of a consensus definition of remission or recovery that includes cognitive and functional outcomes.
Development of Criteria for Remission in Schizophrenia
As a starting point, the working group reviewed the historical constructs for schizophrenia, as well as subsequent studies that used factor analysis to examine the illness construct
(40–
51). For many years categorical approaches were used to identify and classify disease types and subtypes. The traditional categorical “Kraepelinian subtypes” have formed the basis for the DSM approach to classifying schizophrenia in all its recent editions. Although these classifications were retained in DSM-IV, an alternative dimensional approach was also carefully considered and included in the appendix for future consideration.
Categorical and dimensional approaches have important conceptual differences. Although categories divide patients into groups, dimensions divide symptoms into groups. Categorical approaches tend to have the problem that patients’ disorders often do not present in classic “pure” forms. Dimensional approaches recognize the fact that symptom groups overlap in individual patients
(40). The consensus of the working group was that it would be useful to base the definition of symptomatic remission on the more innovative and heuristic dimensional approach to descriptive psychopathology.
Dimensions of psychopathology are typically identified by using the statistical techniques of factor analysis. Numerous factor analytic studies have been conducted, with highly replicable results
(41–
47). Three dimensions have been identified. The first, a negative symptom dimension (also referred to as psychomotor poverty), includes poverty of speech, decreased spontaneous movement, unchanging facial expression, paucity of expressive gesture, affective nonresponse, and lack of vocal inflection. The second, a disorganization dimension, includes symptoms of inappropriate affect, poverty of content of speech, tangentiality, derailment, pressure of speech, and distractibility. The third, a psychoticism dimension (also called “reality distortion”), includes hallucinations and delusional ideas. These results confirm the importance of negative symptoms and suggest that “positive symptoms” should be further subdivided into a psychotic and a disorganization dimension.
However, factor analysis demonstrates only that symptoms are correlated with one another in the specific groups of patients studied. The dimensions identified by factor analysis can be considered to be valid only if they have meaningful relationships with other clinical or biological measures. The validity of these dimensions has been supported by studies demonstrating relationships with neuropsychological measures, longitudinal course, and neuroimaging measures
(41,
42,
48–52). It has been posited that although medication may have differential effects on these three dimensions, they represent related but distinguishable components of the disease process in schizophrenia.
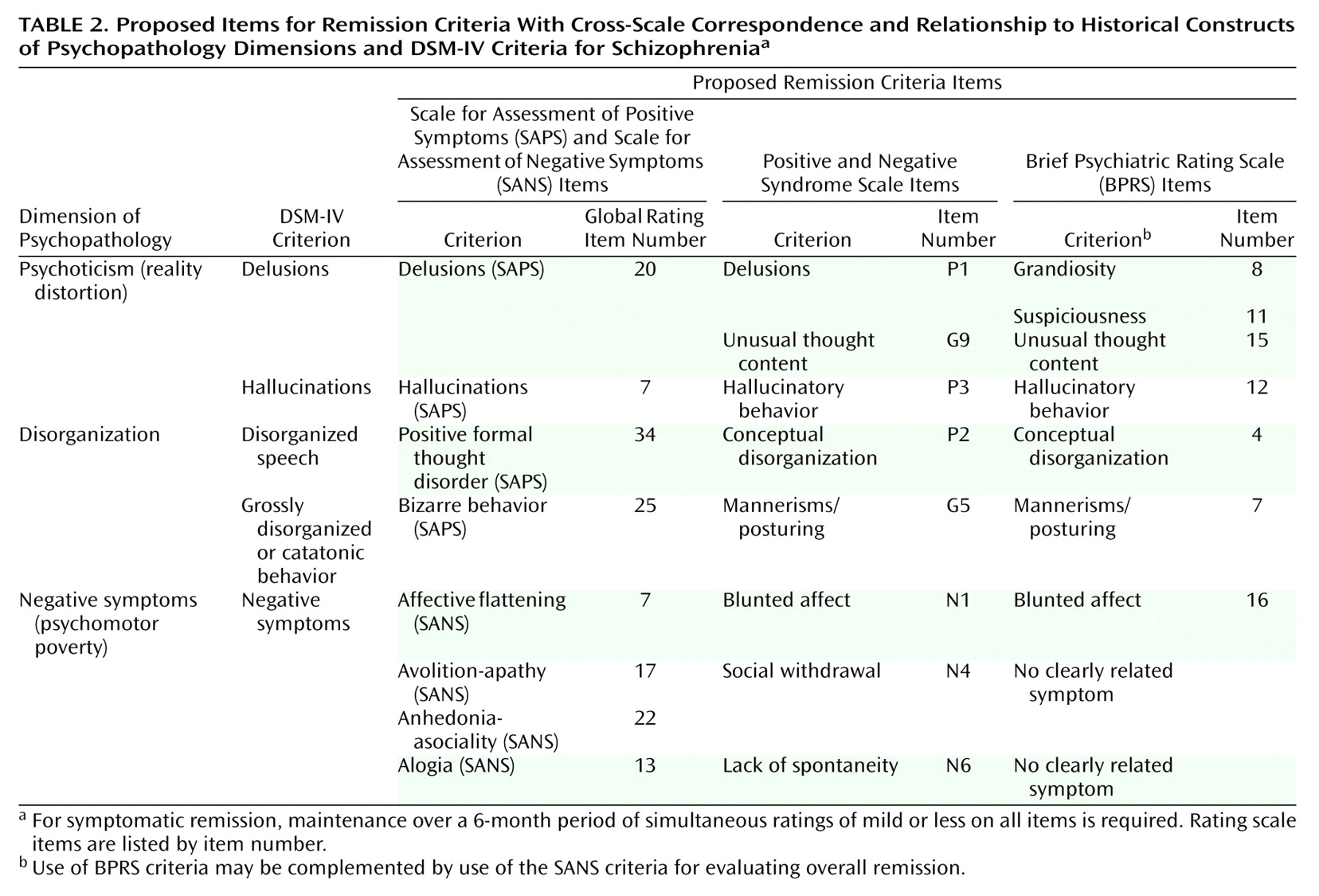
The DSM-IV diagnostic criteria for schizophrenia closely align with the three dimensions identified in the factor analyses reviewed here, representing the application of such concepts to clinical practice. Agreeing on the value of this widely accepted application, the working group then considered assessment instrument(s) on which an operational definition of symptom remission could be practically based. Subsequently, three validated, widely used assessment scales were identified: 1) a single scale represented by the Scale for the Assessment of Positive Symptoms (SAPS) and the Scale for the Assessment of Negative Symptoms (SANS)
(52,
53), 2) the Positive and Negative Syndrome Scale
(54), and 3) the Brief Psychiatric Rating Scale (BPRS)
(55).
The SAPS, a 34-item scale used to assess positive symptoms in schizophrenia, is designed for use in conjunction with the 25-item SANS, which is used to assess negative symptoms; scoring ranges from 0 (no abnormality) to 5 (severe). Ratings from the SAPS and SANS
(52,
53) are divided into three symptom dimensions, including psychoticism (hallucinations and delusions), negative symptoms (affective flattening, alogia, avolition-apathy, and anhedonia-asociality), and disorganization (inappropriate affect, bizarre behavior, and formal thought disorder)
(45). The Positive and Negative Syndrome Scale
(54) is a 30-item inventory assessing the absence or severity of schizophrenia symptoms across three subscales: positive symptoms (items P1–P7, including hallucinatory behavior, delusions, and conceptual disorganization), negative symptoms (items N1–N7, including blunted affect, social and emotional withdrawal, and lack of spontaneity), and general psychopathology symptoms (items G1–G16, including mannerisms and posturing, unusual thought content, and lack of insight). Each item is scored on a scale ranging from 1 (absent) to 7 (extreme), with item ratings incorporating the behavioral effect of symptoms as well as their severity. The BPRS
(55) is an 18-item scale originally formulated by using a 7-point range from 1 (not present) to 7 (most severe), although a 6-point version (0, not present, to 6, most severe) also exists. Ratings are based on clinical observations of symptoms (tension, emotional withdrawal, mannerisms and posturing, motor retardation, and uncooperativeness) and subjects’ verbal report of symptoms (conceptual disorganization, unusual though content, anxiety, guilt feelings, grandiosity, depressive mood, hostility, somatic concern, hallucinatory behavior, suspiciousness, and blunted affect)
(56).
Based on an examination of these scales, the working group identified appropriate criteria to serve as the basis for defining symptomatic remission in schizophrenia. The goal was to align significant research on symptom factors in schizophrenia and their practically applied outcome (DSM-IV criteria) with major symptom domains that significantly affect the course of illness. Although the working group recognized that a variety of symptom domains (e.g., depression, anxiety) also affect patient outcome and well-being, consensus was reached to maintain a focused, diagnostic-based definition. In addition, the working group proposed that remission criteria might be described separately for positive and negative symptoms, to allow primary consideration of these symptom groups independently in the assessment of symptomatic remission. It should be noted that a potential complication in the assessment of negative symptoms is the possibility that symptoms in certain domains, such as anhedonia, may be secondary (as a side effect of neuroleptic treatment or a symptom of comorbid depression) rather than primary. Likewise, positive symptoms may sometimes be secondary (e.g., agitated disorganized behavior secondary to akathisia).
Specific items selected for consideration as criteria for remission in schizophrenia were chosen to map the three dimensions of psychopathology identified by factor analyses and the five criteria for schizophrenia specified in DSM-IV (see
Table 2 for details). With regard to severity, the working group consensus defined a score of mild or less (Positive and Negative Syndrome Scale item scores of ≤3; BPRS item scores of ≤3, using the 1–7 range for each item; SAPS and SANS item scores of ≤2) simultaneously on all items as representative of an impairment level consistent with symptomatic remission of illness. Given the long-term course and intrinsic character of schizophrenia, the working group consensus defined a period of 6 months as a minimum time threshold during which the aforementioned symptom severity must be maintained to achieve remission. When the BPRS is used in assessment, the possibility of including the SANS should be considered, to provide complementary information on negative symptom items in achieving the criteria for overall (positive and negative) symptomatic remission.
In consideration of clinical realities and research interests, the working group consensus provided that in addition to meeting the criteria, individuals may remain in remission while experiencing minor changes in symptoms, in the absence of appreciable effects on daily function or subjective well-being. Ongoing or emerging thoughts regarding self-harm or harm of others were considered to be a critical focus for clinical care; the relationship of these thoughts to remission may depend on their presence as part of a depressive versus psychotic disorder.
Implementation of these criteria should provide researchers and clinicians with a robust, well-defined outcome goal in the long-term treatment of schizophrenia, facilitating comparisons of effectiveness across therapeutic modalities. Moreover, the use of these criteria may more closely align the interests and goals of clinicians, professional organizations, commercial entities, and regulatory agencies with those of patients, their families, and caregivers. To facilitate the adoption and implementation of these criteria, the working group proposed parallel, cross-scale remission criteria items (
Table 2). As part of the evaluation of the proposed remission criteria, and to expand knowledge about the relationship of remission to recovery of functioning, both academic and commercial interests should include metrics of patient functioning in future clinical investigations. The implementation of criteria for symptomatic remission will support efforts around the development of criteria for recovery from schizophrenia, which is conceptually related to and facilitated by symptom stabilization and remission.
Conclusions
The Remission in Schizophrenia Working Group was formed to develop criteria for symptomatic remission in patients with schizophrenia, in a manner similar to consensus development in mood and anxiety disorders. The timeliness of these criteria is reinforced by the growing understanding of disease course, by evolving treatment options, and by the constrained outcome expectations held by affected individuals, care providers, and clinicians. These criteria are proposed with the goals of further examining their validity and utility and of providing momentum and support for definitions of recovery or for other types of definitions that would include functional criteria. The ability to incorporate the growing amount of information related to cognitive dysfunction remains present, pending the evolving consensus around core deficits associated with schizophrenia. Acceptance, refinement, and use of these criteria should help to facilitate comparisons of effectiveness across the range of available therapeutic options and to support a positive, longer-term approach regarding outcome for patients with schizophrenia.