Mentioned briefly in DSM as “a diminished ability to think or concentrate” (DSM-IV), the effects of depression on cognitive functioning are more wide-ranging and pronounced than this statement indicates. Deficits in verbal fluency
(4,
5), visual search
(6), psychomotor speed
(7), attention
(8), and working memory
(9,
10) have been reported. Automatic processing abilities remain largely intact
(6) .
Few studies have examined the cognitive impairment in seasonal affective disorder, initially finding associated deficits for individuals with seasonal affective disorder on tasks requiring an extended period of mental effort, perceptual flexibility, and abstract thinking
(1) . O’Brien et al.
(11) also administered a wide array of assessments for cognitive ability (i.e., spatial recognition, short-term memory, learning, and psychomotor speed) to 11 patients with seasonal affective disorder and 10 comparison subjects who were matched for age, IQ, and education. The tests were administered once in the winter and again in the summer after remission of symptoms and clinical recovery. Impairments in pattern recognition, visual short-term memory, and visual learning that were observed in the winter (in relation to comparison subjects) improved after clinical recovery in the summer. A study by Michalon et al.
(12) administered visual and verbal assessments to 30 patients with seasonal affective disorder and 29 age- and education-matched comparison subjects before and after 2 weeks of light treatment. The most consistent deficits associated with seasonal affective disorder were on tests of visual memory and visual construction skills, both of which improved after light therapy.
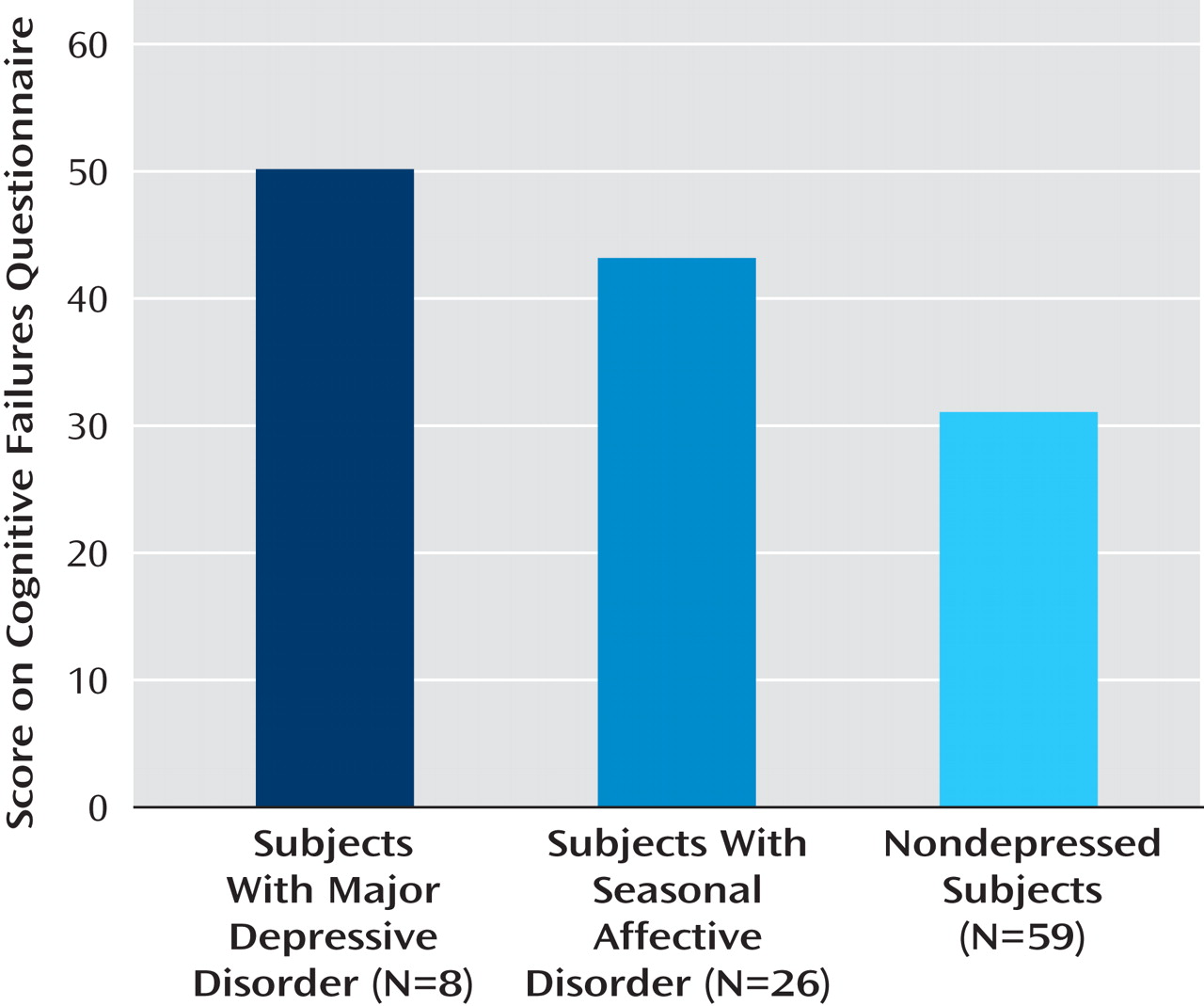
Given the scarcity of research on seasonal affective disorder and cognitive deficits, the goal of the current study was to better understand the similarities between seasonal and nonseasonal depression in cognitive function. Instead of assessing highly specific cognitive processes, we chose to examine a broader category of functions that appear to be evident to the individual in real-world activities.
Cognitive failures are the reported difficulties people experience in typical everyday situations (e.g., forgetting names or misinterpreting directions) that are linked to lapses in controlled processes, such as focus of attention and working memory
(13) . Assessing cognitive failures includes asking individuals to rate how often certain mistakes occur, such as forgetting what you went to the store to buy, failing to notice signs, or missing appointments
(14) . Although cognitive failures are not considered to be particularly dangerous in and of themselves, they are strongly related to more serious occurrences, such as car accidents, hospitalizations, and falling injuries
(15) and work-related accidents
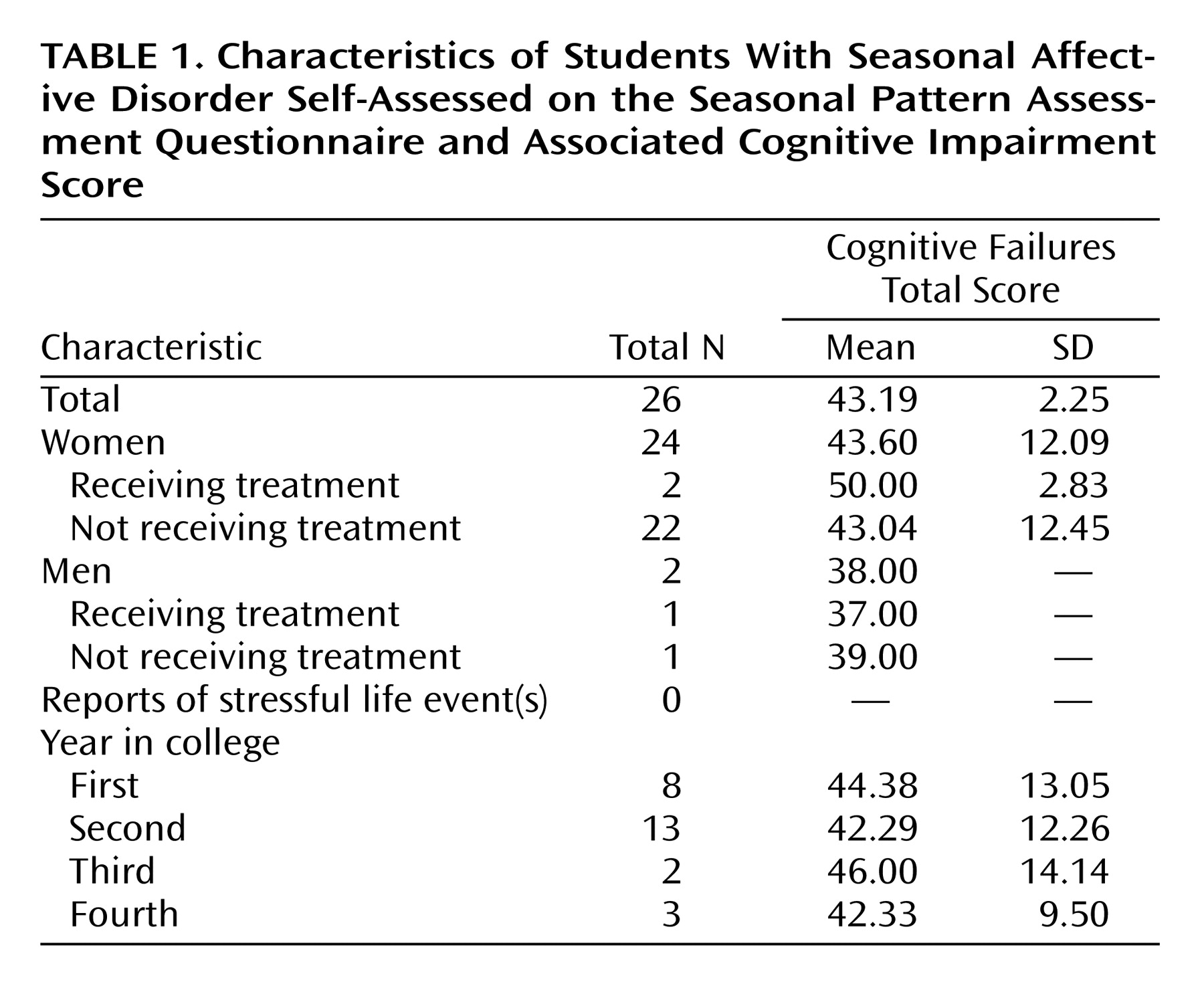
(16) . The present study identified individuals who have seasonal affective disorder or who have major depressive disorder by observing self-reported responses on affective inventories (the Beck Depression Inventory and the Seasonal Pattern Assessment Questionnaire). We expected that in the Midwestern region of the United States there would be college students qualifying for seasonal and nonseasonal depression during the month of November, allowing a comparison of cognitive failures across the two types of depression, along with a nondepressed group.