The treatment of patients with borderline personality disorder is challenging
(1,
2) . The use of medication has increased, but while several drugs have proven useful, their benefit has been modest
(3 –
4) . A range of psychotherapies has been developed and several have garnered empirical support
(5 –
12), including dialectical behavioral therapy
(5 –
7,
12), mentalization-based therapy
(8,
9), cognitive behavioral therapy
(10), schema-focused therapy
(11), and transference-focused therapy
(12) .
In 1995, Blum et al. developed Systems Training for Emotional Predictability and Problem Solving (STEPPS) based on a program introduced by Bartels and Crotty
(13) . STEPPS is a group treatment that combines cognitive behavior elements and skills training with a systems component for individuals with whom a patient regularly interacts
(14,
15) . STEPPS is easily learned and efficiently delivered by therapists of varying educational and professional backgrounds. The program supplements—but does not replace—a patient’s ongoing treatment (e.g., medication, individual therapy, case management). Data from two uncontrolled studies have supported its use
(16,
17) . STEPPS is used in the United States
(18) and was introduced in the Netherlands in 1998. By 2005, nearly 400 Dutch therapists were trained in its use
(18) .
In the present study, we report results of a 20-week randomized controlled trial and a 1-year follow-up. Outpatients with borderline personality disorder were randomly assigned to STEPPS plus treatment as usual or treatment as usual alone. We hypothesized the following: 1) STEPPS plus treatment as usual would result in greater improvement in borderline traits, social functioning, global functioning, and mood relative to treatment as usual alone; 2) STEPPS plus treatment as usual would result in fewer suicidal and self-harm acts and the use of fewer crisis resources relative to treatment as usual alone; and 3) gains resulting from STEPPS plus treatment as usual would be maintained during the follow-up.
Method
Subjects
Subjects with DSM-IV
(19) borderline personality disorder were recruited from the University of Iowa inpatient and outpatient psychiatric services (N=92); clinicians and mental health centers in eastern Iowa (N=35); advertisements (N=29); word of mouth (N=8); and unspecified methods (N=8). We excluded subjects who 1) did not speak English; 2) had a psychotic or primary neurological disorder; 3) were cognitively impaired; 4) had current (past month) substance abuse or dependence; or 5) participated in STEPPS previously. Subjects were required to designate a mental health professional and a friend or relative to serve as system members. The purpose was to ensure that an independent mental health professional could be reached in a crisis and that a friend or relative could participate in the systems component of STEPPS. The designated individual was taught how to respond to the subject’s dysfunctional thoughts or behaviors. Subjects were not required to have recent suicidal or self-harm behavior. Subjects gave written informed consent according to procedures approved by the University of Iowa Institutional Review Board.
Assessments
The diagnosis of borderline personality disorder was established using the Structured Interview for DSM-IV Personality
(20) . The Structured Clinical Interview for DSM-IV (SCID)
(21) assessed current and lifetime DSM-IV axis I disorders. Efficacy assessments included the Zanarini Rating Scale for Borderline Personality Disorder
(22) to assess affective disturbance, cognitive disturbance, impulsivity, and disturbed relationships; the Borderline Evaluation of Severity Over Time
(18) to assess thoughts, feelings, and behaviors associated with borderline personality disorder; the Positive and Negative Affect Schedule (PANAS)
(23) to assess positive and negative dispositions; the Beck Depression Inventory
(24) ; the Symptom Checklist-90-Revised
(25) ; the Barratt Impulsiveness Scale (version 11a)
(26) ; and the Social Adjustment Scale
(27) . Suicide and self-harm behaviors, medication usage, physician visits, other therapies, and crisis contacts were also assessed.
Primary outcome was the Zanarini Rating Scale for Borderline Personality Disorder total score. Zanarini Rating Scale for Borderline Personality Disorder subscales were used as secondary efficacy measures. Other secondary measures included the rater-administered Clinical Global Impression (CGI) Improvement and Severity scales
(28), patient CGI self-rating
(28), Global Assessment Scale
(29), Beck Depression Inventory
(24), Symptom Checklist-90-Revised
(25), Barratt Impulsiveness Scale
(26), and Social Adjustment Scale
(27) . The CGI and Global Assessment Scales were used in part because of their demonstrated utility in medication studies of borderline personality disorder
(30,
31) . Secondary outcome measures also included crisis variables (hospitalizations, emergency department visits, and crisis phone calls), suicide attempts, and self-harm acts.
To achieve reliability on interview measures, raters were trained by Nancee Blum, who also provided ongoing supervision. Excellent diagnostic agreement was achieved (kappa=1.0 for borderline personality disorder). The intraclass correlation coefficient was 0.96 for the Zanarini Rating Scale for Borderline Personality Disorder total and 0.58 for the CGI severity ratings.
In addition to screening and baseline evaluations, subjects were assessed at weeks 4, 8, 12, 16, and 20. The Client Satisfaction Questionnaire-8
(32) was administered at week 20.
Treatment Assignment
Subjects were assigned by coin toss to either the STEPPS plus treatment as usual group or treatment as usual alone group. Whenever eight to 12 subjects were assigned to STEPPS plus treatment as usual, they were notified that a group would begin. Groups began a mean of 6.5 (SD=6.6) weeks after random assignment. Eight treatment cohorts were recruited between 2002 and 2006.
STEPPS Program
STEPPS is a manual-based group treatment program for outpatients with borderline personality disorder that combines cognitive behavioral elements with skills training; it does not include individual therapy. The program involves 20 2-hour weekly sessions with two co-facilitators who follow a detailed lesson plan. Participants receive a packet of materials each week, including an agenda and homework assignments. STEPPS is systems-based in that family members, significant others, and health care professionals are educated about borderline personality disorder and instructed how best to interact with their relative or friend with the disorder. Participants are urged to share their notebooks and lesson materials with system members.
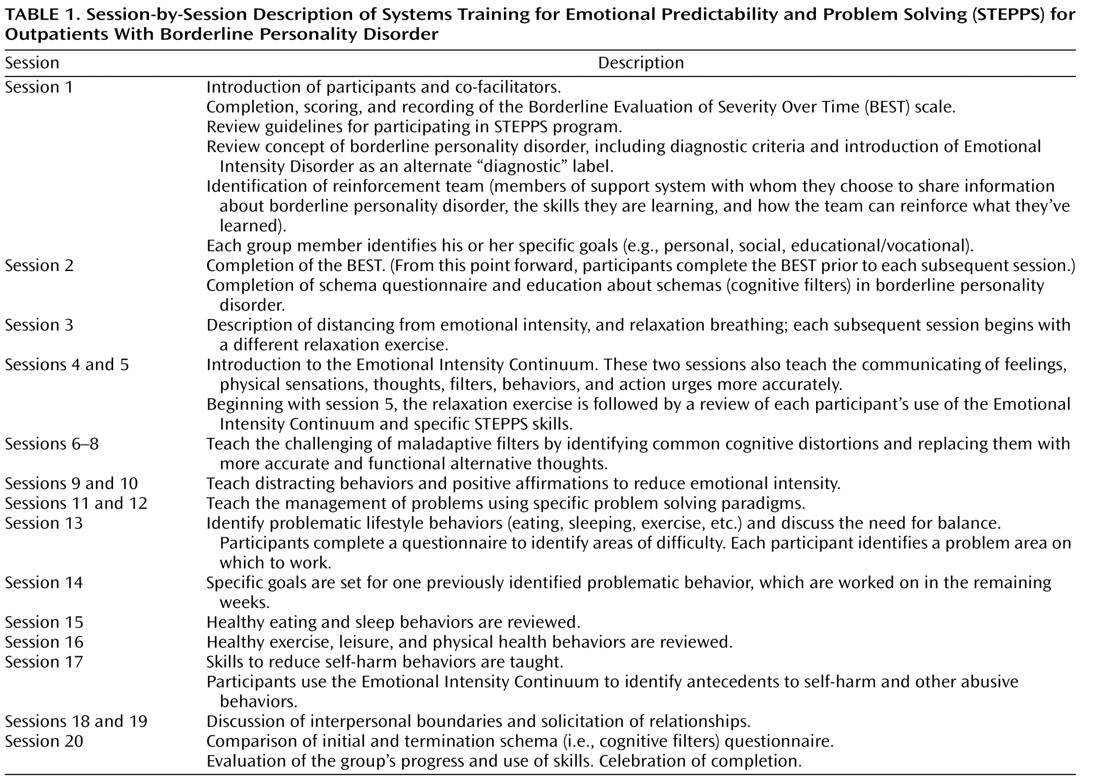
The STEPPS program has the following three main components: 1) psychoeducation about borderline personality disorder; 2) emotion management skills training; and 3) behavior management skills training. The first component teaches subjects to replace misconceptions about borderline personality disorder with an awareness of the thoughts, feelings, and behaviors that define it and to identify their own schemas (i.e., cognitive filters) that drive their behaviors. The disorder is also reframed as an emotional intensity disorder, which patients find preferable to borderline personality disorder. The second component teaches the following skills to better manage the cognitive and emotional effects of borderline personality disorder: distancing, communicating, challenging, distracting, and problem management. The third component teaches the following behavioral skills, which subjects are encouraged to master: goal setting, healthy eating behaviors, sleep hygiene, regular exercise, leisure activities, health monitoring (e.g., medication adherence), avoiding self-harm, and interpersonal effectiveness. A session-by-session description is provided in
Table 1 .
Sessions have the look and feel of a seminar. Participants sit at a conference table facing a board. There is a short break between the first and second hours. Each weekly session is organized around a particular skill. Some skills require more than one session to teach. In addition to the use of a board and printed materials, the program is facilitated by poetry, songs, art work, and relaxation exercises. Participants are encouraged to bring materials or artwork to reinforce the skills and themes of the meetings.
Participants are asked to monitor their thoughts, feelings, and behaviors over the course of the program; this enables them to become aware of and to monitor improvements in the intensity and frequency of their emotional episodes. They are introduced to the Emotional Intensity Continuum, a 1- to 5-point scale using the metaphor of pots on a burner. At level 1, there is no heat under the pot; at level 5 the pot is boiling over. This allows participants to recognize early warning signs of an impending outburst. New skills become the tools to prevent the heat from getting too hot, thereby reducing the chance that the pot will boil over. With this and other metaphors, abstract concepts are made more concrete and understandable. As participants progress, they are asked to monitor the new skills employed to manage their emotional intensity. Patients gradually become more aware of emotional triggers that may lead to outbursts.
Participants are encouraged to continue with ongoing concomitant treatment. Those participating in individual therapy are asked to familiarize their therapist with STEPPS, thereby enabling all members of the treatment team to employ a consistent approach and terminology. Participants are encouraged to show a copy of the handouts to their therapist and to review their homework assignments during their individual sessions.
A 2-hour evening session is held for family members or significant others as part of the program. These individuals are educated about borderline personality disorder and how best to respond to their relative or friend with the disorder. STEPPS attendees are encouraged to share their lessons with their individual therapist and significant others. This constitutes the systems component of the program.
STEPPS was administered by two of the authors of the present study (Ms. Blum and Mr. St. John). Adherence to the manual was rated on a 5-point scale, with a score of 5 denoting excellent adherence (unpublished data of Donald W. Black, 2002). A score of 4 (good) or higher was considered acceptable. Two Ph.D.-level psychologists who were not involved with the randomized controlled trial but familiar with STEPPS rated 43 randomly selected videotaped sessions. The mean adherence score was 4.4 (SD=0.8).
Additional information about the STEPPS program may be found at www.steppsforbpd.com. The website contains a summary of the program, literature references, author information, and contact instructions.
Treatment as Usual
Subjects assigned to either STEPPS plus treatment as usual or to treatment as usual alone were encouraged to continue their usual care, including individual psychotherapy, medication, and case management. Subjects received no instructions or advice about other pharmacologic or psychotherapeutic treatments. Subjects assigned to treatment as usual alone could not attend any STEPPS group until they completed the 20-week trial.
Follow-Up
At the end of the 20-week treatment period, subjects entered a 1-year follow up. Assessments were made at months 1, 3, 6, 9, and 12. These included the Borderline Evaluation of Severity Over Time, Beck Depression Inventory, PANAS, CGI severity and improvement ratings, Global Assessment Scale, and Social Adjustment Scale. Data on crisis variables, medication use, psychotherapy visits, suicide attempts, and self-harm acts were also collected.
Statistical Analysis
Subjects with at least one postbaseline assessment were included in the analyses. To test for treatment group imbalances, baseline demographic characteristics and clinical variables were compared using Pearson’s chi-square tests or Student’s t tests.
A linear mixed-effects model was used for primary and secondary outcomes. Each subject’s trajectory of scores from baseline to week 20 was summarized with a subject-specific intercept and slope, thus allowing STEPPS efficacy to be tested by examining the difference between the mean slopes of the two groups. To adjust for possible bias from informative right censoring (which occurs, for example, when subjects with more favorable response are more likely to be assessed), last assessment time was used as a covariate for intercepts and slopes. For the primary outcome variable (Zanarini Rating Scale for Borderline Personality Disorder total), last assessment time was not related to baseline score (intercept) or level of improvement (slope), and therefore this adjustment had little effect on the test of STEPPS efficacy. To ensure that a significant baseline difference with respect to avoidant personality disorder did not confound the test of STEPPS efficacy, the disorder was used as a covariate for intercepts and slopes. Avoidant personality disorder was associated with baseline severity (intercept) for the primary outcome but not level of improvement (slope), an adjustment that had little effect on the test of STEPPS efficacy.
Group differences were also tested across the 1-year follow-up. A repeated measures analysis of variance (ANOVA) model was used to compare group changes from week 20 with week 72 (1-year follow-up). By utilizing the correlation of subjects’ responses over time, this model accommodates subjects with incomplete data. The correlation of subjects’ responses was assumed to have a first-order autoregressive structure, which assumes that the correlation of a subject’s responses decreases as the time between the assessments increases. For this analysis, week 20 was considered the baseline.
Groups were compared on the use of crisis services throughout the treatment and follow-up periods. For these variables, subjects were asked to report utilization during the last month. For each subject, we counted the number of follow-up months (n) and number of months for which each crisis service (hospitalizations, emergency department visits, and crisis calls) was utilized (y). Assuming a binomial model (y is a binomial random variable with parameters n and p) with logistic link function, we tested whether the probability of monthly utilization (p) differed for the groups. Using the Cox proportional hazards model, the study groups were compared on times to first suicide attempt and self-harm act.
Statistical analyses were carried out using SAS
(33) . The linear mixed-effects and repeated measure models were fit using the MIXED procedure; the binomial models were fit using the NLMIXED procedure; and the Cox proportional hazards model was fit using the PHREG procedure. All tests were performed using a two-sided significance level of p=0.05.
Results
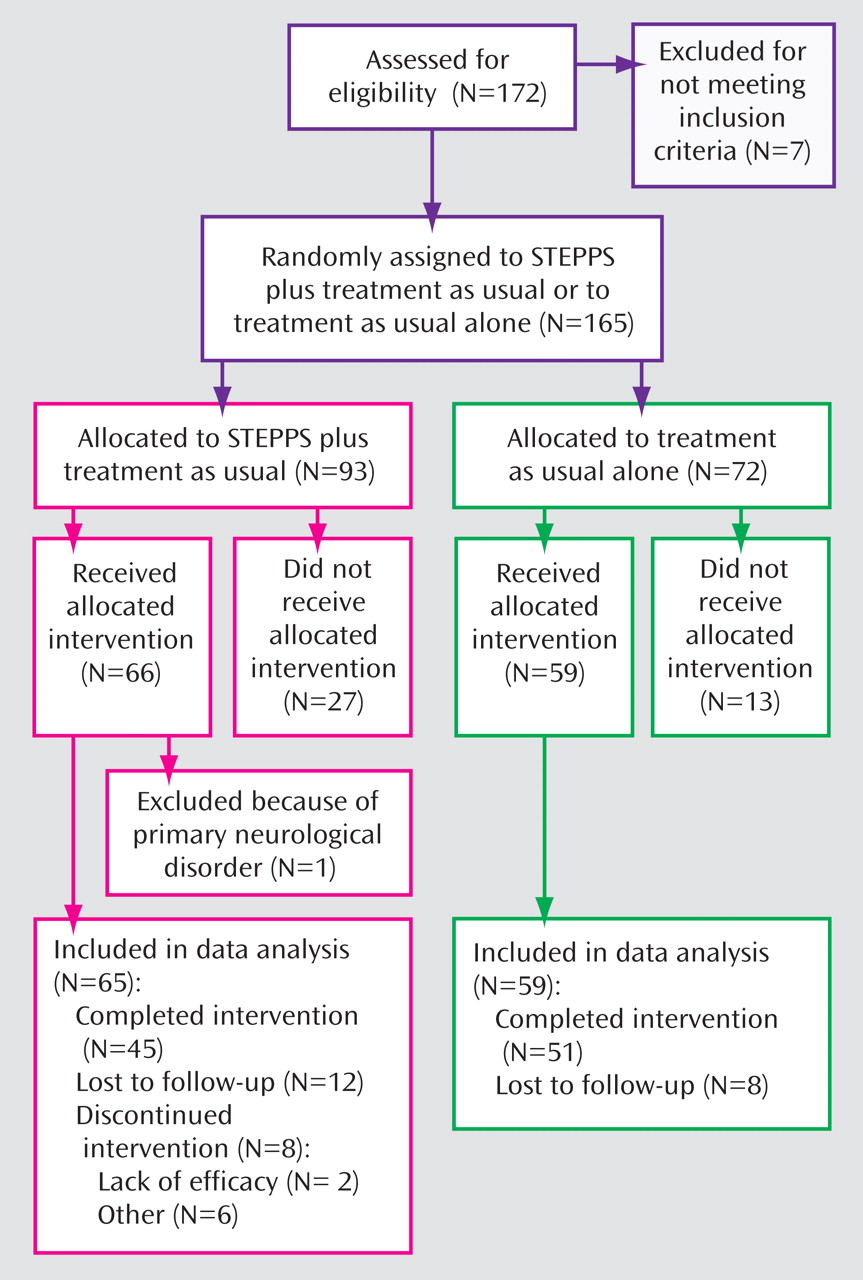
One hundred seventy-two men and women 18 years and older were screened; 165 were enrolled and randomly assigned to STEPPS plus treatment as usual or treatment as usual alone. One hundred twenty-five subjects received the allocated interventions. Of these, data from 124 were analyzed (
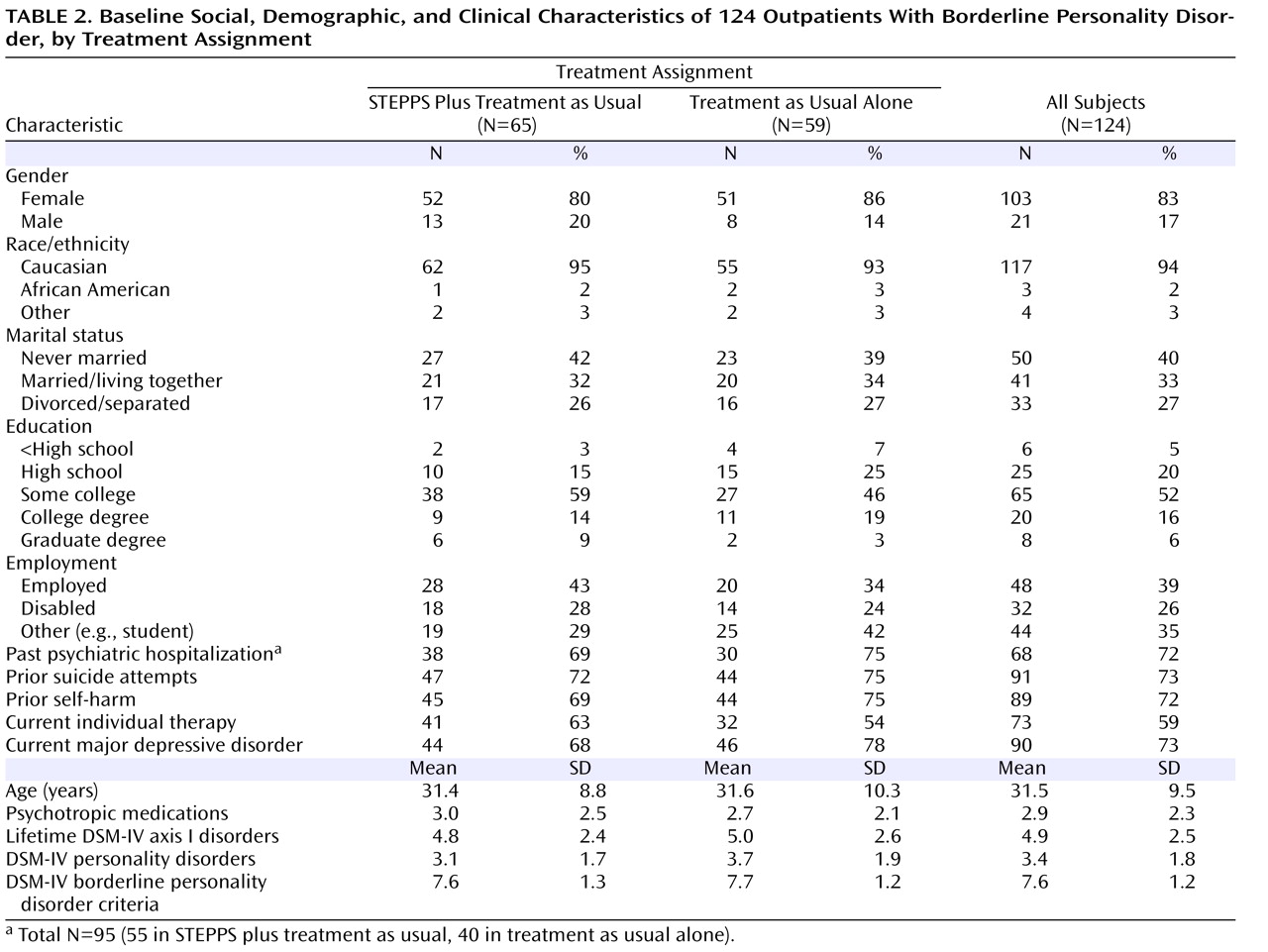
Figure 1 ). (One subject was excluded because of a primary neurological disorder.) The groups were balanced on baseline demographic and clinical variables (
Table 2 ), except avoidant personality disorder was more frequent in the treatment as usual alone group (66% versus 45%; χ
2 =5.8, df=1, p=0.016).
Forty-five (69%) subjects assigned to STEPPS plus treatment as usual and 51 (86%) subjects assigned to treatment as usual alone completed the week 20 assessment (χ 2 =5.2, df=1, p=0.022). Baseline variables—age, gender, severity (Borderline Evaluation of Severity Over Time), and depression (Beck Depression Inventory)—were not predictive of having at least one postbaseline assessment or early discontinuation. Subjects completed a mean of 4.2 (SD=1.3) assessments, with no significant differences between treatment conditions (Mann-Whitney test: χ 2 =1.6, df=1, p=0.213). Overall, 82 (66%) subjects were assessed at least once during the 1-year follow-up. During follow-up, the mean number of assessments was 3.0 (SD=1.6) for STEPPS plus treatment as usual recipients and 2.8 (SD=1.3) for treatment as usual alone recipients (Mann-Whitney test: χ 2 =0.4, df=1, p=0.549). STEPPS recipients attended a mean of 12.9 (SD=5.4) group treatment sessions.
Assessment of Efficacy: Treatment Period
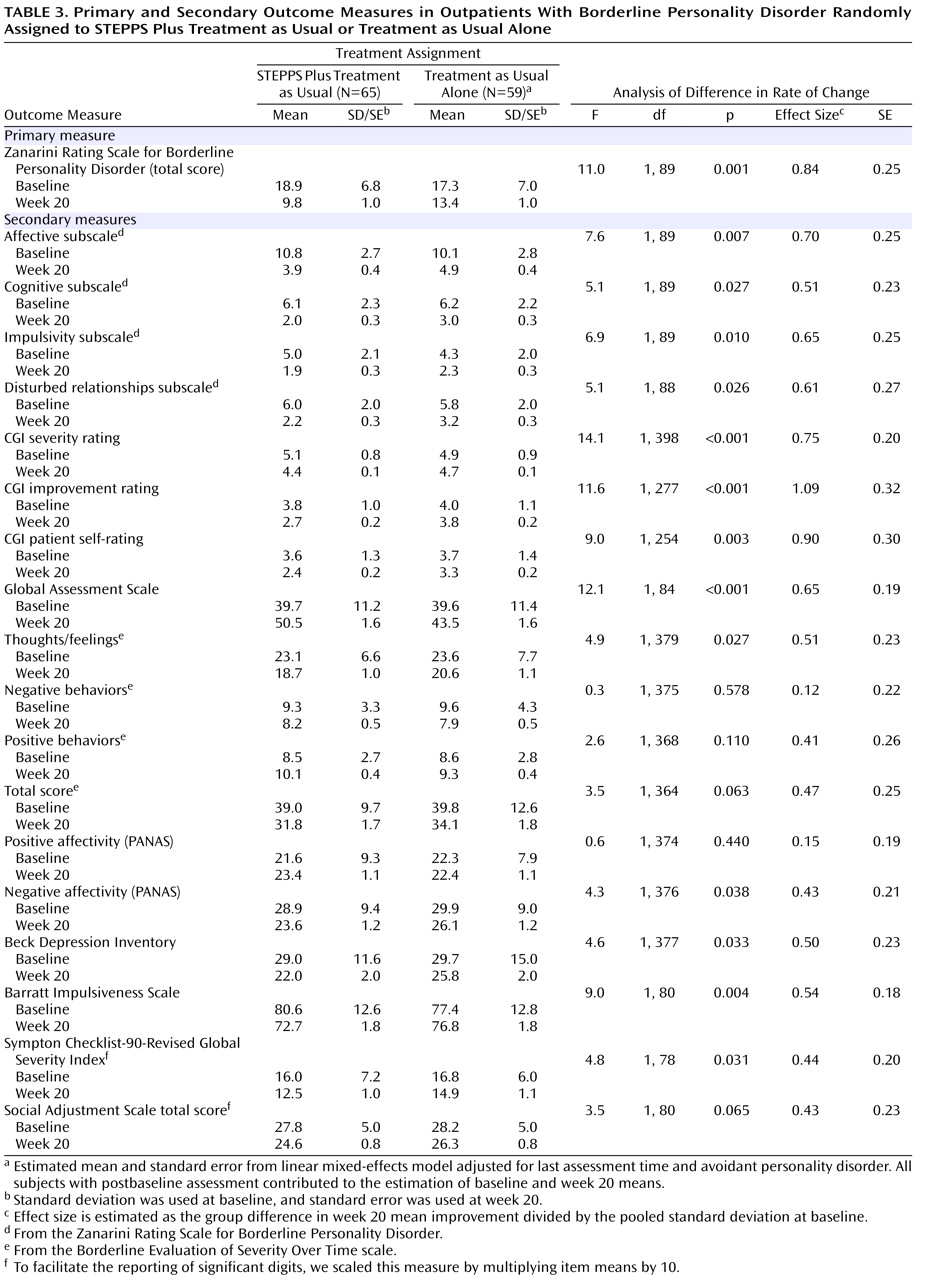
STEPPS plus treatment as usual recipients improved from baseline through week 20 on primary and secondary outcome measures (
Table 3 ). The mean rate of change for the STEPPS plus treatment as usual group was significantly greater relative to the treatment as usual alone group for the Zanarini Rating Scale for Borderline Personality Disorder total and all four subscales, CGI severity and improvement ratings, Global Assessment Scale, Borderline Evaluation of Severity Over Time (thoughts/feelings subscale), Barratt Impulsiveness Scale, PANAS (negative affectivity subscale), Beck Depression Inventory, Symptom Checklist-90-Revised (depression, psychoticism, and global severity subscales), and Social Adjustment Scale (social/leisure subscale and total score). For other outcomes, improvement observed in the STEPPS plus treatment as usual group was greater than the treatment as usual alone group, but differences were not statistically significant.
Effect sizes for the STEPPS program at 20 weeks represent group differences in mean improvement divided by the pooled standard deviations at baseline. While some assessment scales were reverse-coded (lower scores more favorable), we report all effect sizes in a positive direction. For the Zanarini Rating Scale for Borderline Personality Disorder total, estimated effect size was 0.84, indicating a large effect of the STEPPS program on the primary outcome. For secondary outcome measures, effect size estimates ranged from 0.12–1.09. Generally, those of 0.50 and greater were statistically significant.
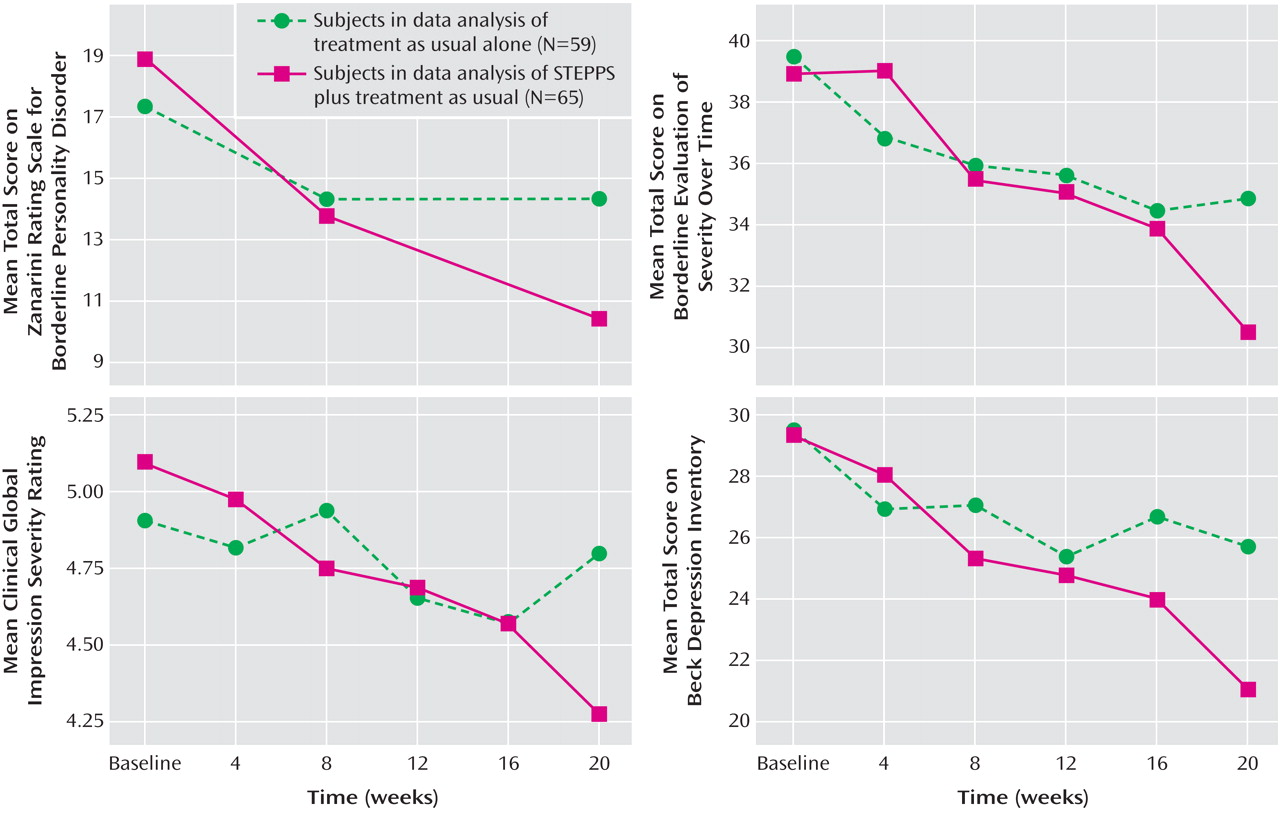
Figure 2 shows estimated means over the treatment period for the primary and selected secondary outcomes. Improvements for the STEPPS plus treatment as usual group appear to be monotonic and roughly linear. Improvements for the treatment as usual alone group appear mostly confined to the first half of the treatment period.
Subjects randomly assigned to STEPPS plus treatment as usual had greater change in CGI severity and improvement ratings relative to those randomly assigned to treatment as usual alone. Using each subject’s last observation within the treatment period, those randomly assigned to STEPPS plus treatment as usual were more likely to be rated “very much” or “much” improved (40.0% versus 5.1%; χ 2 =21.0, df=1, p<0.001); subjects’ own global self-ratings showed similar results, with 58.5% of STEPPS plus treatment as usual recipients rating themselves as “very much” or “much” improved, compared with 22.0% for those assigned to treatment as usual alone (χ 2 =16.9, df=1, p<0.001). STEPPS plus treatment as usual recipients were more likely to reach the clinically relevant Global Assessment Scale cutoff (>60) (18.5% versus 5.1%; χ 2 =5.2, df=1, p=0.023).
Assessment of Efficacy: 1-Year Follow-Up
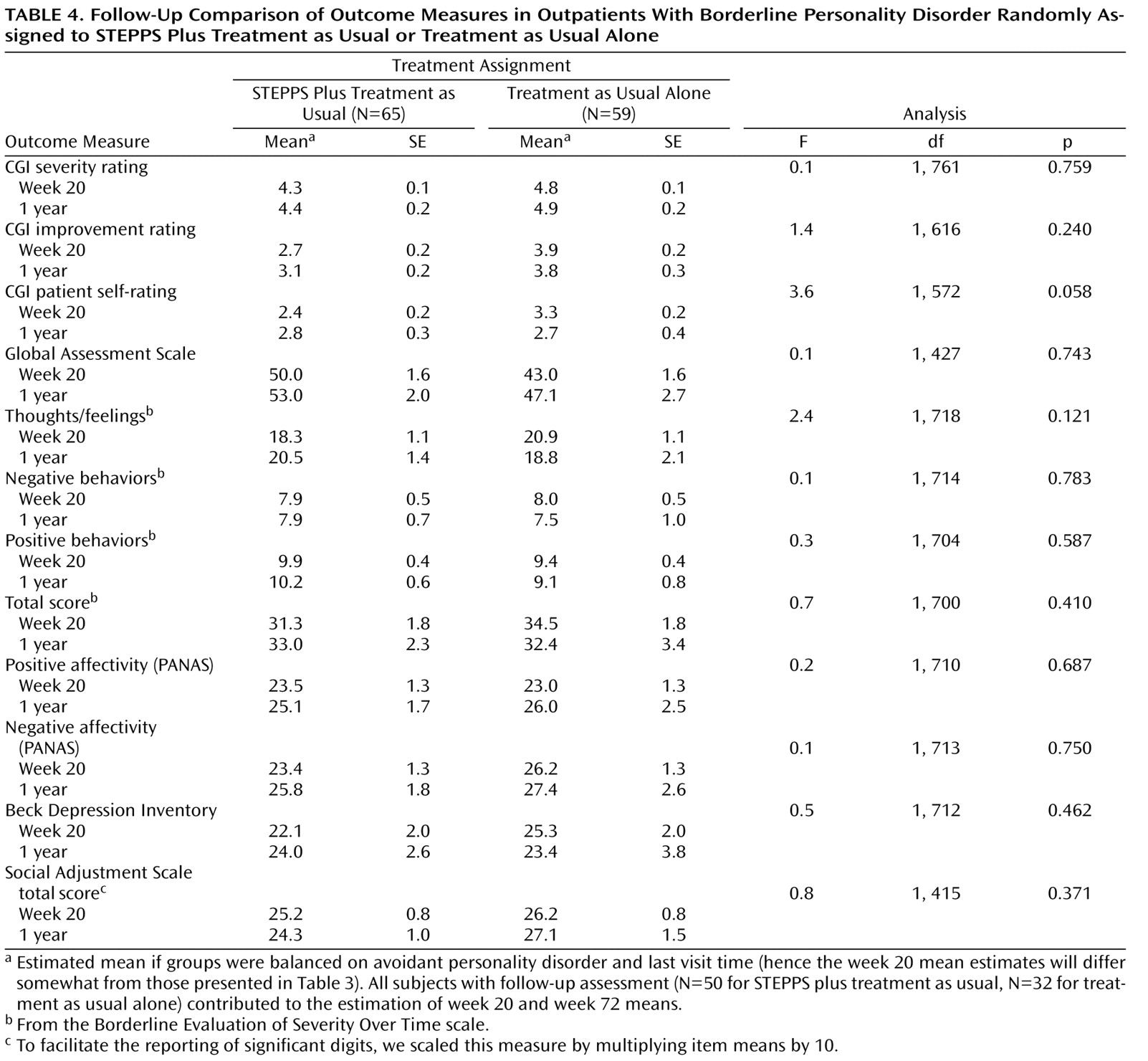
There were no statistically significant group differences across the 1-year follow-up (
Table 4 ), suggesting that treatment period gains attributed to STEPPS were maintained. Because not all subjects were assessed through the follow-up period, these analyses were less powerful than the primary analyses through week 20.
Using each subject’s last observation within the follow-up period, those subjects randomly assigned to STEPPS plus treatment as usual were still more likely to be rated “very much” or “much” improved (40.0% versus 15.6%; χ 2 =5.5, df=1, p=0.019). However, subjects’ global self-ratings were not significantly different during the follow-up, with 55.1% of STEPPS plus treatment as usual recipients rating themselves “very much” or “much” improved, compared with 43.8% of those assigned to treatment as usual alone (χ 2 =1.0, df=1, p=0.318). Within the follow-up period, subjects in STEPPS plus treatment as usual were still more likely to reach the Global Assessment Scale score cutoff (>60) (28.0% versus 9.7%; χ 2 =3.9, df=1, p=0.049).
Medication and Individual Psychotherapy
Ninety percent of subjects reported at least one psychotropic medication at baseline. Antidepressants were reported by 42 (65%) of the STEPPS plus treatment as usual recipients and 33 (56%) of the treatment as usual alone group (χ 2 =1.0, df=1, p=0.323). Psychotropic usage significantly decreased during the 20-week treatment period for both groups (from 2.9 to 1.3 medications per subject), but there was no group difference in level of change (Mann-Whitney test: χ 2 =0.1, df=1, p=0.782). Thus, medication usage did not confound study results. Additionally, 63% of STEPPS plus treatment as usual subjects and 54% of treatment as usual alone subjects were receiving individual psychotherapy at baseline. These percentages remained relatively static during the 20-week treatment period.
Indirect Indicators of Efficacy
Subjects were asked to report crisis care utilization within the last month. Because subjects varied in their number of assessments, we report utilization statistics in terms of the number of months per year in which utilization occurred. Thus, for example, we can distinguish a subject with three utilizations over 3 months (i.e., 12 months per year with utilization) from a subject with three utilizations over 6 months (i.e., 6 months per year with utilization). Overall, 35 (28.2%) subjects had at least one hospitalization during the treatment period or follow-up. Subjects randomly assigned to STEPPS plus treatment as usual averaged 1.13 months per year during which hospitalization occurred, and subjects randomly assigned to treatment as usual alone averaged 1.24; the difference was not significant (binomial test: p=0.670). In addition, 43 (34.7%) subjects had at least one emergency department visit during the treatment period or follow-up. Subjects randomly assigned to STEPPS plus treatment as usual averaged 0.97 months per year with at least one emergency department visit, and subjects randomly assigned to treatment as usual alone averaged 1.52; the difference was significant (binomial test: p=0.040). Finally, 60 (48.4%) subjects made at least one crisis call during the treatment period or follow-up. Subjects randomly assigned to STEPPS plus treatment as usual averaged 2.49 months per year during which at least one crisis call was made, and subjects randomly assigned to treatment as usual alone averaged 2.31; the difference was not significant (binomial test: p=0.603).
Suicide attempt and self-harm data were available for 108 of the 124 subjects. Suicide attempts were reported by 24 subjects (22.2%), and self-harm acts were reported by 56 (45.2%) subjects during treatment and follow-up. Nearly all who attempted suicide (88%) also reported self-harm acts. Among those who attempted suicide, the median number of attempts was 1.75 per year, and the mean was 2.60. Among those who reported acts of deliberate self-harm, the median number of acts was 9.8 per year, and the mean was 16.6. Using the Cox proportional hazards model, treatment group was not associated with time to first suicide attempt (χ 2 <0.1, df=1, p=0.994) or first self-harm act (χ 2 <0.1, df=1, p=0.902).
Client Satisfaction Questionnaire-8 total scores at week 20 were significantly higher for the STEPPS plus treatment as usual group relative to the treatment as usual alone group (t=4.7, df=71, p<0.001), with means of 28.2 (SD=4.9) and 22.6 (SD=5.2), respectively, indicating greater satisfaction.
Discussion
STEPPS plus treatment as usual was superior to treatment as usual alone in the treatment of outpatients with borderline personality disorder across a spectrum of illness-specific and global measures. These results are encouraging because they suggest that a relatively brief adjunctive program can deliver clinically meaningful benefits to persons with this disorder and improve their quality of life. STEPPS now joins several other treatment programs supported by empirical evidence and is a reminder that earlier pessimism regarding the treatment of borderline personality disorder was misplaced
(5 –
12) .
This treatment program helped subjects to better understand their personality disorder and gave them skills to cope with it. It may also have provided social support, hope, and therapeutic alliance, which are common factors that may be responsible for benefit from many forms of therapy
(34 –
36) . Further, our test of STEPPS employed features of an effectiveness study suggesting that STEPPS provides “real-world” benefit. For example, subjects were allowed to take psychotropic medication or receive individual therapy and case management.
STEPPS led to broad-based improvements that included the affective, cognitive, impulsive, and disturbed relationship domains assessed by the Zanarini Rating Scale for Borderline Personality Disorder; it also had a robust antidepressant effect. Impulsivity, as measured by the Barratt Impulsiveness Scale, was significantly reduced, as were negative thoughts and feelings and negative affectivity, the latter findings indicating that STEPPS recipients were less likely to feel hopeless and helpless or to have negative self-impressions. These changes reflect the emphasis of the program in that subjects are taught to regulate their intense emotions and maladaptive behaviors. Importantly, improvements were generally maintained during the follow-up, suggesting that subjects learned new skills that they used beyond the treatment period to enhance their quality of life. Nonetheless, there was regression in some scores during the follow-up for STEPPS recipients. Without the support and structure of the group, mild regression may be inevitable in some persons.
Subjects assigned to STEPPS plus treatment as usual had moderate to high levels of satisfaction with the program based on their Client Satisfaction Questionnaire-8 scores, findings congruent with our preliminary data
(16) . Of course, these ratings were obtained from subjects who completed the treatment study, and those who did not may have been less satisfied.
We were unable to confirm our a priori hypotheses regarding a reduction in suicidal and self-harm acts during the 20-week treatment or follow-up, although there were no suicides. Additionally, while there was less crisis utilization among those individuals receiving STEPPS, only the reduction of emergency department visits was statistically significant. It may be that a positive effect on these behaviors requires more than a 20-week program or that more intensive follow-up is needed. To this end, we have developed an adjunctive program designed to follow STEPPS, which we plan to investigate. Reductions in crisis utilization, suicide attempts, and self-harm acts reported by other researchers have generally followed at least 12 to 18 months of active treatment
(6 –
10) . In addition, unlike some studies
(5,
6), we did not require subjects to be suicidal at intake, and the low base rate of suicidal behaviors may have made it difficult to show a treatment effect.
There are several methodological limitations. First, we experienced a relatively high discontinuation rate. High drop-out rates are the bane of borderline personality disorder treatment trials. Bateman and Fonagy
(8,
9) claimed a rate of only 12%, as did Linehan et al.
(6) in their recent dialectical behavioral therapy trial, yet substantially higher rates have been reported by others. Verheul et al.
(7) reported that 34 of 58 subjects (59%) assigned to dialectical behavioral therapy or treatment as usual dropped out. While we encouraged patients to remain in the study, we neither sought a commitment nor made a systematic attempt to reduce nonattendance. Most subjects assigned to STEPPS plus treatment as usual were not regular attendees of our clinic, and lack of “clinic loyalty” may have contributed to dropping out. Additionally, for some subjects, travel to Iowa City for the program, particularly during winter months, may have played a role. Subjects assigned to treatment as usual alone only had to complete periodic assessments, often conducted by telephone. While we intended to conduct blind assessments, we found it nearly impossible to maintain blindness. The convergence of both rater- and patient-administered scales suggests that this may not have been an important deficiency.
Another concern is the possible confounding of results by psychotropic medication. Zanarini
(4) noted that nearly all patients treated for borderline personality disorder receive psychotropic medication. This was true of our subjects. Yet, there were no differences between groups indicating that results favoring STEPPS plus treatment as usual were not because of medication. Similarly, individual psychotherapy did not appear to confound the results.
The paucity of men and minorities does not allow firm conclusions about the effectiveness of STEPPS in these groups. Nor does the study design allow conclusions about the effectiveness of STEPPS relative to other manual-based treatment programs. Additionally, the fact that we did not seek subjects with recent suicidal or self-harm behaviors limits comparison with studies that have actively recruited such persons
(5,
6,
10) .
Additional trials of STEPPS by independent research groups and testing STEPPS in other patient populations should be considered. Future studies should also address premature discontinuation and develop strategies to minimize this limitation.