Since Kraepelin first separated manic depression from schizophrenia, bipolar disorder has been thought of as a good prognosis condition, one not inevitably associated with deterioration and deficits in functioning. Recent studies, however, have pointed to the substantial chronicity of the illness, with patients experiencing symptoms almost 50% of the time, despite adequate treatment
(1) . In addition, residual symptoms persist during interepisode “well” periods in most patients
(1,
2) . This often unfavorable course of illness, which includes the frequent presence of chronic subsyndromal states and associated impairments in cognitive and executive function
(3,
4), likely contributes to the poor psychosocial outcomes associated with bipolar disorder.
Occupational functioning is an essential component of mature adult functioning. Indeed, Erikson writes, “Freud was once asked what he thought a normal person should be able to do well. The questioner probably expected a complicated answer. But Freud, in the curt way of his old days, is reported to have said: ‘Lieben and arbeiten’ (to love and to work)”
(5), thus characterizing work as one of the two key tasks of adulthood.
Unfortunately, the ability to work is an area of functioning that is typically severely compromised by bipolar disorder
(6) . Coryell and colleagues
(7) observed substantial deterioration in employment status across time in patients with major affective illness: impairment was present in all the areas of functioning and did not appear to change significantly with clinical remission. In an observational study evaluating patients during a 1-year follow-up after an acute manic episode, Goetz and colleagues
(8) reported that work impairment was significantly associated with the longitudinal severity of the disorder (e.g., higher number of episodes, suicide attempts, or hospitalizations), a rapid cycling course, the presence and severity of depressive symptoms during the manic episode, substance abuse, and not living with a partner. Our own study of individuals in a bipolar disorder patient registry indicated that up to 64% were currently unemployed, despite relatively high educational attainment
(9) . In addition, patients with bipolar disorder who are employed have a higher number of annual missed work days than individuals without bipolar disorder
(10) and tend to have more deficits in work performance when compared with persons with unipolar depression and with a nationally representative control group
(11) . Unfortunately, most treatment studies demonstrate that poor psychosocial and occupational outcomes often characterize bipolar disorder, despite symptom reduction achieved with pharmacological treatments. These observations have highlighted the importance of developing treatments that specifically address the psychosocial impairments associated with bipolar disorder.
Method
Participants were enrolled in the Maintenance Therapies in Bipolar Disorder study, which was conducted from 1991 to 2002. The study procedures and primary outcomes are described in detail elsewhere
(13) . Patients meeting DSM-III or DSM-IV criteria for an acute episode of bipolar I disorder (depressed, manic, or mixed) were randomly assigned to one of four psychosocial treatment strategies: 1) acute and maintenance interpersonal and social rhythm therapy, 2) acute and maintenance intensive clinical management, 3) acute interpersonal and social rhythm therapy followed by maintenance intensive clinical management, or 4) acute intensive clinical management followed by maintenance interpersonal and social rhythm therapy.
All participants received pharmacotherapy according to a standardized algorithm, which is described in detail elsewhere
(13) . Stabilization was defined as scores averaging ≤7 on both the 17-item Hamilton Depression Rating Scale (HAM-D) and the Bech-Rafaelsen Mania Scale
(14) over the course of 4 consecutive weeks, after which participants moved from the acute to the maintenance treatment phase.
Participants
Participants were eligible for study entry if they were acutely ill, ages 18–60, had a lifetime diagnosis of bipolar I disorder and schizoaffective disorder, manic type, and were experiencing their third or more lifetime affective episode. A score of ≥15 on the 17-item HAM-D or ≥15 on the Bech-Rafaelsen Mania Scale was required for study entry. Patients were excluded if they met criteria for rapid cycling (≥4 episodes/year), borderline or antisocial personality disorder, an active eating disorder, or chronic drug or alcohol abuse or if they had an uncontrolled medical illness that would preclude protocol pharmacotherapy or were pregnant. Of the 175 initial participants, 125 achieved stabilization and entered maintenance treatment. Of those who entered maintenance treatment, a total of 30 individuals withdrew from the study over the subsequent 2 years. A detailed flow chart of subject progress is presented elsewhere
(13) . Occupational functioning was assessed pretreatment (baseline), at the end of acute treatment, and at the end of 1 and 2 years of maintenance treatment. Of the 125 participants who entered the maintenance phase of the trial, occupational functioning ratings were available for 94, 99, 86, and 70 subjects at baseline, start of maintenance treatment, end of 1 year of maintenance treatment, and end of 2 years of maintenance treatment, respectively.
Interpersonal and Social Rhythm Therapy
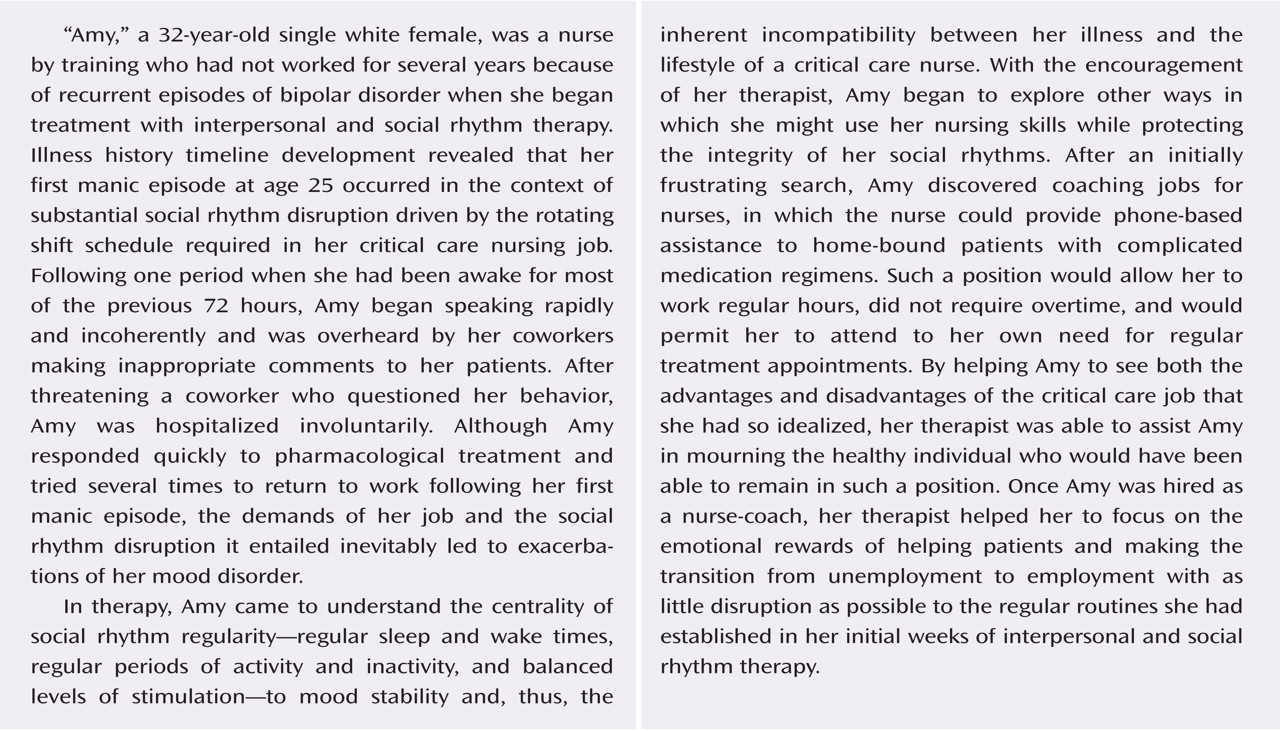
Interpersonal and social rhythm therapy is a modular, manual-based treatment aimed at helping patients stabilize their daily routines and sleep/wake cycles in the hopes of stabilizing endogenous circadian rhythms, gaining insight into the bidirectional relationship between mood and interpersonal events, and resolving interpersonal problems related to grief, role transitions, role disputes, and interpersonal deficits
(15) . The therapy involves four phases. In the initial phase, the clinician collects the history of the illness, completes an interpersonal inventory, provides education about the disorder, and identifies an interpersonal problem area to work on. In the intermediate phase, the therapist helps to implement social rhythm stabilization strategies, strategies to manage affective symptoms, and works on interpersonal problem areas. In the preventative phase, the goals are to consolidate treatment gains and help the patient to identify potential threats to continued stability. The termination phase includes reviewing the patient’s treatment successes as well as areas of vulnerability to future episodes. The intervention is described in detail elsewhere
(12) .
Intensive Clinical Management
Intensive clinical management is a manual-based approach to the medical management of bipolar disorder that was developed based on clinical management strategies employed in the National Institute of Mental Health (NIMH) Treatment of Depression Collaborative Research Program
(16) and in our own earlier study, entitled Maintenance Therapies in Recurrent Depression
(17) . The treatment focuses on patient education about bipolar disorder and its treatments, medication management, side effect/somatic symptom management, and medication adherence. The specific elements of intensive clinical management include 1) education about bipolar disorder, 2) education about the medications used to treat bipolar disorder, 3) education about basic sleep hygiene, 4) careful review of symptoms, 5) careful review of side effects, 6) medical and behavioral management of side effects, and 7) nonspecific support.
Assessments
The diagnosis of bipolar I disorder for participants enrolled before 1995 was made using the Schedule for Affective Disorders and Schizophrenia (SADS)
(18) ; after 1995, the Structured Clinical Interview for DSM-IV (SCID)
(19) was used. Severity of depression and mania were determined with the 17- and 25-item HAM-D and the Bech-Rafaelsen Mania Scale, respectively.
Occupational functioning was assessed using the UCLA Social Attainment Scale
(20), a scale ranging from 1 to 5 (in which 1=high-level functioning), at study entry, at entry into the maintenance phase, and at the end of 1 and 2 years of maintenance treatment. Occupational functioning ratings were available at these four time points for 94, 99, 86, and 70 subjects, respectively.
Statistical Analyses
We used mixed-effects repeated measures analysis to examine the data, with the subject as a random variable and the assessment points (baseline, end of acute treatment, end of 1 year of maintenance treatment, and end of 2 years of maintenance treatment) as fixed variables. Acute treatment assignment and acute treatment by assessment time point interaction were also included in the model. The covariance matrix was unstructured. Vocational functioning scores were also examined by gender.
Results
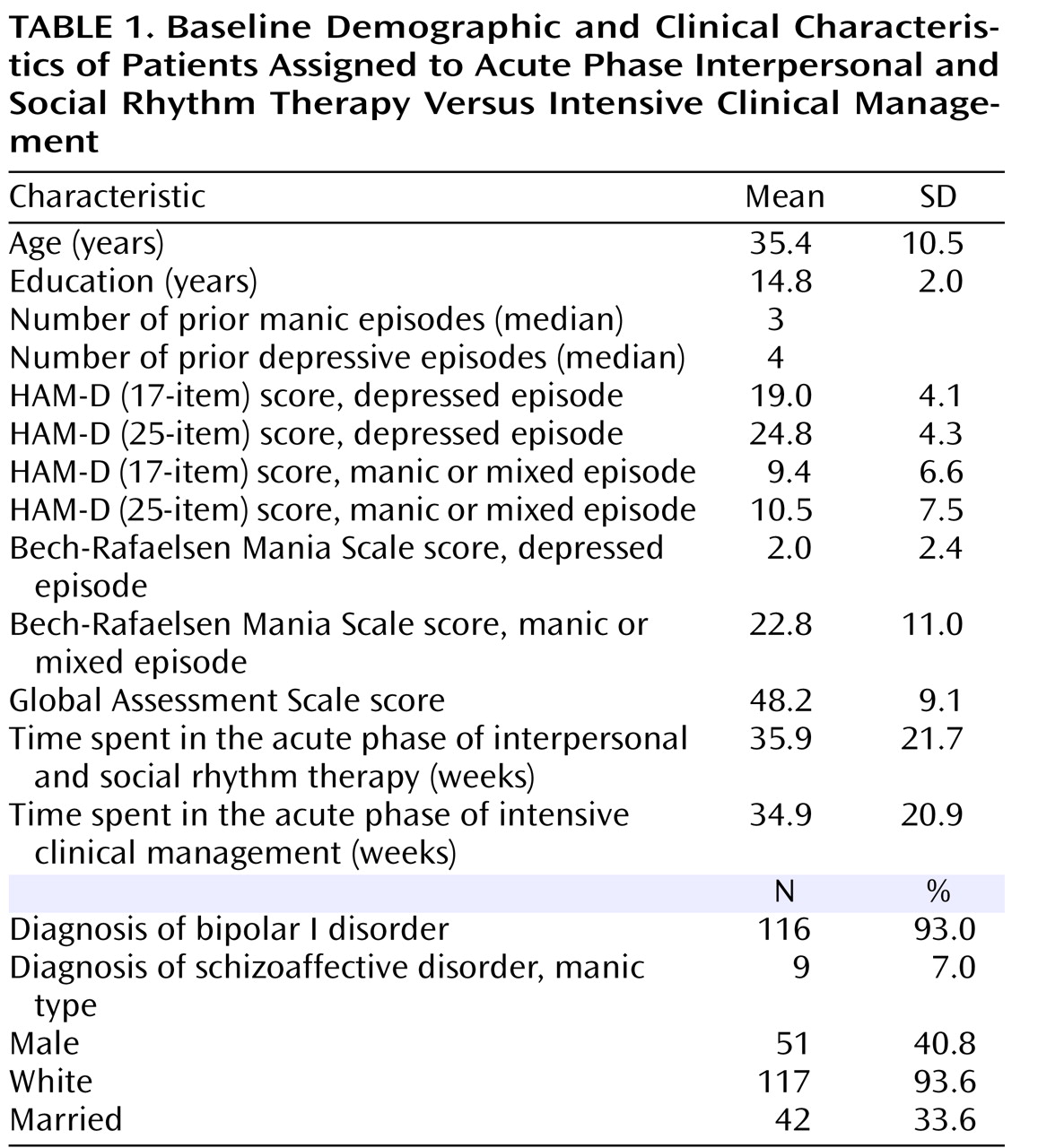
Baseline demographic and clinical characteristics of the sample are shown in
Table 1 . Only 12.8% and 11.7% of patients reported high or moderately high baseline occupational functioning, respectively. The majority of participants reported average (25.5%) or below average (27.7%) functioning, and 22.3% reported poor occupational functioning at study entry. No significant differences in baseline vocational functioning were observed between participants initially assigned to interpersonal and social rhythm therapy and those assigned to intensive clinical management (3.35 [SD=1.30] versus 3.38 [SD=1.37], respectively), nor between male and female participants (3.47 [SD=1.25] versus 3.28 [SD=1.33], respectively). Mean time spent in the acute phase was 35.9 weeks (SD=21.7) for interpersonal and social rhythm therapy and 34.9 weeks (SD=20.9; p=0.79) for intensive clinical management.
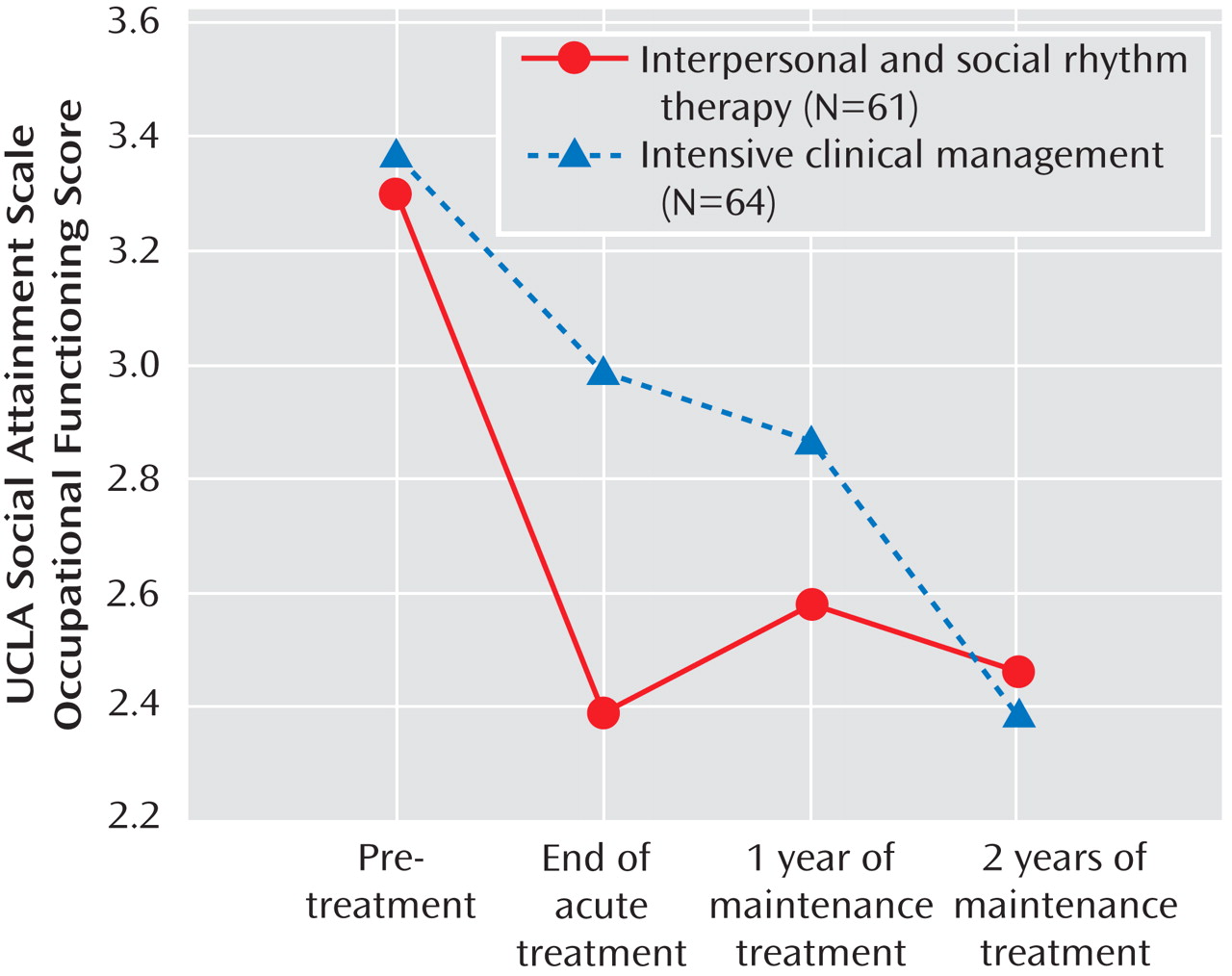
The main effect of initial treatment assignment did not reach conventional levels of statistical significance; however, we did observe a significant initial treatment by time interaction such that participants assigned to acute phase interpersonal and social rhythm therapy showed significantly more rapid initial improvement in occupational functioning than those initially assigned to intensive clinical management (F=4.08, df=1, 111, p=0.046). The improvement tended to be sustained during the maintenance phase, irrespective of the type of psychosocial treatment to which the participant was assigned during that phase. We observed no effect of maintenance treatment assignment. Although participants assigned to intensive clinical management in the acute phase showed much slower improvement in occupational functioning, by the end of 2 years of maintenance treatment their occupational functioning was virtually identical to that of participants assigned to acute phase interpersonal and social rhythm therapy (
Figure 1 ).
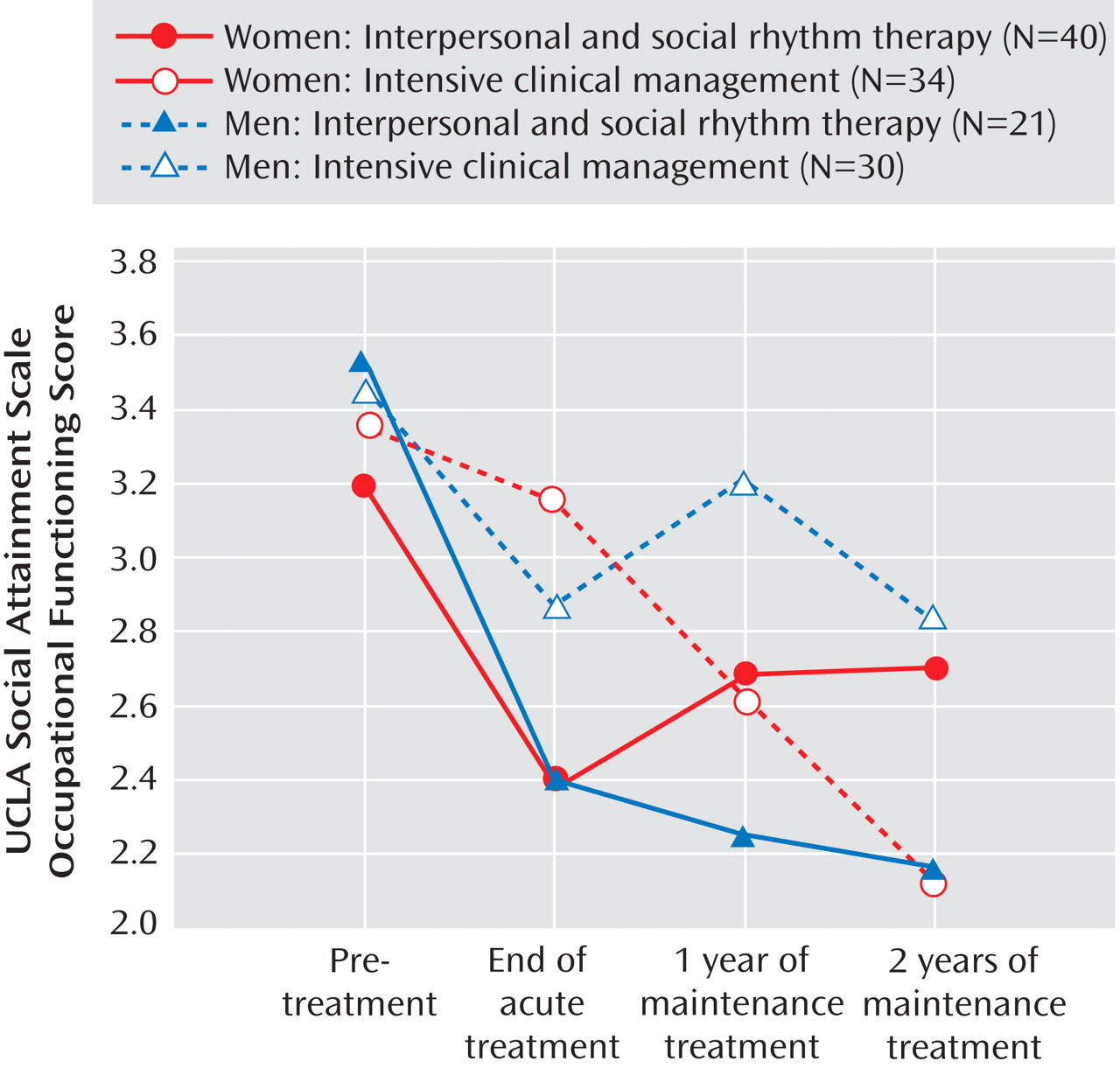
The repeated measures mixed-effects model showed a significant three-way interaction over the four time points among acute treatment assignment, gender, and time (F=3.06, df=3, 104, p=0.032). The analysis was repeated, stratified by gender, and showed a significant treatment by time interaction in female participants (F=4.66, df=3, 64.2, p=0.005) but not in men (F=1.42, df=3, 40.7, p=0.25).
Figure 2 illustrates the observed scores across time by acute phase treatment assignment and gender. The significant interaction among women is accounted for by the difference at the end of the acute treatment phase, with participants initially assigned to interpersonal and social rhythm therapy performing significantly better occupationally than those initially assigned to intensive clinical management.
No significant differences in educational attainment, age, or number of prior depressive or manic episodes were found between male and female participants. Differences were observed, however, in the occupations of men and women. Not surprisingly, all of those categorized as homemakers were women, while men accounted for almost three-fourths of those reporting sales as their occupation. Women who were homemakers showed significantly worse occupational functioning at baseline (t= –3.15, p=0.002) than other occupational groups, but no differences in occupational functioning were observed among the various occupational categories at the subsequent time points.
In order to explore possible explanations for the observed gender difference, we conducted additional analyses to examine whether this difference could be accounted for by improvement among women who were homemakers only (who are, in essence, accountable only to themselves and their families and are not dependent on the evaluation of external employers). We found no evidence that improvement among homemakers only accounted for the gender difference in outcomes (t=1.23, df=45, p=0.23); however, homemakers did improve more on average (0.9 [SD=1.0] versus 0.3 [SD=1.4]).
We also questioned whether this effect could be explained by a history of more antisocial behavior among the male participants (which might have made them less employable, even after symptomatic recovery). Using data from the antisocial personality probes of the SCID, we found no differences between men and women in this study in terms of the number of positive probes for antisocial personality criteria, nor did men and women in this sample differ in terms of the probability of having a lifetime diagnosis of drug abuse or dependence disorder (14% for men versus 18% for women). However, male participants were significantly more likely to have a lifetime diagnosis of alcohol abuse or dependence disorder (36% for men versus 17% for women; χ 2 =7.70, p=0.006).
Finally, we were interested in whether occupational functioning is simply a surrogate measure of clinical outcome, which would mean that our findings were simply a reflection of the better clinical outcomes resulting from initial assignment to interpersonal and social rhythm therapy, as documented in our original report on this trial
(13) . To test whether improvement in occupational functioning was the actual mediator of the longer time to recurrence observed in those initially assigned to interpersonal and social rhythm therapy, we conducted a Cox proportional hazards model, using time to recurrence as outcome and occupational functioning at 1 year as predictor (data not shown). Worse occupational functioning predicted shorter time to recurrence but only explained a small percent of the variation (R
2 =0.056). Thus, the benefits of initial assignment to interpersonal and social rhythm therapy for time to recurrence and for occupational functioning appear to be largely independent effects.
Discussion
Treatments for bipolar disorder traditionally target mood symptoms and focus on preventing both manic and depressive recurrences. There is increasing evidence, however, that simply treating the symptoms of the disorder does not often yield satisfactory results in the wider domains of psychosocial and occupational functioning
(21) . As indicated in the present study, both mania and depression have detrimental and long-lasting effects on general functioning
(7,
8), occupational status, and work performance. On the other hand, the lack of a daily routine structure that comes with being unemployed may increase the risk of recurrence of a mood episode
(22) .
There is growing interest in the role of psychosocial interventions in the management of bipolar disorder, an illness that has been historically considered “purely biological” and, therefore, unlikely to be responsive to psychosocial treatments. As recent evidence has pointed out, psychosocial outcomes resulting from traditional treatment strategies are largely unsatisfactory, and new emphasis has been placed on the role of psychotherapy and psycho-education
(23) .
Interpersonal and social rhythm therapy is designed to target the three important pathways to symptom maintenance and recurrence in bipolar disorder: 1) nonadherence to medication, 2) stressful life events, especially interpersonal events and changes in social roles, and 3) disruptions in social rhythms or routines. It has been shown to be effective in shortening the time to remission of depression
(24), prolonging the time to recurrence
(12), and decreasing suicidality
(25) .
Our results suggest that interpersonal and social rhythm therapy, with its emphasis on amelioration of interpersonal and role functioning, has significantly greater capacity to improve and maintain occupational functioning than a psychoeducational approach with no such emphasis on functional capacities. In addition, the emphasis that is placed on the maintenance of social rhythm regularity in interpersonal and social rhythm therapy may also play a role in helping patients to pace their daily activities in a way that permits successful return to work and maintenance of employment. As we have previously reported, social rhythm stabilization is more likely to take place when interpersonal and social rhythm therapy is administered in the acute treatment phase, regardless of the treatment assignment in the maintenance phase
(13) . Additionally, rhythm stabilization mediated a longer time to recurrence among interpersonal and social rhythm therapy patients during the maintenance phase
(13) .
Even though we did not observe a clear mediator effect of social rhythm stabilization on occupational functioning, we speculate that patients may have been more receptive to the social routine education when they were in the midst of or just beginning to recover from an acute episode.
Interestingly, administering interpersonal and social rhythm therapy in the acute phase of treatment had a differential impact on occupational functioning in men and women. Women who were assigned to acute phase interpersonal and social rhythm therapy showed the most rapid and marked improvement, while men overall showed slower changes in vocational functioning, with those not receiving acute interpersonal and social rhythm therapy performing worse than all other groups. There is limited to no information available on gender-specific outcomes of psychotherapy in bipolar disorder; however, studies of major depression have generally failed to show a clear differential response between men and women to psychotherapy
(26 –
28), and we did not observe a gender difference in time to recurrence in the present study
(13) . We considered whether some behavioral and social differences between men and women with bipolar disorder could explain the gender effect; compared to women, men with bipolar disorder tend to have more legal problems
(29), more behavioral problems during manic episodes
(30), and more antisocial behavior in early life
(31) . By protocol design, none of the participants in this study endorsed full criteria for antisocial personality disorder. There was no difference between men and women in our sample in terms of their report of lifetime antisocial characteristics, as defined by the baseline SCID-II item, nor were men more likely to report lifetime history of drug abuse. Men were, however, more likely to have a lifetime history of alcohol abuse. Although none of the study participants met criteria for current alcohol abuse, this difference in past history may have rendered integration (or reintegration) and functioning in a competitive work environment more difficult for that subset of males (about one-third) and may have contributed to a smaller magnitude of treatment effect when a past history was present.
Not surprisingly, significant gender differences in occupation were present, with women accounting for the totality of homemakers and men accounting for the majority of sales positions. However, no gender differences in educational attainment, age, or number of prior depressive or manic symptoms were observed that could explain the gender difference in benefit from initial interpersonal and social rhythm therapy treatment. Women who were homemakers showed significantly worse baseline occupational functioning, but no differences were observed at the subsequent time points. Given the sample size, it is not possible to clearly examine the differences in benefit of treatment on vocational functioning for each occupational category. In addition, men are underrepresented relative to women in this sample; thus, the lack of statistical power could be a possible explanation for the absence of treatment effect. Thus, while we can rule out several possible explanations for the observed gender effect on improvement in occupational functioning, we are not able to say with confidence why it occurred.
A final question of interest was whether occupational functioning is simply a proxy for symptomatic status and whether the present findings are redundant with our earlier report of longer survival time without a new episode among individuals initially assigned to interpersonal and social rhythm therapy. Our analysis of whether improved occupational functioning mediated time to recurrence suggests that these are independent positive effects of interpersonal and social rhythm therapy treatment.
In summary, although the psychosocial and occupational outcomes of persons with bipolar disorder are often poor, we found that patients who began treatment with a combination of medication management and interpersonal and social rhythm therapy made rapid gains in occupational functioning that were particularly large among women. Perhaps most important, these gains were largely maintained over the subsequent 2 years.