Generalized anxiety disorder is characterized by chronic, pervasive, and uncontrollable worry and is associated with somatic complaints
(1) . The disorder has a lifetime prevalence estimated at 5.7%
(2) and is associated with high rates of comorbidity
(3) .
As shown in several studies and meta-analyses
(4 –
7), cognitive behavior therapy (CBT) is an efficacious and specific treatment for generalized anxiety disorder, according to the definition of efficacy by Chambless and Hollon
(8) .
Few studies have assessed the outcome of short-term psychodynamic psychotherapy for generalized anxiety disorder. Durham and colleagues
(9) compared short-term psychodynamic psychotherapy and CBT in the treatment of generalized anxiety disorder. In that study, however, the two treatments were not equally carefully implemented. In contrast to the CBT practitioners, for example, the therapists applying short-term psychodynamic psychotherapy were not specifically trained in their treatment model. Treatment manuals were used only for CBT. Adherence to the treatment model and competent delivery were not checked for short-term psychodynamic psychotherapy. In that study, short-term psychodynamic psychotherapy served as a kind of “straw man,” as Smith et al. (
10, p. 119) put it. In an open, manual-guided study, Crits-Christoph and colleagues
(11) examined supportive-expressive therapy, as described by Luborsky
(12), which was specifically adapted to generalized anxiety disorder
(13) . Crits-Christoph et al.
(11) reported significant improvements for patients with generalized anxiety disorder after treatment. The within-group effect sizes for improvements in anxiety were large
(14) and of the same size as those previously reported for CBT
(15) . In a randomized, controlled feasibility study, supportive-expressive therapy adapted to generalized anxiety disorder was as effective as a supportive therapy with regard to continuous measures of anxiety, but it was significantly superior with regard to symptomatic remission rates
(16) . However, the sample sizes in that study were relatively small (15 and 16 subjects, respectively), and the study was not sufficiently powered to detect other possible differences between treatments.
In sum, there is a need to study the effects of short-term psychodynamic psychotherapy in generalized anxiety disorder in a more rigorous way. In this article, we shall present a study of short-term psychodynamic psychotherapy based on supportive-expressive therapy. In a randomized, controlled trial, manual-guided short-term psychodynamic psychotherapy was compared to manual-guided CBT in generalized anxiety disorder.
Method
This study was carried out in the Department of Psychosomatic Medicine and Psychotherapy at the Georg-August-University Goettingen between May 2001 and June 2007. It was approved by the ethics committee of the university’s school of medicine. After providing their informed consent, the patients were randomly allocated to the two treatment groups.
An investigator allegiance effect was controlled for by including representatives of both short-term psychodynamic psychotherapy (F. Leichsenring, S.S.) and CBT (E.L., C.W.) in the trial.
The inclusion criteria required subjects to be between 18 and 65 years old and to have a primary diagnosis of generalized anxiety disorder. Primary diagnosis was defined as the most severe mental disorder according to the Anxiety Disorders Interview Schedule—Revised
(17) . The following exclusion criteria were applied: 1) any acute, unstable, or severe axis III medical disorder that might interfere with the successful completion of treatment, 2) any current or past history of schizophrenic disorder, bipolar disorder, or cluster A or B axis II disorder, 3) any current or past neurological disorder, 4) alcohol or substance dependence or abuse, an eating disorder, or major depression in the previous 12 months, and 5) current concomitant psychotherapeutic or psychopharmacological treatment.
Participants
The patients were recruited by referrals of psychotherapists and physicians in private practices and by advertisements and information about the study presented in mass media. All patients were diagnosed by use of the Structured Clinical Interview for DSM-IV (SCID-I and SCID-II)
(18,
19) . All interviews were carried out by an experienced and trained master’s-degree-level clinical psychologist (C.W.). Diagnoses were made by the consensus of at least two experienced clinical psychologists (F. Leichsenring, C.W., E.L.). A total of 231 patients were screened. Fifty-seven patients fulfilled the inclusion criteria and did not meet any of the exclusion criteria (
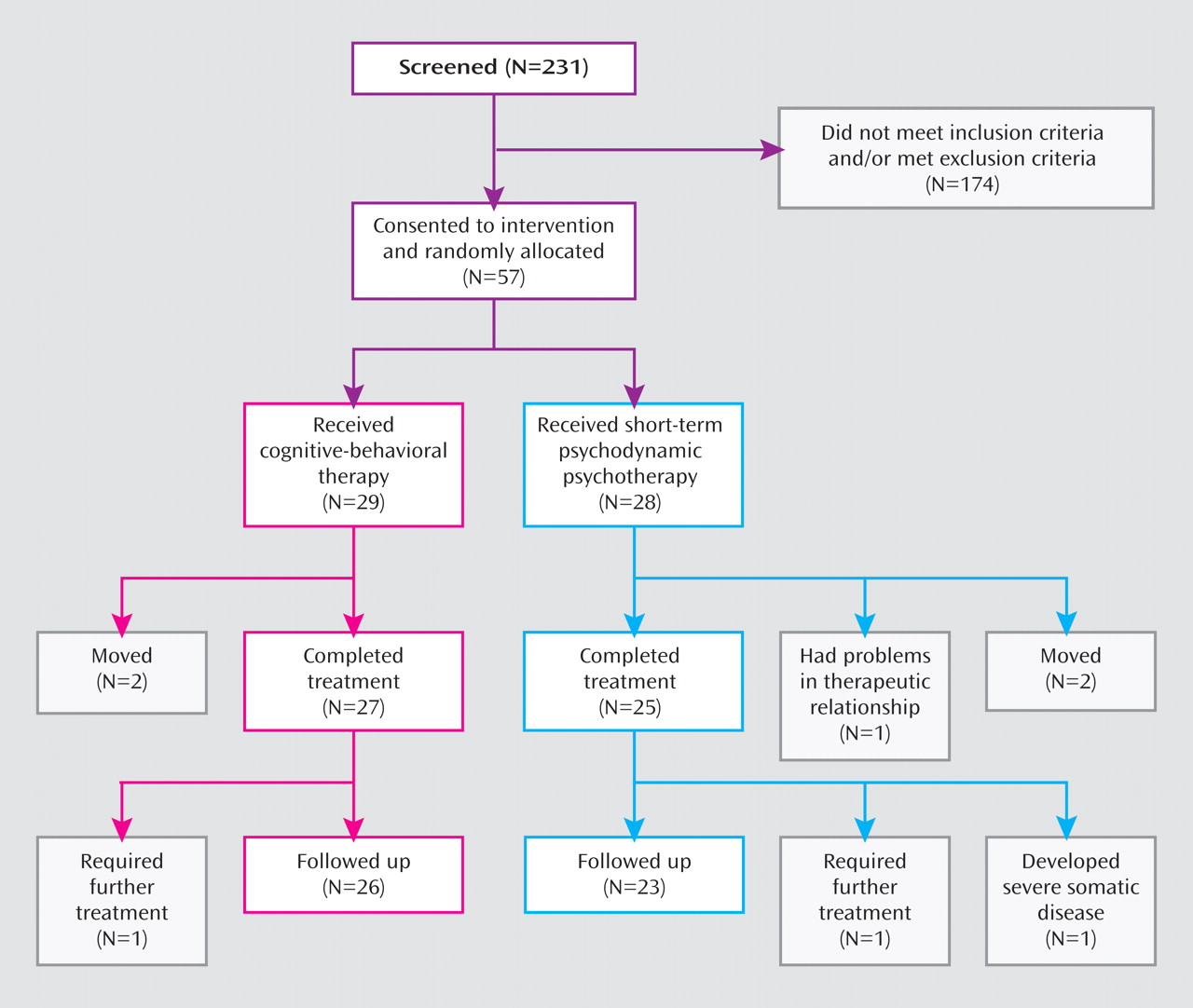
Figure 1 ).
Five patients did not complete their treatment; one patient dropped out because of problems in the therapeutic relationship, whereas the others (two in each treatment group) moved to other cities. At the 6-month follow-up, three additional patients dropped out. Further psychotherapeutic treatment was required by two of these patients (one in each treatment group). The third patient (receiving short-term psychodynamic psychotherapy) developed breast cancer and was unable to pass the follow-up examination. During the 6-month follow-up period, the remaining 49 patients received no psychotherapeutic or psychopharmacological treatment. Our inclusion criteria also required no additional interventions during the treatment period.
The mean age of the intention-to-treat study group (N=57) was 42.5 years (SD=12.3). Most of the participants were female (80.7%) and in permanent partnerships (78.9%). For 16 patients (28.1%), generalized anxiety disorder was the only mental disorder diagnosis, while 41 patients (71.9%) showed one or more comorbid mental disorders. Of the comorbid disorders, other anxiety disorders (35.1%) and depressive disorders (26.3%) were most prominent. Some patients showed adjustment disorders (19.3%), obsessive-compulsive disorders (12.3%), and somatoform disorders (5.3%). Nearly one-half of the patients (45.6%) had undergone psychotherapeutic treatment in the past.
Treatments and Therapists
Both CBT and short-term psychodynamic psychotherapy included up to 30 (50-minute) sessions and were carried out according to treatment manuals. Apart from general strategies, the applied CBT treatment includes the following interventions: relaxation training, problem solving, planning of recreational activities, and homework. The focus of the treatment is on changing and controlling worrying (including worry exposure) and catastrophizing anticipations. Thus, the applied form of CBT described in the treatment manual
(20) combines different techniques as used, for example, by Borkovec and Ruscio
(21) and Brown et al.
(22) .
The applied method of short-term psychodynamic psychotherapy was based on Luborsky’s supportive-expressive therapy
(12), which has been specifically adapted to the treatment of generalized anxiety disorder by Crits-Christoph et al.
(13) . For this study, the treatment manual by Crits-Christoph et al.
(13) was adapted to a 30-session treatment
(23) . The short-term psychodynamic treatment carried out in this study may differ in some ways from how it is usually carried out in U.S. studies
(11,
16) . It can best be described as short-term psychodynamic psychotherapy based on supportive-expressive therapy
(12) . The treatment used in this study focuses on the core conflictual relationship theme associated with the symptoms of generalized anxiety disorder. Emphasis is put on a positive therapeutic alliance. As patients with the disorder are hypothesized to suffer from insecure attachment, a positive therapeutic alliance provides a corrective emotional experience and allows the patient to approach feared situations, both psychologically and behaviorally
(13,
23) . Within a positive therapeutic alliance, it is recommended that therapists encourage new behaviors, including approaching feared situations, which is consistent with Freud’s recommendations
(24) for the treatment of phobia. The experiences the patient has when approaching feared situations are used to work on the core conflictual relationship theme, e.g., modify the expected responses from others. Thus, although the approaches of CBT and short-term psychodynamic psychotherapy are clearly different regarding the therapeutic procedures, the patient is encouraged in both forms of psychotherapy to approach feared situations, but for different reasons (changing catastrophizing anticipations versus changing the core conflictual relationship theme).
The mean number of sessions for the patients who completed CBT was 28.8 (SD=3.4), and for short-term psychodynamic psychotherapy it was 29.1 (SD=3.1). The treatments were carried out by nine licensed psychotherapists (including R.K.) in independent practice who regularly apply either CBT or psychodynamic therapy. Three of the nine psychotherapists were women. The mean age of the therapists at the beginning of the study was 47.9 years (range, 41 to 53 years). The average length of their professional experience as psychotherapists was 18.7 years (range, 12 to 30 years) for the CBT therapists and 16.3 years (range, 4 to 26 years) for the psychodynamic therapists. In contrast to the psychodynamic therapists, the CBT therapists were in general familiar with the use of treatment manuals. Throughout their professional experience they had practiced the specific interventions included in the applied CBT manual. All therapists were specifically trained in the use of the respective treatment manuals by the developers of the German versions of the manuals (F. Leichsenring, E.L.).
Implementation of the treatment manuals, including adherence to the manuals and competent delivery of the interventions, was ensured for each group of therapists by continuous group supervision, which was carried out every month by supervisors (F. Leichsenring, E.L.) who were highly experienced in CBT or psychodynamic therapy and highly familiar with the respective treatment manual. The supervision included reading and discussing the manual and talking over audiotaped cases or special treatment situations.
All of the sessions were audiotaped. From each treatment included, one session was randomly selected and rated by nine independent raters who were provided with extensive information about the two treatment manuals, including their specific treatment elements. Each of the selected sessions was rated blindly by three to eight raters (including U.J., H.K., F. Leweke) with regard to the type of treatment that was applied. The raters identified 26 (89.7%) of 29 CBT sessions correctly as the form of therapy described in the CBT manual and 24 (85.7%) of 28 short-term psychodynamic psychotherapy sessions correctly as the form of therapy described in the short-term psychodynamic psychotherapy manual (overall rate of correct identification, 87.7%). A closer look at the misidentified treatment sessions showed that in these sessions, therapists of both types encouraged the patients to approach feared situations. As previously described, both approaches address feared situations, but they use different rationales. The kappa value for agreement beyond chance was 0.76
(25), which can be considered as indicating excellent agreement beyond chance
(26) . These results suggest that the treatments were carried out in good accordance with the respective manuals.
Assessment and Measures
The patients were assessed at baseline, at the end of treatment, and 6 and 12 months after end of the treatment. The results of the 12-month follow-up will be reported later.
As the primary outcome measure, the Hamilton Anxiety Rating Scale (HAM-A)
(27) was used. It includes 14 items that are each rated on a 5-point scale. The scale was rated by three specifically trained, independent, and blinded raters (including C.W.). In the case of divergent ratings, the raters discussed the findings until consensus was reached.
In addition, we applied several self-report measures for which reliability and validity have been demonstrated. Worry was assessed by the Penn State Worry Questionnaire
(28) . Trait anxiety was assessed by the State-Trait Anxiety Inventory
(29) . For other measures of anxiety, we used the Beck Anxiety Inventory
(30) and the anxiety scale of the Hospital Anxiety and Depression Scale
(31) . Severity of depression was assessed by the Beck Depression Inventory (BDI)
(32) . Interpersonal problems were assessed by using the Inventory of Interpersonal Problems, circumplex version
(33) .
Data Analysis
Data were analyzed by using SPSS version 16.0 (SPSS, Chicago). The baseline clinical and demographic variables of the two treatment groups were compared by chi-square tests for dichotomous variables or t tests for continuous variables. Differences between the two treatment groups at baseline in scores on the HAM-A, Penn State Worry Questionnaire, State-Trait Anxiety Inventory, Beck Anxiety Inventory, Hospital Anxiety and Depression Scale anxiety scale, BDI, and Inventory of Interpersonal Problems were examined by one-way analyses of variance (ANOVAs).
The outcomes of CBT and short-term psychodynamic psychotherapy were examined by repeated-measures ANOVAs. In the case of a significant group-by-time interaction, post hoc t tests were applied. Analyses were performed for posttreatment and follow-up assessments. Intention-to-treat analysis (N=57) was employed by using the last observation carried forward. In addition, we conducted a completer analysis (N=52) for all patients who completed their psychotherapy as expected. For the primary outcome measure specified a priori (HAM-A score), alpha was not adjusted. For this scale, a two-tailed alpha level of 0.05 was used in statistical tests. For the secondary outcome measures, alpha was set to 0.01 (0.05/5) in order to protect against type I error inflation.
Within-group effect sizes were assessed by dividing the difference between the pretreatment and posttreatment or follow-up score by the pooled standard deviation at baseline
(14) .
Results
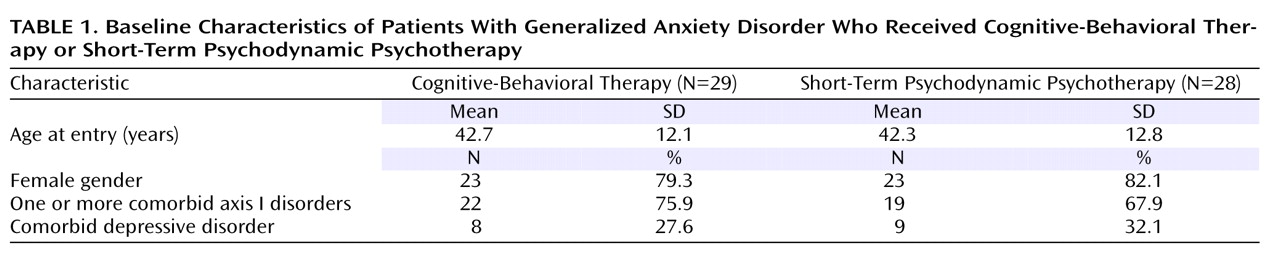
No significant differences were found in clinical or demographic variables between the two treatment groups at baseline (
Table 1 ). Furthermore, the two treatment conditions did not differ significantly with regard to dropout rates during treatment (χ
2 =0.01, df=1, p=0.91). In
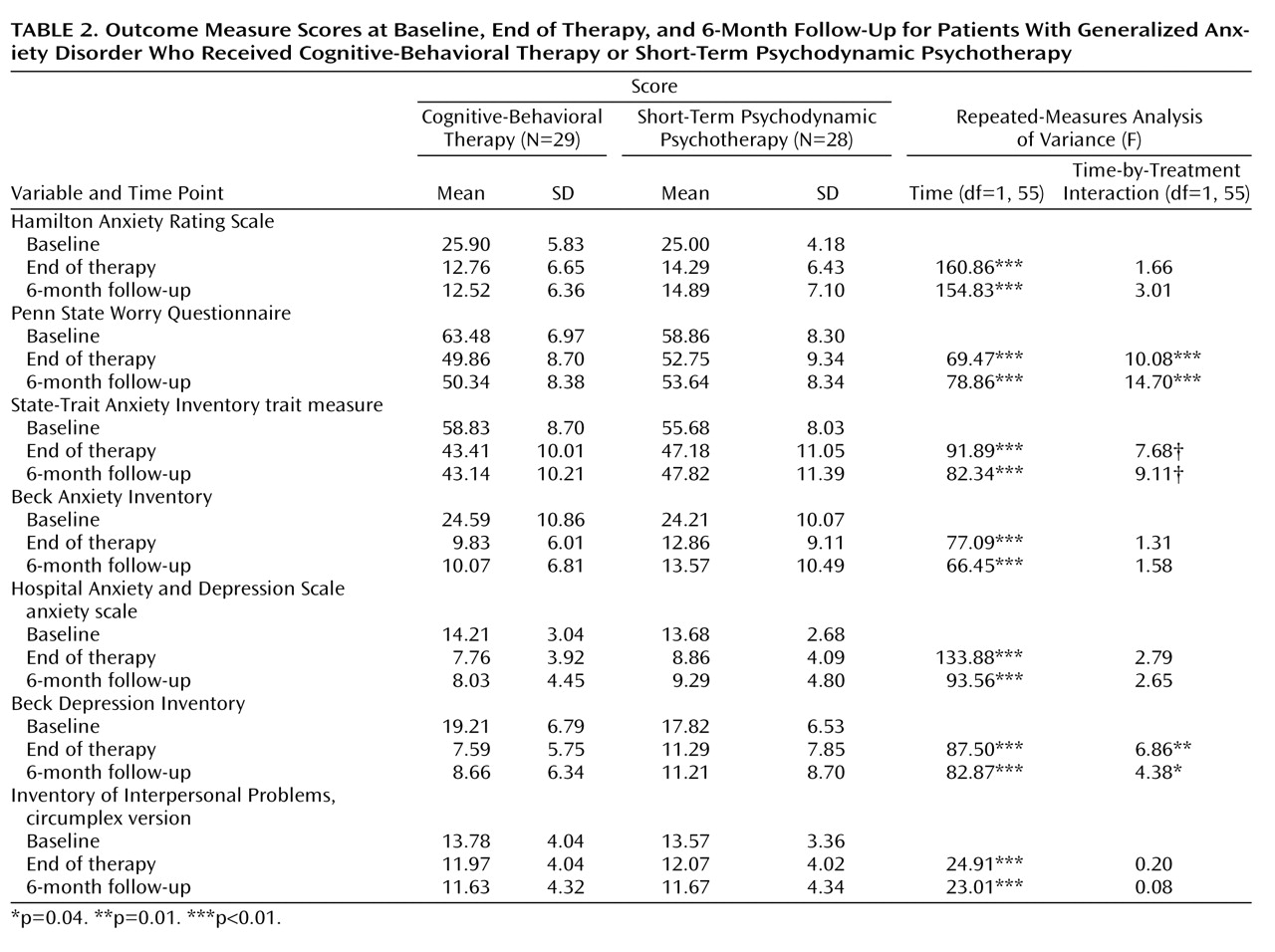
Table 2, scores on the outcome measures are presented for the intention-to-treat group.
One-way ANOVAs showed no significant differences between the two treatment groups at baseline on the HAM-A (F=0.44, df=1, 55, p=0.51), Penn State Worry Questionnaire (F=5.21, df=1, 55, p=0.03), State-Trait Anxiety Inventory trait measure (F=2.01, df=1, 55, p=0.16), Beck Anxiety Inventory (F=0.02, df=1, 55, p=0.89), Hospital Anxiety and Depression Scale anxiety scale (F=0.48, df=1, 55, p=0.49), BDI (F=0.62, df=1, 55, p=0.44), and Inventory of Interpersonal Problems (F=0.04, df=1, 55, p=0.84).
The outcomes of the two treatments were compared by repeated-measures ANOVAs (
Table 2 ). For the posttreatment data, significant effects of time were found for all outcome measures, indicating significant improvements. This was also true for all outcome measures at the 6-month follow-up. Examination of the completer group yielded similar results.
The interactions of time and group at the end of treatment were not significant for the HAM-A, Beck Anxiety Inventory, Hospital Anxiety and Depression Scale anxiety scale, or Inventory of Interpersonal Problems (
Table 2 ), indicating no differences in treatment outcome between CBT and short-term psychodynamic psychotherapy. Significant time-by-group interactions did emerge for the Penn State Worry Questionnaire, State-Trait Anxiety Inventory trait measure, and BDI. At the 6-month follow-up, no significant time-by-group interaction was found for the HAM-A, Beck Anxiety Inventory, Hospital Anxiety and Depression Scale anxiety scale, BDI, or Inventory of Interpersonal Problems, but significant interactions emerged for the State-Trait-Anxiety Inventory trait measure and Penn State Worry Questionnaire. Analyses of the completer group yielded no divergent results.
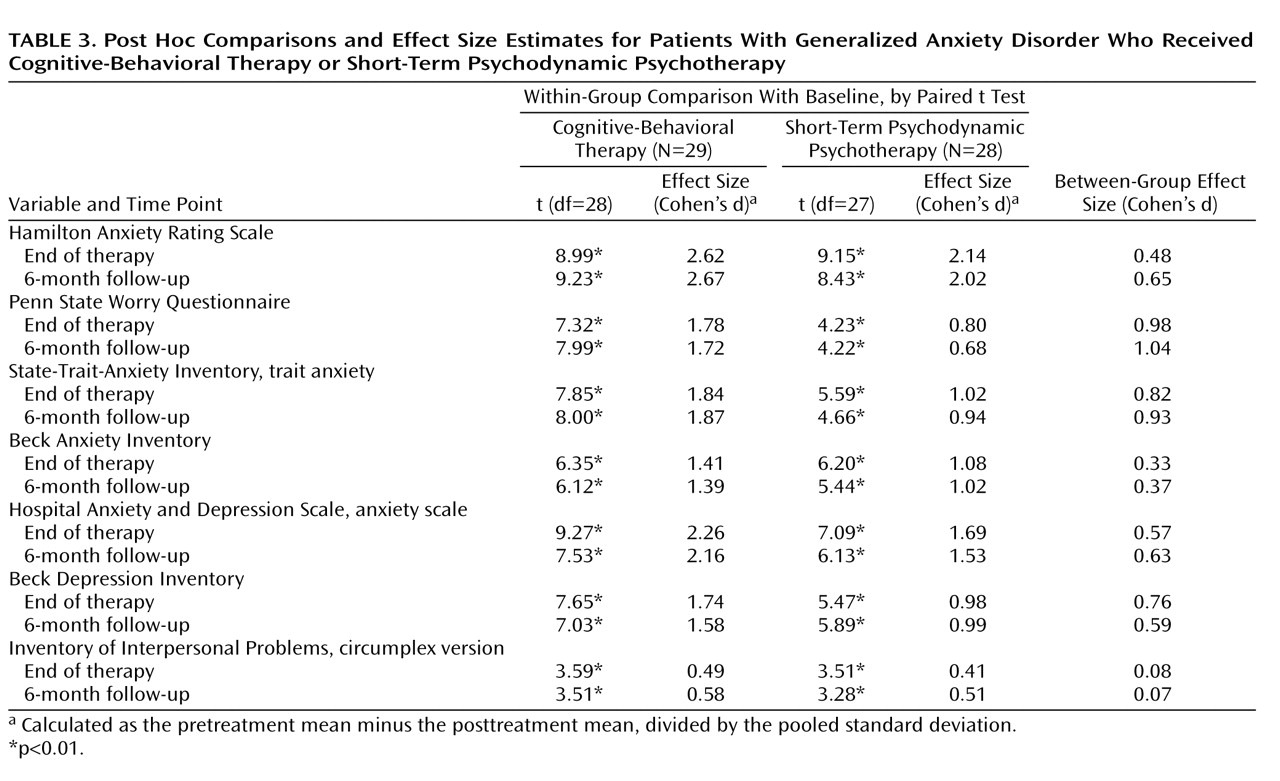
The results of the post hoc two-tailed t tests indicated that CBT yielded significantly larger treatment effects for the Penn State Worry Questionnaire (t=3.19, df=52, p<0.01), State-Trait Anxiety Inventory trait measure (t=2.78, df=52, p<0.01), and BDI (t=2.63, df=52, p=0.01) after treatment. This was also true at the 6-month follow-up for the Penn State Worry Questionnaire (t=3.86, df=51, p<0.01) and State-Trait Anxiety Inventory (t=3.03, df=54, p<0.01). Superiority of CBT in these measures was associated with large between-group effect sizes in favor of CBT (
Table 3 ).
Repeated-measures ANOVAs testing for differences between posttherapy and follow-up scores did not reveal significant main effects of time or significant time-by-group interactions (p>0.24).
All within-group effect sizes for measures of anxiety and depression were large (≥0.80) according to Cohen
(14), except for the effect of short-term psychodynamic psychotherapy on the Penn State Worry Questionnaire score at follow-up (d=0.68,
Table 3 ). For the Inventory of Interpersonal Problems the effect sizes were medium in both treatments. At the 6-month follow-up, the treatment effects were maintained.
Discussion
In this randomized, controlled trial, short-term psychodynamic psychotherapy and CBT were compared in the treatment of generalized anxiety disorder. With regard to the severity of anxiety symptoms at baseline, the patients in this study were comparable to those in other treatment studies; for example, pretreatment scores on the HAM-A have ranged from 23.21 to 25.83
(34) and from 21.8 to 26.8
(35), and scores on the State-Trait Anxiety Inventory have ranged from 57.34 to 58.43
(34) and from 49.8 to 52.2
(35) .
Both treatments were associated with significant improvements in measures of anxiety and depression. For both methods, the within-group effect sizes were comparable to or even larger than those in several other studies
(11,
15,
34,
35) . For the primary outcome measure (HAM-A) and two other measures of anxiety (the Beck Anxiety Inventory and the Hospital Anxiety and Depression Scale anxiety scale) and for interpersonal problems (Inventory of Interpersonal Problems), no significant differences in outcome between the two treatments were found. However, CBT was superior in measures of trait anxiety (State-Trait Anxiety Inventory), worrying (Penn State Worry Questionnaire), and depression (BDI). With regard to descriptive statistics, the between-group effect sizes were in favor of CBT. Thus, it is possible that more differences between the two treatment conditions exist but that the groups were not large enough to permit detection. This is a limitation of our study. As in many studies of psychotherapy research, this was due to limitations in funding. Future randomized, controlled trials comparing the outcome of psychodynamic psychotherapy with results from other active forms of psychotherapy should be carried out with larger study groups.
In contrast to short-term psychodynamic psychotherapy, a core element in the applied method of CBT is modification of worrying. This specific difference between the treatments may explain the superiority of CBT on the Penn State Worry Questionnaire and, in part, on the State-Trait Anxiety Inventory measure of trait anxiety; the latter also contains several items related to worrying. The results presented here suggest that the outcome of short-term psychodynamic psychotherapy in generalized anxiety disorder may be further optimized by employing a stronger focus on the process of worrying. In psychodynamic psychotherapy, worrying can be conceptualized as a mechanism of defense that protects the subject from fantasies or feelings that are even more threatening than the contents of his or her worries
(36) .
As CBT focuses explicitly on changing cognitive processes such as worrying or automatic thoughts, using the Penn State Worry Questionnaire as an outcome measure may tailor outcome measurement specifically to the effects of CBT. In this context, it is of interest that scores on the Penn State Worry Questionnaire did not show significant correlations to scores on the HAM-A (r=0.16) or the Beck Anxiety Inventory (r=0.16) in this group of patients with generalized anxiety disorder (N=57). In contrast, the Penn State Worry Questionnaire scores did correlate significantly with those on the State-Trait Anxiety Inventory (r=0.66, p<0.0001). As just noted, several items of the State-Trait Anxiety Inventory trait measure are related to worry. These correlations suggest that the Penn State Worry Questionnaire and, in part, the State-Trait Anxiety Inventory trait measure tap other, more cognitive aspects of anxiety than does the HAM-A or Beck Anxiety Inventory. The items of the latter two instruments suggest that these two instruments tap more somatic aspects of anxiety. On these two measures of anxiety, the treatments did not differ significantly.
The specificity of pathological worry in generalized anxiety disorder has been questioned by several authors
(37) . Thus, the superiority of CBT to short-term psychodynamic psychotherapy for comorbid depression (BDI) found at the end of treatment may reflect the affinity of anxiety and depression in terms of worrying and rumination
(38) . As noted earlier, these cognitive aspects are typically addressed by CBT.
It is common practice in psychotherapy research to use the total score on the Inventory of Interpersonal Problems. However, even in homogenous diagnostic groups, different interpersonal subtypes can be found
(39) . These subtypes do not differ in levels of symptom severity or comorbid diagnoses, but they exhibit differences in the improvement of interpersonal problems (unpublished data). Thus, studying changes in the total score on the Inventory of Interpersonal Problems provides only limited information and differences between the two treatments regarding improvements in interpersonal problems may exist. Furthermore, the treatments may be able to yield more than only medium improvements in interpersonal problems.
CBT has a long tradition of treating anxiety disorders by manual-guided therapy. A large number of randomized, controlled trials of CBT for anxiety disorders, including generalized anxiety disorder, have been carried out. For short-term psychodynamic psychotherapy, we believe that this is the first randomized, controlled trial for generalized anxiety disorder. The results are promising, but further studies are required in order to refine and enhance the efficacy of this form of psychotherapy.