The worst possible outcome of major depressive disorder is suicide. Among inpatients, the risk of completed suicide is as high as 20-fold compared with the normal population (
1). Approximately one-half of those who complete suicide have attempted suicide at least once before (
2). The lifetime risk of a nonfatal suicide attempt in major depressive disorder is estimated at 16%–40% (
3,
4). Suicide attempts are an important proxy outcome when investigating risk factors for suicide.
In earlier studies, risk factors for suicide attempts (
3–
14) have included a history of attempt by the patient or suicide in the family (
3,
5–
10), female gender (
10), younger age (
7,
11), presence of an episode of major depression (
9), early age at onset (
3), severe or recurrent depression or failure to achieve remission (
8,
9), hopelessness (
7,
10), suicidal ideation (
7,
10,
13), melancholia (
4), psychotic symptoms (
4,
14), comorbid personality disorder (especially borderline personality disorder) (
10), alcohol dependence or misuse (
3,
5–
7,
10,
11), chronic physical illness (
5), aggressive or impulsive traits (
3,
6,
7,
10,
13), cigarette smoking (
7,
10), and social factors (
3,
8,
10–
12). Risk factors for completed suicide (
15–
17) have been male gender, family history of suicide, hopelessness, suicidal ideation, psychotic symptoms, comorbid personality disorders, alcohol dependence or misuse, and anxiety disorders. In a comprehensive review of prospective studies of suicidal behavior, past suicidal behavior, recurrent or refractory depression, and comorbid alcoholism were the most robust predictors (
4). The paradigmatic stress-diathesis model by Mann et al. (
10,
13) conceptualizes suicidal acts as the outcome of the balance between trait- and state-related predisposing and protective factors.
The stress-diathesis model is a valid conceptual framework, but it has one significant limitation: it does not account for the role of time. As we have shown elsewhere (
18), temporal variations in risk states, such as depression, and time spent in them are likely to be important determinants of cumulative overall risk for suicidal acts. To our knowledge, no previous long-term study on major depressive disorder has linked information on suicide attempts to patients' concurrent clinical state and cumulative exposure to risk states. Longitudinal studies combining life chart methodology with precise timing of attempts are scarce. Thus, the relative importance (effect size) of state versus trait factors has remained elusive. In addition, most previous studies exhibited other epidemiologically important limitations, having been conducted within predominantly inpatient settings (
3,
5,
6,
9,
10,
12,
13,
17), having relatively small sample sizes (
5,
9,
14), or having investigated populations with diagnostically mixed affective disorders (
6,
7,
15,
16). Therefore, the generalizability of their findings to other settings or populations or their power to detect risk factors may be limited.
We have previously reported factors associated with suicidal ideation and suicide attempts cross-sectionally as well as an 18-month analysis of longitudinal variations in the risk of suicide attempts among psychiatric patients with major depressive disorder (
8,
11). The risk of attempts was almost eightfold during major depressive episodes compared with periods of full remission and effectively predicted by the time spent depressed, previous suicide attempts, and lack of a partner. In another study (Jorvi Bipolar Study), we found the incidence of attempts to vary markedly between illness phases among bipolar disorder patients, with mixed and depressive phases involving the highest risk per time, and time spent in high-risk illness phases to be the major determinant of overall risk for suicide attempts among these patients (
18).
In the present prospective 5-year study, our aim was to investigate variations in incidence of attempted suicide among patients in major depressive episodes, partial remission, and full remission and whether other risk and protective factors modify this risk. We hypothesized that the rate of incidence would be highest during major depressive episodes and that comorbid substance use, cluster B personality and anxiety disorders, perceived level of social support, and previous suicide attempts would influence the risk.
Method
The Vantaa Depression Study is a collaborative depression research project conducted by the Mood, Depression, and Suicidal Behavior Unit of the National Institute for Health and Welfare, Helsinki, Finland, and the Department of Psychiatry, Peijas Medical Care District, Vantaa, Finland (
19). The Department of Psychiatry at Peijas Hospital provides secondary care psychiatric services to all residents of Vantaa (169,000 inhabitants in 1997). The Ethics Committee of Helsinki University Central Hospital approved the study protocol. The background and methodology of the Vantaa Depression study have been reported in detail elsewhere (
19–
21).
Screening and Baseline Evaluation
In the first phase of the study, 806 psychiatric patients were screened for the presence of depressive symptoms during an 18-month period, starting from February 1, 1997. Of the 703 eligible subjects, 542 (77%) agreed to participate and gave their written informed consent after the procedure had been fully explained (
19). In the second phase, a researcher, using the World Health Organization Schedules for Clinical Assessment in Neuropsychiatry, 2.0 (
22), interviewed these consenting patients, 269 of whom were diagnosed as having DSM–IV major depressive disorder and included in the study. All baseline interviewers received relevant training by a World Health Organization certified training center. Diagnostic reliability was investigated using 20 videotaped diagnostic interviews. The kappa coefficient for major depressive disorder was 0.86 (range=0.58–1.0), with a 95% agreement rate. The Structured Clinical Interview for DSM–III–R personality disorders (SCID–II) was used to assess diagnoses on axis II (
23). The baseline measurements were the 17-item Hamilton Depression Rating Scale (HAM–D) (
24), 21-item Beck Depression Inventory (BDI) (
25), Beck Anxiety Inventory (
26), Beck Hopelessness Scale (
27), Beck Scale for Suicide Ideation (
27), Social and Occupational Functioning Assessment Scale (
29), Social Adjustment Scale–Self-Report (
30), Interview for Recent Life Events (
31), Interview Measure of Social Relationships (
32), Perceived Social Support Scale–Revised (
33), and Eysenck Personality Inventory (
34). In addition, the number of chronic medical disorders (axis III) was investigated with a checklist.
Follow-Up Evaluation
After baseline, subjects were investigated at 6 months, 18 months, and 5 years. Of the 269 subjects with current major depressive disorder initially included in the study, 229 participated in the 6-month follow-up evaluation, 207 in the 18-month follow-up evaluation, and 182 in the 5-year follow-up evaluation. All available medical and psychiatric records were used to complement the interview data. The subjects were prospectively followed up with a life chart, and BDI items were rated monthly until month 6. The outcome of major depressive disorder and comorbid disorders was then investigated at 6 and 18 months using repeated Schedules for Clinical Assessment in Neuropsychiatry and SCID–II interviews. In the 5-year follow-up interview, we used the Structured Clinical Interview for DSM–IV–TR Axis I Disorders (
35) instead of the Schedules for Clinical Assessment in Neuropsychiatry. All observer and self-report scales were included at the follow-up assessments.
The diagnoses and timing of depressive episodes were based on the aforementioned structured interviews as well as patient records. A graphic life chart was created after reviewing with the subject all information from the follow-up period. The life chart was based on DSM–IV criteria and definitions. In addition to symptom ratings and visits with attending personnel, we also inquired about change points in psychopathological states, using probes related to important life events, to improve the accuracy of the assessment. Our life chart method was similar, but not identical, to the Longitudinal Interval Follow-Up Evaluation methodology developed by Keller et al. (
36) and used in the Collaborative Depression Study of the National Institute of Mental Health. Time after the first baseline interview was divided into the following three periods: 1) full remission (none of the nine major depressive episode criteria symptoms), 2) partial remission (one to four of the nine symptoms), and 3) major depressive episode (five or more of the nine symptoms). Occurrence of a suicide attempt before the baseline interview and during the follow-up evaluation was based on both the interview and psychiatric records. The attempts were timed and placed on the life chart. By definition, a suicide attempt had to involve at least some degree of intent to die.
Information on 249/269 subjects (92.6%) was included in the analyses of risk of suicide attempts. Those dropping out were subjects who did not participate in any follow-up evaluation (N=20). In addition, over the 5-year follow-up assessment period, 29 subjects were diagnosed with bipolar disorder, one was diagnosed with schizophrenia, and two were diagnosed with schizoaffective disorder. These subjects remained in the cohort until they were censored at the change of diagnosis. By the end of the 5-year evaluation period, 10 subjects had died, one with bipolar disorder. The median follow-up time was 5.2 years (SD=2.0) from baseline, with 1,017.9 patient-years altogether. Compared with participants who remained in the study, at baseline those dropping out were younger (mean age: 33.0 years [SD=9.1] versus 40.1 years [SD=11.0]; t=2.81, p=0.005), had a lower age at onset (mean age: 27.1 years [SD=8.8] versus 31.8 years [SD=12.7]; t=2.22, p<0.04), more often had dysthymia (35.0% versus 10.0%; χ2=11.0, df=1, p=0.001) and panic disorder with agoraphobia (20.0% versus 6.4%; χ2=4.96, df=1, p<0.03), had more antisocial personality disorder symptoms (z=–2.73, p=0.006), perceived less social support (t=2.01, p<0.05), were more often unemployed (70.0% versus 37.9%; χ2=7.93, df=1, p=0.005), and were less often married or cohabiting (80.0% versus 47.4%; χ2=7.87, df=1, p=0.005). However, the dropouts did not differ in terms of suicide attempts or suicidal ideation at baseline or before entry.
Statistical Analyses
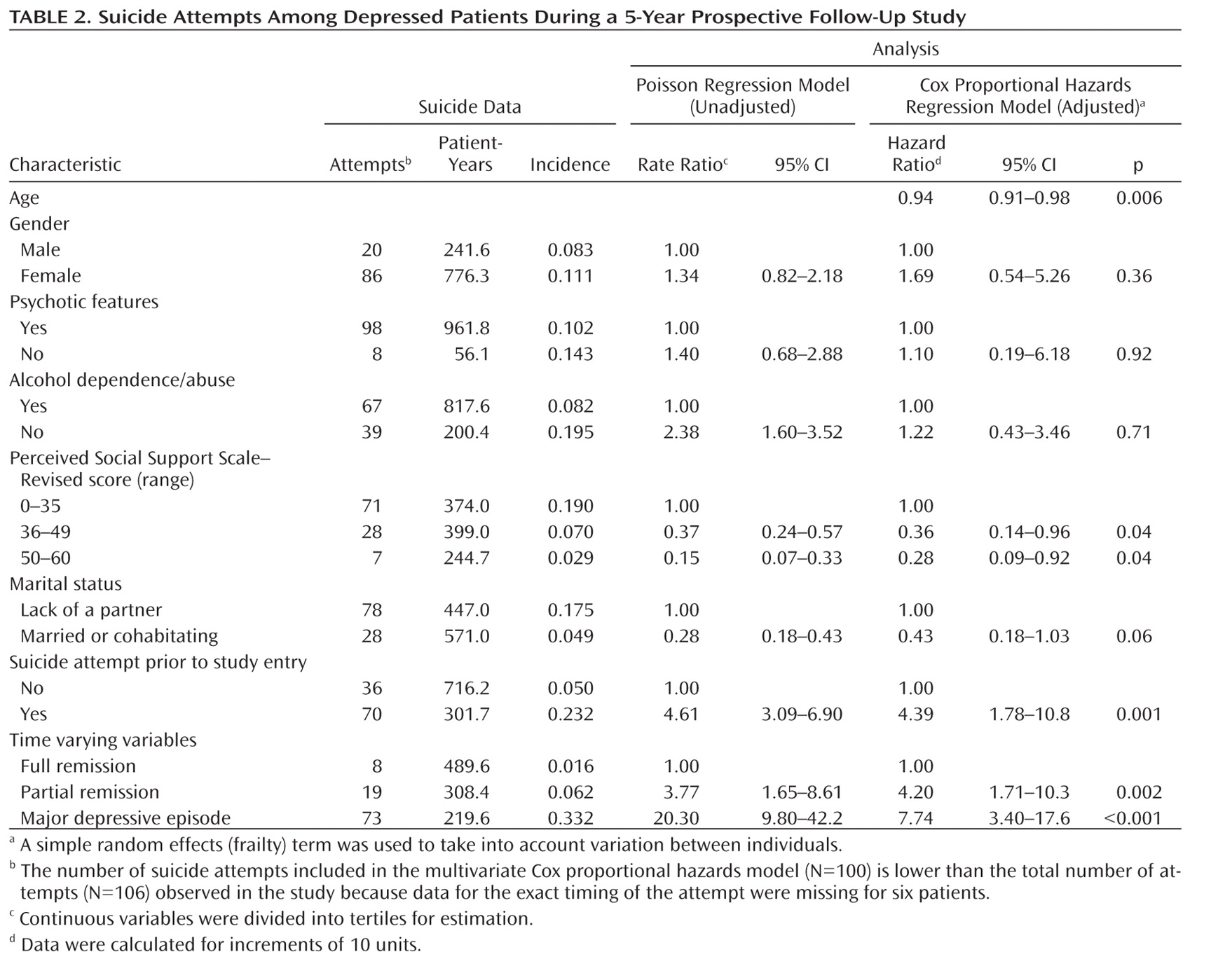
Subjects who attempted suicide during the follow-up period were compared with subjects who did not, using the chi-square test with Yates' continuity correction or Fisher's exact test as appropriate. In comparisons of continuous variables, the two-sample t test was used for variables with normal distribution, and the Mann-Whitney and Kruskal-Wallis tests were used for non-normal distribution. Our multivariate analyses were based on the hypotheses. After detailed univariate analyses, we chose predictors for our final models by considering their clinical and statistical validity, significance, and relevance in representing a domain of risk factors. We omitted the statistically nonsignificant variables from the final models, but the analyses were adjusted for age and gender.
The Poisson regression model was used to investigate univariate rate ratio for explanatory variables for suicide attempts. Cox proportional hazards regression model was used to investigate association between time varying and fixed (time invariant) explanatory variables and hazards of suicide attempts. The association between the concurrent level of depression (full remission, partial remission, or major depressive episode) and suicide attempts in the life chart was analyzed using the level of depression as a time varying covariate. We included a simple random effects (frailty) term in the Cox model to take into account variation between individuals (
37). For each individual, the follow-up assessment was divided into time periods in which the value of the time varying variable (i.e., level of depression) was constant. Thus, the follow-up evaluation consisted of several contiguous time periods, each defined by a specific entry and exit time. Because there were several observations (time periods) for the same individual, robust sandwich variance estimator was used. In the model, suicide attempts before follow-up assessment, suicide ideation at baseline, highest values for the Beck Anxiety Inventory and HAM–D measurements, psychotic features, alcohol use disorders, number of cluster B symptoms (suicide item excluded), marital status, hopelessness (Beck Hopelessness Scale rating), perceived social support, and size of social network (during the episode of lowest depression) were used as fixed covariates. For continuous variables (age; HAM–D, Beck Anxiety Inventory, and Beck Hopelessness Scale ratings; perceived social support; and size of social network), hazard ratios were calculated for 10-unit increments. The interactions between the time varying phase and other risk factors were tested using the Cox model with the likelihood ratio test. The results of the Cox model are presented as hazard ratios. The model describes how the hazard of event (suicide attempt) is predicted by the current values of explanatory variables. The population attributable fraction was calculated by comparing the time in major depressive episodes with other phases and using a formula for multicategory exposures (
38). The Statistical Package for Social Sciences software, version 17.0 (SPSS, Inc., Chicago), and an R package (R Development Core Team, Vienna, Va.) were used.
Discussion
During a long-term follow-up evaluation of psychiatric patients with major depressive disorder, three-fourths of suicide attempts took place during major depressive episodes. The incidence rate of attempts was 21-fold during time depressed and fourfold during time in partial remission compared with time in full remission. In addition to time spent in depressive states, previous suicide attempt, age, and perceived social support also independently influenced the risk.
Our study has several strengths. It is a prospective, long-term follow-up assessment of a representative cohort of psychiatric out- and inpatients with major depressive disorder in a medium-to-large Finnish city. We used life chart methodology, which enabled us to investigate the effect of variations in risk and time at risk. We investigated a broad range of risk and protective factors from several domains, including axis I and II comorbid disorders and symptoms, history of suicidal behavior, and temperamental and psychosocial factors in the risk of suicide attempts. Structured and semistructured measures, both objective and subjective, were used. Only 20 subjects (7.4%) dropped out from all follow-up interviews, and the use of Cox proportional hazards model enabled analyses of information on subjects remaining in the study for different lengths of time. Individuals who dropped out did not differ in terms of suicide attempts or suicidal ideation at baseline or before entry.
Nevertheless, some methodological limitations must be noted. First, although we had access to patient records, the 3.5 years between the last two interviews may have affected the accuracy of life charts. We have previously acknowledged that because of a long follow-up period between the last two interviews, we probably slightly underestimated (by approximately 10% overall) the recurrence rate during the time most remote from the 5-year interview after 18 months (
20). Second, similar to any study with retrospective assessment, it is possible that suicide attempts might bias recall of depression. Third, the timing of six suicide attempts (5.7% of the total) was uncertain, and these attempts were excluded from analyses. Fourth, effort after meaning and circularity as a result of diagnostic criteria could in theory affect the timing of when the suicide attempts and when the major depressive episodes were estimated to have happened. However, although patients or the interviewer might have retrospectively automatically attributed suicide attempts to depressive episodes, collateral information on state factors at the time of attempts was also available from psychiatric and medical records. Further, virtually all subjects who attempted suicide also reported suicidal ideation (
11), which alone fulfills the DSM–IV suicidality criterion (A9) for major depressive episodes. Thus, whether or not a suicidal patient attempts suicide is rarely decisive in the fulfillment of criteria for a major depressive episode. Therefore, this diagnostic item is unlikely to tautologically bias the relationship between major depressive episodes and suicide attempts. Fifth, we did not have reliable information on impulsive-aggressive behavior and traits, which might modify risk during major depressive episodes. However, they often correlate with comorbid cluster B personality disorders and alcohol abuse or dependence. In our study, only alcohol dependence or abuse during the follow-up assessment period predicted suicide attempts. Nevertheless, significance of individual frailty in the Cox model suggests that unmeasured trait factors (e.g., impulsivity and aggressivity) may well significantly influence suicide attempts. Sixth, we could only investigate average risk for the time spent in risk states. The risk for suicide attempts likely covaries markedly with variations in levels of hopelessness, depression, and perhaps anxiety, none of which we could measure on a daily basis. Seventh, our statistical models cannot completely distinguish between effects at the population and individual level, meaning that causal inferences at the level of individuals are not warranted. Eighth, the study was naturalistic, and we did not control for treatment. However, treatment could influence the risk for suicide attempts in the following two ways: by reducing the time spent depressed and, possibly, by modifying the risk independently or interacting with the effect on depression. Since our main outcome was the occurrence of suicide attempts per time, treatments that merely reduce the time depressed should not bias incidence estimates, although they reduce the total number of suicide attempts. We believe that our incidence estimates represent realistic and generalizable risk estimates under usual treatment conditions in psychiatric care.
To our knowledge, no previous long-term study has investigated variations in the incidence of suicide attempts during different levels of depression among patients with unipolar major depressive disorder. The incidence rate varied strongly with time, being 20.9-fold during major depressive episodes compared with full remission. This is consistent with findings in our 18-month follow-up assessment (
8) and in the Jorvi Bipolar Study, a comparable study of bipolar disorder (
18). Another medium-term study conducted by Oquendo et al. (
9) reported a sevenfold hazard during depressive episodes, which is similar to our estimate (hazard ratio=7.7). Our incidence rate of suicide attempts during major depressive episodes (0.33 per patient-year) was similar to these earlier estimates (0.30–0.42 per patient-year). In accordance with most prospective studies, the risk was highest during the first year of follow-up evaluation, likely as a result of decline in the time spent depressed after the first follow-up year. However, the incidence rate of suicide attempts during depressive episodes remained constant. Shortcomings in the continuity and provision of acute phase, continuation, and maintenance antidepressant and psychosocial treatments are obvious, both in this cohort (
39,
40) and in other settings (
9), and have been described for patients with major depressive disorder overall as well as for those attempting suicide. Given the importance of high-risk states for overall risk, reducing the time at risk by effective treatments may be crucial for reducing suicide attempts in the long-term.
We also found evidence for other risk and protective factors affecting the likelihood of suicide attempts. In the earlier 18-month follow-up assessment for the Vantaa Depression Study, the risk was effectively predicted by the time spent in major depressive episodes, lack of a partner, and previous attempts (
8). Previous suicide attempt has been consistently associated with elevated risk of a later attempt (
3–
10,
15,
16). Additionally, in the present long-term study, the risk was more than fourfold. Lack of a partner increased risk at a nearly significant difference (hazard ratio=2.32), repeating the findings of our 18-month follow-up assessment. Marriage has been associated with a lower risk of suicide attempts (
3), which could reflect protectiveness toward the family and child-related concerns (
12). A partner is a major factor in objective and perceived social support, which in the present study protected patients from suicide attempts both at baseline (
11) and longitudinally. Contrary to our hypothesis, we did not find comorbid cluster B personality disorders to be significantly related to risk. We detected no significant statistical interactions between high-risk time periods and other risk factors, but this does not exclude the possibility that important risk modifying interactions could exist. However, our findings do strongly emphasize the significance of state and time varying factors in the risk of suicidal acts.
Overall, among patients with major depressive disorder, the incidence rate of suicide attempts varies markedly depending on the level of depression, being highest during major depressive episodes. Although previous attempts and poor social support also indicate risk, the time spent depressed is likely the major factor determining overall long-term risk.