Posttraumatic stress disorder (PTSD) is a chronic and debilitating psychiatric disorder, which occurs at a rate among women (10.4%) nearly double that found among men (5.0%) (
1). PTSD is particularly prevalent among women who have experienced childhood abuse and related interpersonal violence, with rates of the disorder ranging from 26% to 52% (
2–
4). PTSD arising from childhood abuse is particularly pernicious because it is associated with multiple forms of trauma in both childhood and adulthood, including emotional abuse, physical assault, sexual assault, and domestic violence (
5,
6). Individuals with PTSD related to childhood abuse typically experience substantial emotion regulation and interpersonal difficulties, which have been classified in DSM–IV under the associated features of the disorder (
7). Cognitive-behavioral therapies (CBTs), particularly exposure therapy, have been shown to be successful and superior to other types of psychosocial therapies in treating PTSD (
8–
10). However, the use of these therapies to resolve the psychosocial consequences of childhood abuse, while successfully applied among pediatric samples (
9), has been little studied among adults (
8,
11). Given the prevalence of adulthood PTSD related to childhood abuse and the range of psychological problems that afflict this population, research on effective treatment for these patients is important.
As noted by several treatment guidelines, CBTs were designed specifically to resolve PTSD symptoms (
8,
9,
11). They do not include interventions that explicitly address the additional interpersonal and emotion regulation problems observed among those with PTSD stemming from childhood abuse. These problems may occur equally or with greater frequency than PTSD symptoms (
12). Interpersonal and social adjustment problems include difficulties functioning at work, marital and dating problems, parenting problems, social isolation, and low perceptions of social support (
13,
14). Emotion regulation disturbances include easy provocation and high reactivity to emotionally evocative stimuli followed by difficulty calming down (
15,
16). Among the most functionally significant of emotion regulation problems are difficulties with anger management. Anger problems have been rated by patients with PTSD as of significant concern (
17) and have been directly implicated in interpersonal problems (
18).
In addition, despite endorsement by professional guidelines, most clinicians do not regularly use exposure therapy, citing concerns about difficulties patients may have in managing feelings that arise from memory processing and the consequent risk of adverse effects (
19,
20). There are, in fact, very limited and conflicting data regarding concerns that exposure therapy might be associated with high treatment dropout rates (
21,
22), PTSD symptom exacerbation during exposure work (
23,
24), or worsening of PTSD at the end of treatment (
25).
Theoretical models of treatment for chronically traumatized individuals have proposed that the restoration or strengthening of day-to-day life competencies be a prerequisite for the exploration of the past (
26). It has been suggested that this type of preparation might enhance the benefits of confronting and reevaluating the meaning of past traumatic events, while protecting against potential adverse consequences. A phase-based treatment was developed in which a protocol in skills training in affect and interpersonal regulation (STAIR) preceded a standardized exposure therapy. A randomized controlled trial demonstrated the feasibility of the treatment and found that relative to a wait-list, the sequential treatment significantly reduced PTSD, emotion regulation, and interpersonal problems (
22).
The purpose of the present randomized controlled trial was to determine whether the use of skills training preceding exposure would produce outcomes better than those for a treatment in which exposure was implemented without skills training. In addition, we aimed to systematically assess the presence of adverse effects in the treatment of PTSD related to chronic and early-life trauma, particularly in regard to the use of exposure therapy. Skills training followed by exposure (STAIR/Exposure) was compared with Supportive Counseling followed by Exposure (Support/Exposure) and with skills training followed by Supportive Counseling (STAIR/Support), where Supportive Counseling provided an active nonspecific treatment to replace each of the specific treatment modules. The comparison of STAIR/Exposure to Support/Exposure allowed an evaluation of the benefits of adding skills training before exposure, controlling for the duration of the treatment phase, number of sessions, and therapist contact. The comparison of STAIR/Exposure to STAIR/Support, in which exposure (the putative source of adverse effects) was eliminated, provided baseline data regarding adverse effects in a nonexposure treatment with the same controls. It was hypothesized that the Skills/Exposure sequential treatment would be superior to the Support/Exposure treatment in providing greater reductions in PTSD symptoms, emotion regulation, and interpersonal problems.
It was also hypothesized that the sequential treatment would be associated with fewer dropouts, lower PTSD symptoms during exposure work, and less patient worsening relative to Support/Exposure and would not differ from the nonexposure skills treatment. In summary, we evaluated the proposal that the sequential treatment would provide benefits superior to those typically associated with exposure therapy but with the safety and tolerability expected in nonexposure therapy.
Method
Procedure
Participants (N=104) were women, between the ages of 18 and 65 years, who had a primary diagnosis of DSM–IV-defined PTSD related to childhood sexual abuse and/or physical abuse by a caretaker or person in authority over them before the age of 18 years. Exclusion criteria were substance dependence not in remission for at least 3 months, current psychotic symptoms, significant cognitive impairment, untreated bipolar disorder, and acute suicidality in the previous 3 months requiring hospitalization or referral to the emergency room. If candidates were receiving psychotherapy or psychopharmacological treatment, they were allowed to maintain the treatment as long as it had been ongoing for at least 3 months prior to study entry and as long as any psychotherapy was not PTSD-focused. All participants provided informed consent using university-approved consent from the Institutional Review Board. Participants were informed that they would be randomly allocated to one of three treatment conditions (
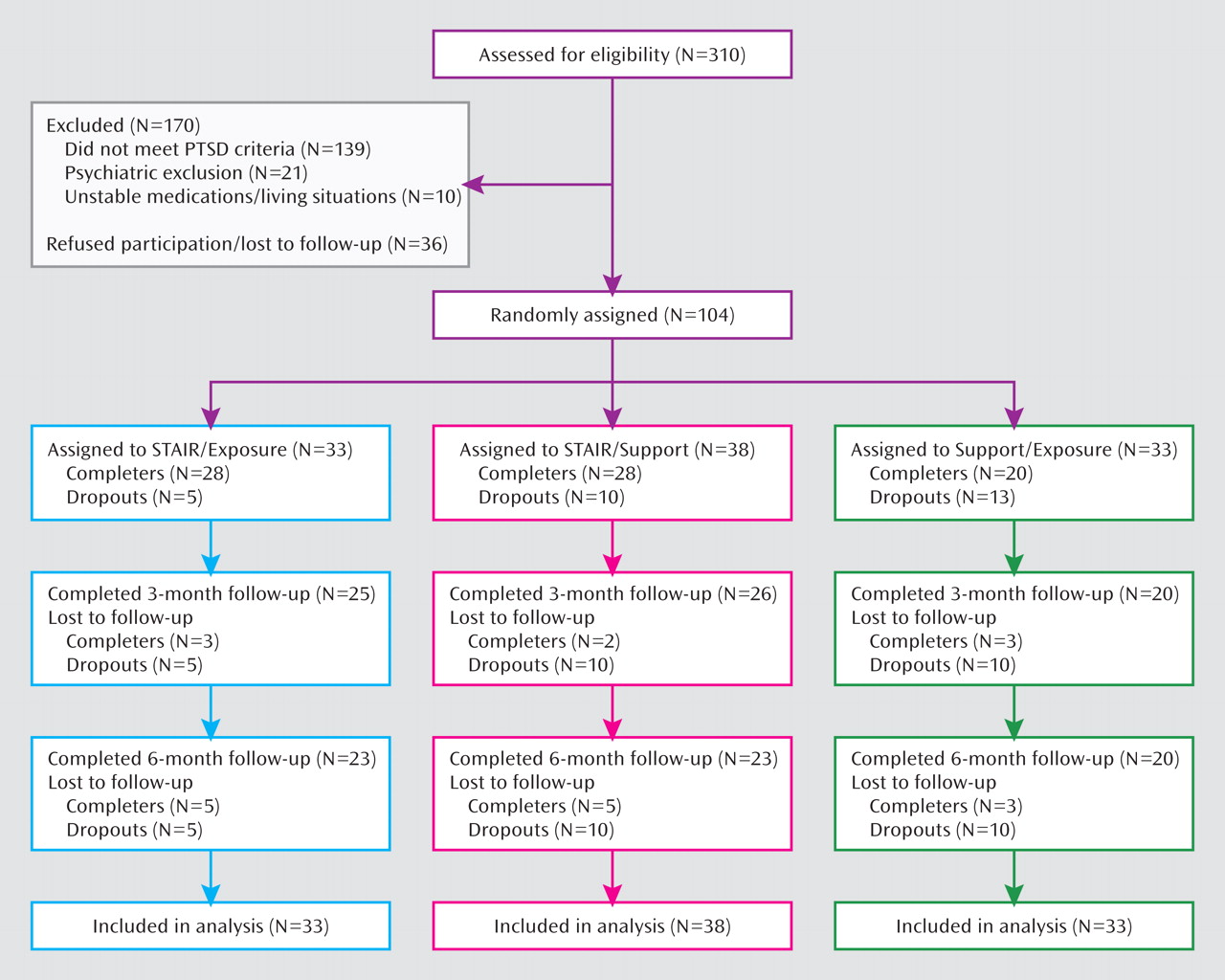
Figure 1). Randomization blocks of nine (three instances of each of the three conditions) were employed, generated by an individual not otherwise involved with the study. Within each randomly assigned condition, the participant was assigned to one of three therapists, based on a match in availability.
Measures
PTSD was diagnosed with the Clinician-Administered PTSD Scale (
27). All other axis I diagnoses as well as axis II diagnoses were assessed using the Structured Clinical Interview for DSM–IV Axis I Disorders (SCID–I) and Structured Clinical Interview for DSM–III–R Personality Disorders (SCID–II), respectively (
28). The Clinician-Administered PTSD Scale and SCID–I were implemented at pre-, post- and follow-up assessments. SCID–II was implemented at pretreatment only. Diagnostic assessments were conducted by independent raters who were blind to treatment condition. Self-report of PTSD symptoms was obtained using the PTSD Symptom Scale–Self Report (
29); emotion regulation was assessed using the General Expectancy for Negative Mood Regulation Scale (
30); and interpersonal problems were assessed with the Inventory of Interpersonal Problems (
31). Secondary outcomes were depression, assessed with the Beck Depression Inventory (BDI) (
32); anxious state, assessed with the State-Trait Anxiety Inventory–S (
33); anger modulation, assessed with the State-Trait Anger Expression Inventory (
34); and perceptions of social support, assessed with the Interpersonal Support Evaluation List (
35).
Treatment Conditions
The therapy was conducted by one of nine female master's degree-level or doctorate-level clinical psychologists or social work staff who were manual trained and received weekly supervision by the first author (Dr. Cloitre) or expert clinicians trained by the first author (Dr. Stovall-McClough, Ms. Cherry). All therapists provided each type of treatment.
STAIR/Exposure
STAIR/Exposure is a weekly 16-session treatment, with eight sessions for skills training and eight for exposure. The skills training interventions are adapted from dialectical behavior therapy (
36). The first four skills sessions concern emotion regulation and focus on identifying and labeling feelings, emotion management, distress tolerance, and acceptance of feelings and experiencing positive emotions. The next four sessions concern interpersonal problems and focus on exploration and revision of maladaptive schemas, effective assertiveness, awareness of social context, and flexibility in interpersonal expectations and behaviors. In this study, the exposure treatment followed the prolonged exposure protocol (
9), with the following two modifications for the study population: 1) in vivo exposure to trauma stimuli was replaced with interpersonal skills practice, and 2) meaning analysis was introduced after the exposure in which abuse-related schemas embedded in the trauma narrative were identified and evaluated. Exposure included narratives of both childhood and adulthood traumas, reviewed in order of distress rating and importance to the participant.
The supportive counseling component in the STAIR/Support and Support/Exposure conditions comprised client-directed discussion of life problems related to abuse history. Skills training and discussion of trauma memories were excluded.
Adherence and competency monitoring
Ten percent of all treatment sessions (N=122) were randomly selected and rated by graduate-level research assistants trained to an adherence protocol (by Dr. Cloitre). Each tape was rated by one of three teams of two raters. Discrepancies were resolved by introducing a third rater from one of the other teams. Adherence was excellent, with 92% of the elements delivered. Competence (1=unacceptable to 4=excellent) was also high, with an average rating of 3.14 (SD=0.55). There were no differences in adherence or competency ratings across the three treatment conditions. No proscribed activities (i.e., no skills training or exposure) were identified in the supportive therapy component of either control conditions.
Statistical Analyses
Analyses for all symptom outcome measures were performed on the intent-to-treat sample using data from all participants according to their randomization assignment. Missing data were imputed using PROC MI in SAS (SAS Institute, Cary, N.C.) to generate 10 imputed data sets. Continuous outcomes were analyzed using longitudinal mixed-effects models, adjusting for baseline. Of interest were 1) main effect of treatment and 2) the interaction between treatment and time, indicating differing effects of time after the end of treatment, depending on the treatment condition. Significance of the main effect for treatment and the interaction term was judged at an alpha level of 0.05 (two-sided). Following a significant omnibus test for the main treatment effect or interaction with time, contrasts between treatment conditions or at different posttreatment times were estimated. Effect sizes within and between groups were reported as the standardized difference of the means at each time point (Cohen's d [
37]).The standardization was based on the pooled standard deviation of the three treatment conditions at baseline. Categorical outcomes were defined for all randomly assigned subjects and the status of subjects with missing observations determined based on their last available value. Logistic regression and likelihood ratio tests were used to assess the significance of between-treatment differences.
Results
Participant Characteristics
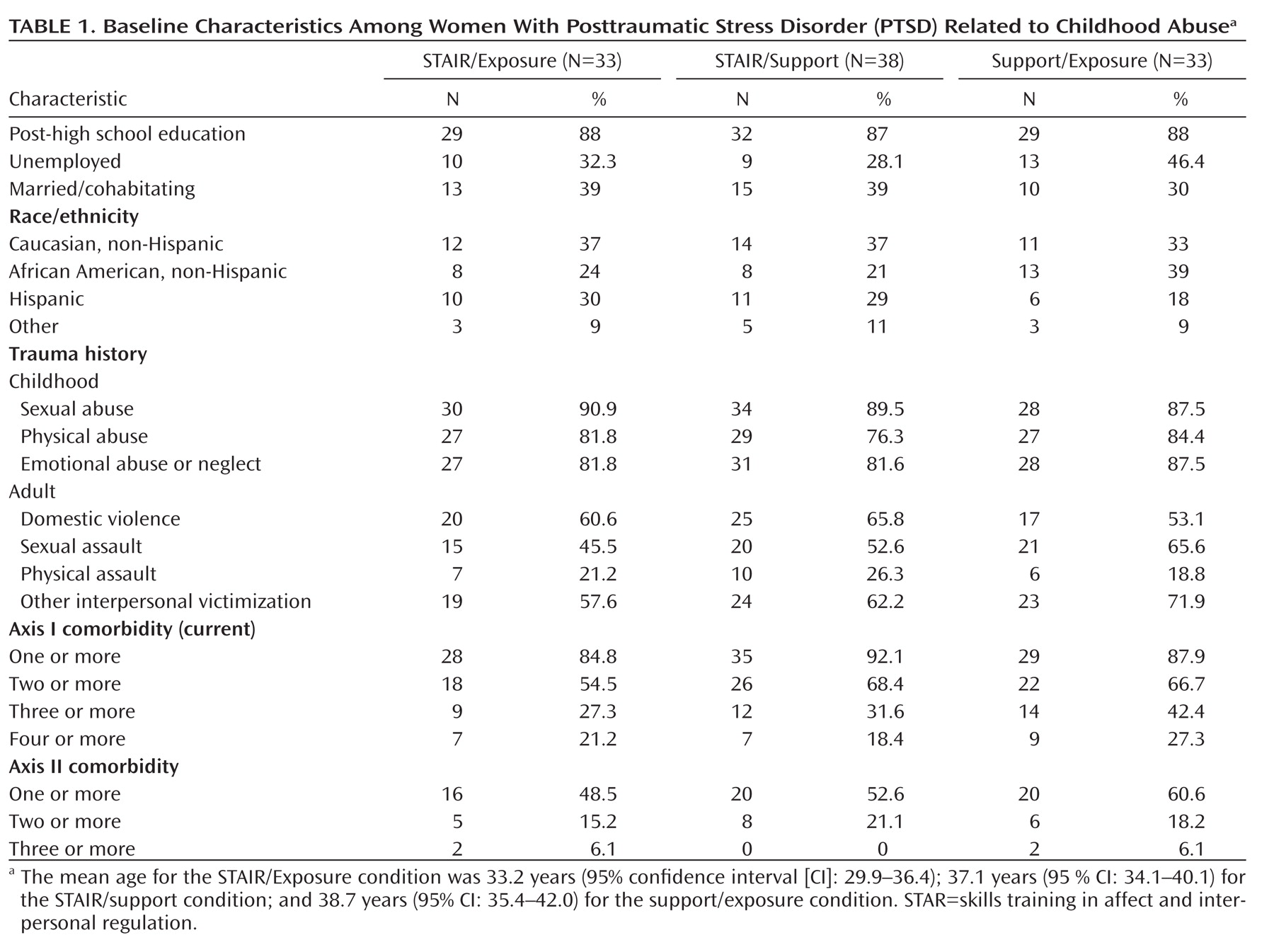
Participants randomly assigned to the three conditions did not differ at baseline with respect to demographic, diagnostic, and clinical characteristics (
Table 1). The average number of lifetime traumas was 6.57 (SD=1.17). The majority of participants met criteria for at least two axis I disorders other than PTSD (average=2.4), and approximately one-half of all participants met criteria for at least one axis II disorder (average=1.1). The most common axis II disorders were avoidant (32%), paranoid (25%), and borderline personality (24%) disorders.
Efficacy
PTSD diagnostic status and symptom severity. Posttreatment diagnostic status did not differ among groups (χ2=1.58, df=2, p=0.11), with a substantial proportion of participants being PTSD-negative in each treatment condition (STAIR/Exposure: N=61%, STAIR/Support: N=47%, Support/Exposure: N=33%). Full remission (defined as a Clinician-Administered PTSD Scale score <20 [27]) at posttreatment was achieved by 27% of STAIR/Exposure participants, 24% of STAIR/Support participants, and 6% of Support/Exposure participants (χ2=6.46, df=2, p=0.04). Pairwise analyses indicated that the remission rate was significantly higher for individuals in the STAIR/Exposure condition than the Support/Exposure condition (χ2=4.37, df=1, p=0.04; odd ratio=5.67, 95% confidence interval [CI]=1.11–28.81).
Persistence of PTSD status at follow-up evaluation was assessed by identifying the proportion of individuals who maintained their status through the 3-month and 6-months assessments. Persistence of PTSD-negative status significantly differed, with 55% of STAIR/Exposure participants, 37% of STAIR/Support participants, and 21% of Support/Exposure participants reaching the criterion (χ2=7.22, df=2, p=0.03). The likelihood of maintaining PTSD-negative status was greater for individuals in the STAIR/Exposure condition than the Support/Exposure condition (χ2=6.72, df=1, p=0.01; odds ratio=4.23, 95% CI=1.42–12.59). The rate of sustained PTSD full remission differed among the three groups (STAIR/Exposure: N=24%, STAIR/Support: N=13%, Support/Exposure: N=0% [χ2=12.56, df=2, p=0.002]), and follow-up pairwise comparisons indicated that the likelihood of maintaining PTSD remission in the STAIR/Exposure condition was greater than in the Support/Exposure condition (odds ratio >10, p<0.001).
Supplemental analyses of the Clinician-Administered PTSD Scale ratings measured continuously were conducted. A mixed-effects model revealed a time-by-treatment interaction (p=0.01), where pairwise between-treatment comparisons indicated that the STAIR/Exposure condition produced lower scores than the Support/Exposure condition at the 3-month follow-up evaluation (Cohen's d=0.76, p<0.001). No other contrasts were significant (
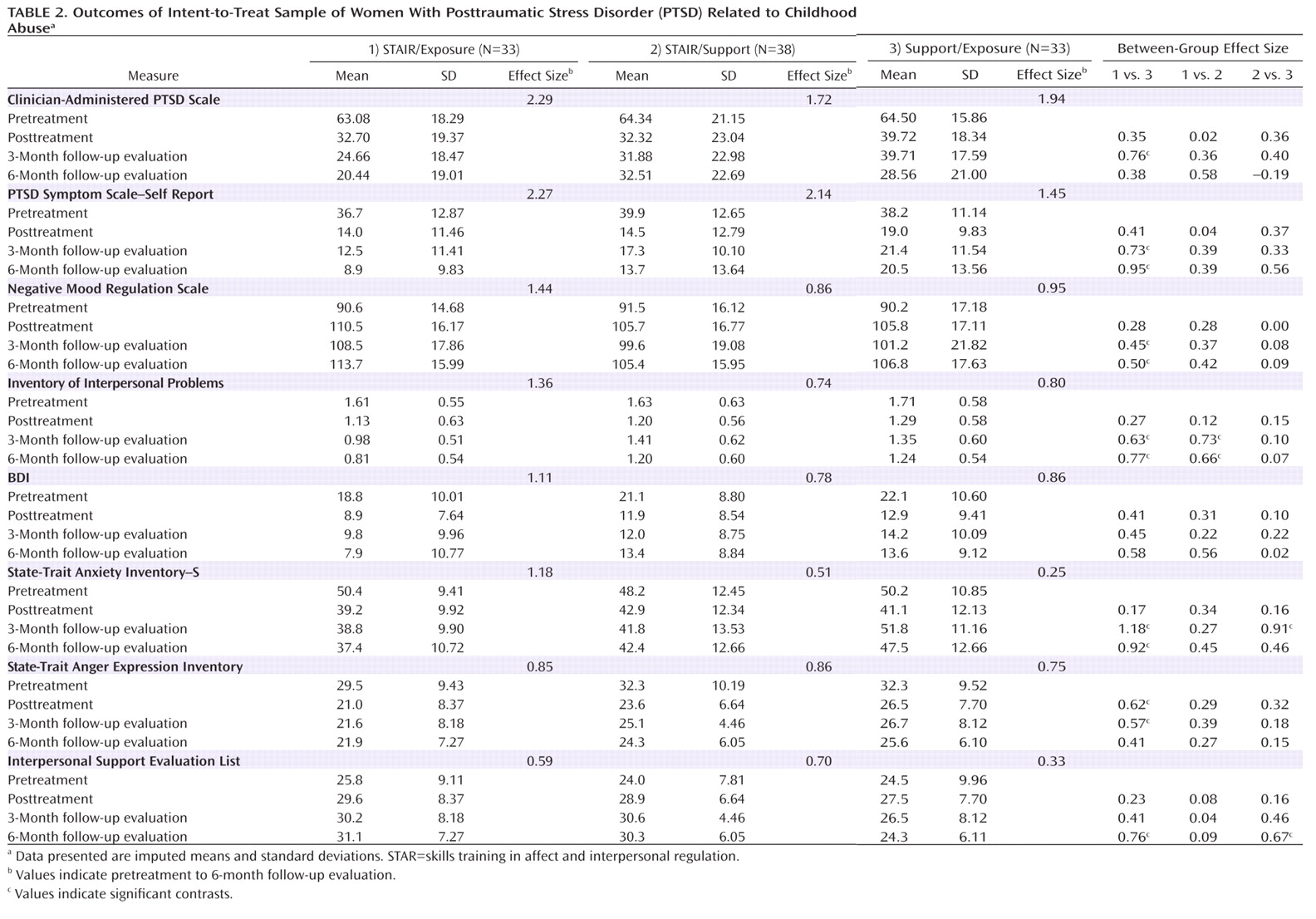
Table 2).
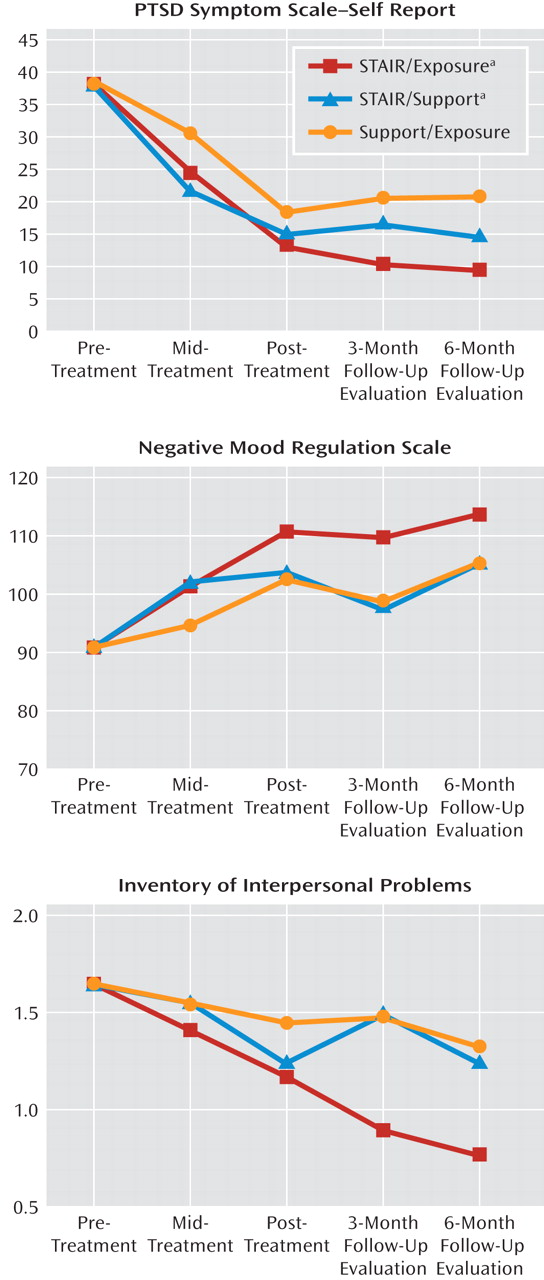
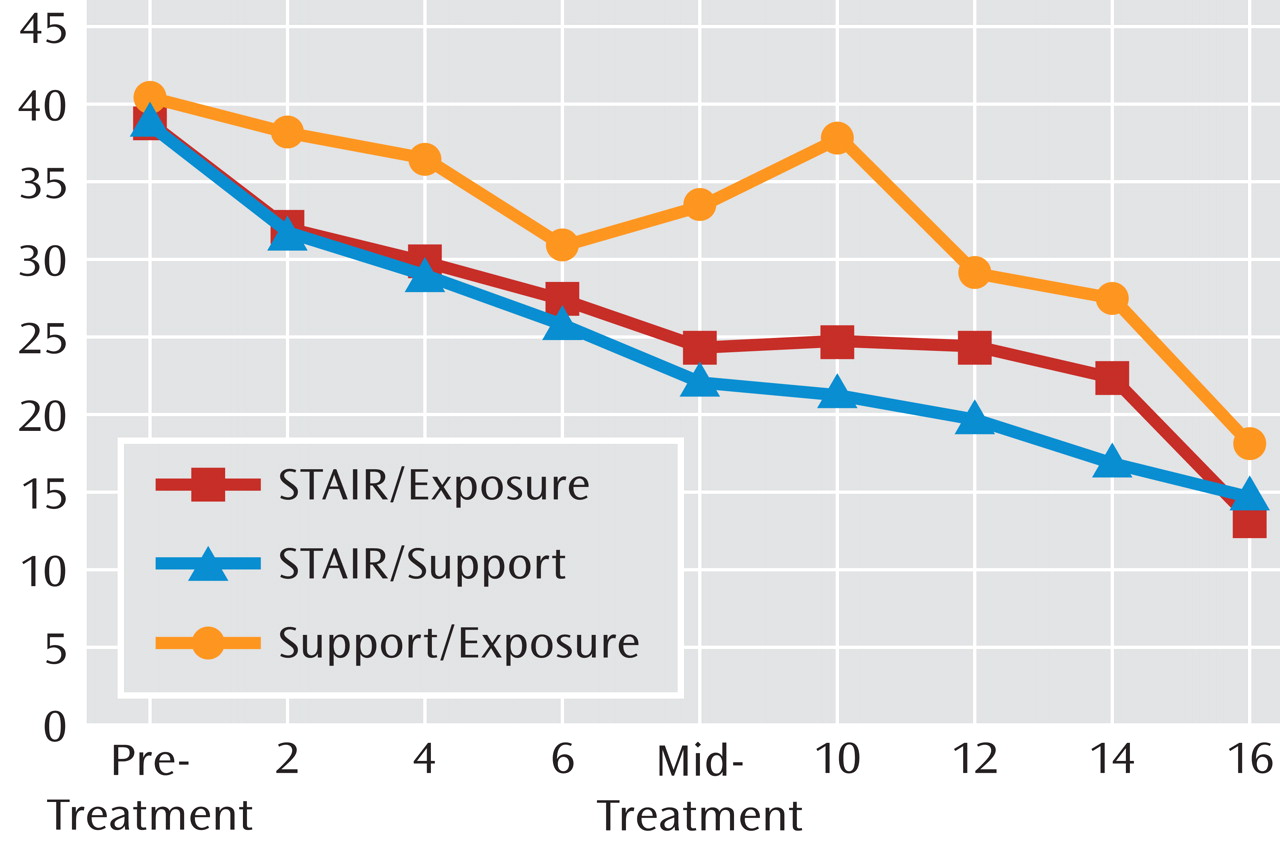
Primary outcomes
Figure 2 depicts observed mean scores across all time points, for which data were collected for the primary outcomes of self-reported PTSD symptoms, negative mood regulation, and interpersonal problems. Table 2 presents the imputed means and standard deviations as well as within- and between-treatment effect sizes.
A main effect (p=0.007) and interaction effect were obtained (p=0.03) for self-reported PTSD symptoms. The STAIR/Exposure condition produced significantly lower PTSD Symptom Scale–Self Report scores at the 3-month (Cohen's d=0.73, p<0.001) and 6-month (Cohen's d=0.95, p<0.001) follow-up assessments. Across time, participants in the STAIR/Exposure condition showed reductions in scores from posttreatment to the 6-month follow-up assessment (Cohen's d=0.34, p<0.001), while no changes were observed following immediate posttreatment in the other two conditions. For negative mood regulation, a marginally significant interaction effect was obtained (p=0.08). Given the a priori interest in specific comparisons and in order to estimate the magnitude of the effects, planned contrasts were undertaken. The STAIR/Exposure and Support/Exposure groups did not differ at immediate posttreatment, but STAIR/Exposure participants produced higher negative mood regulation scores than Support/Exposure participants at the 3-month (Cohen's d=0.45, p=0.05) and 6-month (Cohen's d=0.50, p=0.04) follow-up assessments. No other comparisons were significant.
For interpersonal problems, an interaction effect was obtained (p=0.004). Pairwise contrasts indicated that the STAIR/Exposure and Support/Exposure groups did not differ at posttreatment, but STAIR/Exposure participants produced significantly lower scores at the 3-month (Cohens' d=0.63, p=0.01) and 6-month (Cohen's d=0.77, p=0.003) follow-up assessments. The STAIR/Exposure condition was also superior to the STAIR/Support condition at the 3-month (Cohens' d=0.73, p=0.005) and 6-month (Cohens' d=0.66, p=0.01) follow-up assessments. STAIR/Exposure participants showed improvement from posttreatment to the 6-month follow-up evaluation (Cohen's d=0.34, p<0.001); STAIR/Support participants showed a significant deterioration from posttreatment to the 3-month follow-up evaluation (Cohen's d=0.46, p=0.02); and Support/Exposure participants showed no change.
Secondary outcomes
All participants showed improvement on all measures. No treatment or interaction effect was obtained for depression (BDI score). Regarding state anxiety, an interaction was obtained (p=0.003), with the STAIR/Exposure condition resulting in greater improvement than the Support/Exposure condition at the 3-month (Cohen's d=1.18, p<0.001) and 6-month (Cohen's d=0.92, p<0.003) follow-up assessments. There was a main treatment effect for anger expression (p=0.03), with STAIR/Exposure participants having significantly greater improvement than Support/Exposure participants (Cohen's d=0.45, p=0.02), and this relationship remained the same at all time points (i.e., no time-by-treatment interaction). There was an interaction effect for social support (p=0.05), with the STAIR/Exposure group providing greater improvement in perceived social support at 6 months than the Support/Exposure group (Cohen's d=0.76, p=0.01), as did the STAIR/support group (Cohen's d=0.67, p=0.01) (Table 2).
Adverse Effects
Treatment dropout
The percent of participants who dropped out of treatment differed by treatment condition (χ
2=4.94, df=2, p=0.04), with 15.2% of participants dropping out of the STAIR/Exposure group, 26.3% dropping out of the STAIR/Support group, and 39.4% dropping out of the Support/Exposure group. Pairwise comparisons indicated that the dropout rate for the STAIR/Exposure condition was significantly lower than that for the Support/Exposure condition (χ
2=4.89, df=1, p=0.03). The number of dropouts in both phase 1 and phase 2 of treatment was lowest in the STAIR/Exposure condition (
4,
1), highest in the Support/Exposure condition (
9,
4), and fell in the middle in the STAIR/Support condition (
7,
3).
PTSD symptoms during exposure
PTSD symptoms for the previous week, measured by the PTSD Symptom Scale–Self Report severity scores, were obtained at the end of every other session (see
Figure 3 for observed means across sessions). Phase 2 scores were compared between conditions for the treatment completers (N=76), using mixed-effects analyses. As hypothesized, the mean PTSD symptom severity in the exposure component of the STAIR/Exposure condition was significantly lower than that of the Support/Exposure (p=0.05). In addition, the PTSD score in the exposure component of the STAIR/Exposure condition was higher than but did not differ from that obtained in the parallel (nonexposure) supportive counseling component of the STAIR/Support condition (p=0.22).
Symptom worsening
To measure reliable, clinically meaningful deterioration, we followed the criteria by Devilly and Foa (
25) and defined worsening as when a participant had a posttreatment Clinician-Administered PTSD Scale score exceeding her baseline score by at least one standard deviation of the difference of two repeated administrations. Given a Clinician-Administered PTSD Scale test-retest reliability with an alpha of 0.92 (
27) and standard deviation of the severity score in a nonpsychiatric sample of 16.6 (
38), worsening was equal to 6.6 points. Participant symptom worsening was defined as a total severity score of 7 points or more compared with baseline. At posttreatment, relative to pretreatment, one participant (3.6%) in the STAIR/Exposure group, three participants (7.4%) in the STAIR/Support group, and five participants (15%) in the Support/Exposure group showed symptom worsening, but these differences were not statistically significant. From posttreatment to the 6-month follow-up evaluation, no additional participants showed worsening in the STAIR/Exposure condition, while an additional five participants (22.7%) in the STAIR/Support condition and five (31.3%) in the Support/Exposure condition showed worsening. The STAIR/Exposure condition was superior to both the STAIR/Support (Fisher's exact test, p=0.02) and Support/Exposure (Fisher's exact test, p=0.006) conditions.
Discussion
The present study demonstrates that among women with early-life and chronic traumatization, a phase-based treatment in which skills training preceded exposure provided superior benefits and fewer adverse effects than an exposure treatment without skills and no greater or fewer adverse effects than a nonexposure skills condition. STAIR/Exposure treatment was more efficacious than Support/Exposure in attaining persistent remission of PTSD and persistent PTSD-free diagnostic status. It also provided greater benefit in reducing problems in emotion regulation, anger expression, and anxiety. The STAIR/Exposure condition was superior to both other conditions in improving interpersonal problems. Assessment of adverse effects revealed that 1) the STAIR/Exposure dropout rate was lower than that for Support/Exposure and equivalent to STAIR/Support, 2) symptom exacerbation in the STAIR/Exposure condition during phase 2 was lower than that for phase 2 of the Support/Exposure condition and did not differ from phase 2 of the STAIR/Support condition, and 3) posttreatment symptom worsening was negligible and significantly less than that observed in either control condition.
Consistent with recent reports of exposure therapy (
39), the Support/Exposure condition produced maximum benefit at immediate posttreatment, with little change during follow-up evaluation. The superior benefits of STAIR/Exposure emerged primarily at the 3- and 6-month follow-up assessments. We speculate that continuing improvement after therapy ends may result from the cumulative and complementary benefits of each treatment component. Since patients confront day-to-day challenges in interpersonal and other life stressors, successful exposure therapy may make them less likely to react to events such as "traumatic reminders," while skills training may provide strategies that help address the situation in a realistic and effective way.
The relative advantage of the sequential treatment for negative mood regulation was only marginally statistically significant but, nevertheless, clinically meaningful. In addition, STAIR/Exposure was associated with statistically and clinically greater improvement in anger expression, a problem that has substantial negative effect in the lives of individuals with PTSD. Taken together, these results suggest an overall added benefit associated with STAIR/Exposure regarding emotion regulation difficulties.
The 39% dropout rate in the Support/Exposure condition is similar to that found in previous controlled studies of well-delivered exposure therapy among women with childhood abuse PTSD (41%) (
21) as well as among those with multiple, primarily interpersonal trauma (38%) (
39), while the 15% dropout rate obtained for the STAIR/Exposure condition is at the lower end of rates found in treatment trials across all PTSD populations (
8). The dropout rate was numerically lower in both phases of treatment in the STAIR/Exposure condition relative to the Support/Exposure condition. Initiating treatment with skills training may enhance patient engagement because it responds to the day-to-day problems for which the patient frequently comes to treatment. Reduction in PTSD symptom exacerbation during exposure may also contribute to lower attrition, although the relationship between symptom exacerbation and treatment dropout has not been demonstrated (
24). Regardless of this debate, the reduction in exposure-related symptom exacerbation among STAIR/Exposure completers when paired with superior outcome can be viewed as an improvement in the quality of the treatment and may increase patient and therapist willingness to use exposure-based interventions for PTSD.
Symptom worsening at immediate posttreatment did not differ across the three conditions and did not differ between the STAIR/Support and Support/Exposure groups at the follow-up assessments. Thus, the concern that an exposure-focused therapy results in symptom worsening that exceeds what might be found in a nonexposure therapy was not supported. However, by the 6-month follow-up evaluation, both control conditions were associated with symptom worsening relative to the STAIR/Exposure condition, in which there were no further cases of treatment worsening, suggesting that the therapy provides prophylaxis against posttreatment symptom deterioration.
Some cautions regarding the interpretation of the results are required. First, three previous investigations using the combination of stress management skills training and exposure found that the combination was not superior to either intervention alone (
9). Our findings differ. This may be because of the sequencing of components that gives focused time and attention to each type of intervention or to differences in the type of skills training employed. The dialectical behavior therapy-type skills taught in this treatment may more effectively target the particular difficulties of this patient population relative to the general relaxation or stress reduction techniques used in previous studies. Second, the findings of the Support/Exposure condition may not be representative of exposure therapy as typically practiced, where exposure is rapidly implemented (usually in the second or third session). Supportive Counseling may have contributed to good outcome, since the pre- to posttreatment effect size for the Clinician-Administered PTSD Scale scores in the Support/Exposure condition (1.45) is larger than that for an exposure only treatment (0.71) in a previous childhood abuse PTSD trial (
21). Lastly, while the STAIR component of the treatment has never been tested on its own, the observed benefits associated with STAIR/Support, which were lower than the sequential treatment but often similar to the exposure treatment, suggest that nonexposure skills-focused treatments might warrant investigation.
To date, of the 40 randomized controlled trials conducted regarding PTSD, only four have concerned those with PTSD related to childhood abuse (
40). Our study contributes to the PTSD treatment literature by testing a hybrid treatment that increases treatment options for this population. This phased-based treatment is efficacious in resolving several symptom domains, in reducing dropout rates and in providing protection against posttreatment deterioration.