Prevention represents the Holy Grail for mental disorders, as in other areas of medicine. However, prevention trials are notoriously difficult to design and conduct because of the long time frames involved and the difficulty of reliably identifying malleable risk factors. This is particularly true for studies of young children, in which rapidly changing developmental status, marked heterogeneity of environmental factors, and difficulty in identifying intervention targets all confound study designs. In this issue, Rapee et al. (
1) report the extended follow-up of a selective intervention that yielded promising initial results (
2). The study is notable for the early age at which children were selected (a mean age of less than 4 years), the brief nature of the intervention, and the sustained positive outcome over a 3-year follow-up period.
In brief, children were selected for the study on the basis of having both a high withdrawal score on a subscale of the Childhood Temperament Questionnaire and high scores on a laboratory test of behavioral inhibition. The intervention consisted of six 90-minute sessions conducted by child clinical psychologists with groups of approximately six sets of parents. Intervention elements included a general introduction to developmental aspects of anxiety, principles of parenting techniques (notably instruction on the importance of parental over-protection as a risk factor for child anxiety), cognitive restructuring for parents' worries about the child (and also for the children as they matured), application of exposure hierarchies for the child, and the importance of continued application of the techniques, particularly during high-risk periods, such as starting school. A control group was simply monitored on the same schedule as the experimental group, with assessments in the clinic every 12 months.
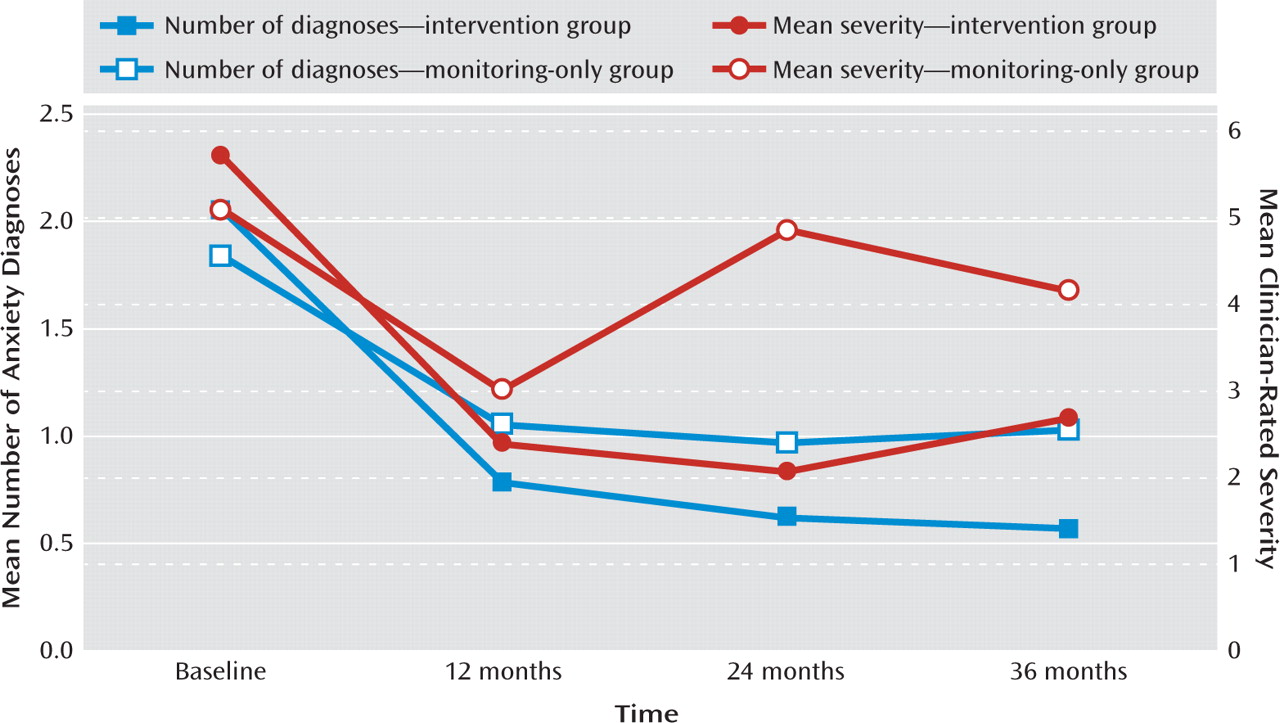
The primary outcome measures were number and severity of diagnosed anxiety disorders, with assessments from baseline through three annual follow-up visits (
Figure 1). The overall number of disorders, as well as their severity, decreased for both groups in the years following study initiation. The notable result, however, was that children in the intervention group showed significantly fewer anxiety disorders and lower symptom severity at the last two follow-ups compared with the control group. Maternal ratings of the children's anxiety also showed lower levels at the 3-year follow-up, with a similar trend for children's self-report of anxiety at 3 years.
This is a remarkable result, particularly given the relatively brief intervention and the lack of any “booster” sessions after the initial parental sessions. Moreover, the intervention was delivered entirely through the parents, with no direct contact between clinicians and children. There are, of course, some limitations of the study that temper its promising conclusions. First, the study used a convenience sample that was not entirely representative; the ethnic makeup was almost exclusively European, and over 50% of the parents had a university education. Since the intervention is entirely dependent on the parents' ability to grasp the sessions' content and their ability to change and sustain their behavior toward their children, effects might be diminished for parents with a lower average education level. The authors also do not report any gender differences, which would be of interest given the well-known higher risk of internalizing disorders for girls.
An intriguing observation was that the treatment effects were relatively modest at 1 year but more robust at 2 and 3 years—the reverse of the usual pattern for extended follow-ups. Also, the mean illness severity differences appear to be due largely to an exacerbation of symptoms in the control group, inviting a replication to ensure that this result is reliable. It is possible, as the authors speculate, that this pattern indicates an adverse trajectory of development in the untreated children. It would be of great interest to know whether this outcome stemmed from a large exacerbation in a relatively small number of children in this group—which would suggest a disjunctive outcome in which a minority experienced an adverse course. Identifying particular risk factors for such a cohort could further enhance prevention efforts.
One particularly interesting aspect of the findings was that measures of inhibited temperament diminished for both groups across the study but failed to show interactions across time, as was seen in the anxiety measures. Several aspects of this result deserve comment. First, it is not surprising that the average trend for children in both groups was in the direction of fewer anxiety disorders overall and reductions in parental reports of the child's inhibitory behaviors. Decades of research have shown a perceptible but modest stability in inhibitory temperament, with many children (presumably because of varying combinations of environmental supports and developmental changes) showing diminished inhibitory behavior over time (
3); children selected for inhibited temperament or familial risk do not necessarily progress to overt disorders, an outcome that often affects only a minority of the high-risk group (
4). Second, the data are nonetheless consistent with other recent studies showing that behavioral inhibition acts as a substantial risk factor for the subsequent development of anxiety and other internalizing disorders (
5). This is true whether the children are identified as offspring of adult patients or through prospective developmental projects (
6,
7). The results of Rapee and colleagues' study illustrate the progress that has been made over the past two decades in identifying malleable risk factors for these effects, such as reducing parental overprotective behavior, helping children gradually adapt to anxiogenic situations, and devising feasible interventions to address such risk factors. Third, it is now clear that early internalizing temperament represents a risk factor for early incidence of disorders that can persist throughout the lifespan; epidemiological data show that most adults report the onset of such disorders by the age of 14 (
8), and social anxiety disorder in adolescents and young adults is well known as a risk factor for major depressive episode (
9). This only adds to the import of Rapee and colleagues' findings.
Finally, recent years have seen considerable evolution in our thinking about the relationships between temperament and mental disorders. In an influential 2005 paper, Clark (
10) discussed temperament as the foundation for both personality and psychopathology (both axis I and axis II); in contrast to other recent models of psychopathology, she wrote, “personality and psychopathology are linked primarily through their shared underlying genetic diatheses of broad temperament dimensions” (p. 511). It is now apparent that the same brain motivational systems that function as the foundation for temperament are also implicated in various aspects of internalizing and externalizing disorders; this fact renders tenuous any distinctions based purely on symptom course or persistence, or differences between axis I and axis II disorders. One consequence of this shift has been a series of proposals in the DSM-5 developmental process to recast personality disorders into a dimensional framework and to distribute the disorders so as to align them with axis I disorders that represent the corresponding neural circuitry (e.g., avoidant personality disorder with the fear circuit disorders). While these proposals have prompted considerable debate (
11), it appears likely that the multiple areas of alignment that have been demonstrated between temperament factors and common mental disorders—as exemplified in the Rapee et al. study—will receive increasing attention with respect to both classification efforts (
12) and new interventions.
The article by Rapee et al. opens up promising new avenues for prevention that can forestall adverse trajectories starting at a very young age. The intervention appears to be amenable to delivery by a wide variety of therapists in multiple settings, including school and community. As the authors remark, “Whether these promising findings will translate to continued protection from anxiety later in the developmental trajectory and whether they can generalize to protection from related disorders remain exciting possibilities” (
1).