Clozapine-Induced Lymphocytic Alveolitis
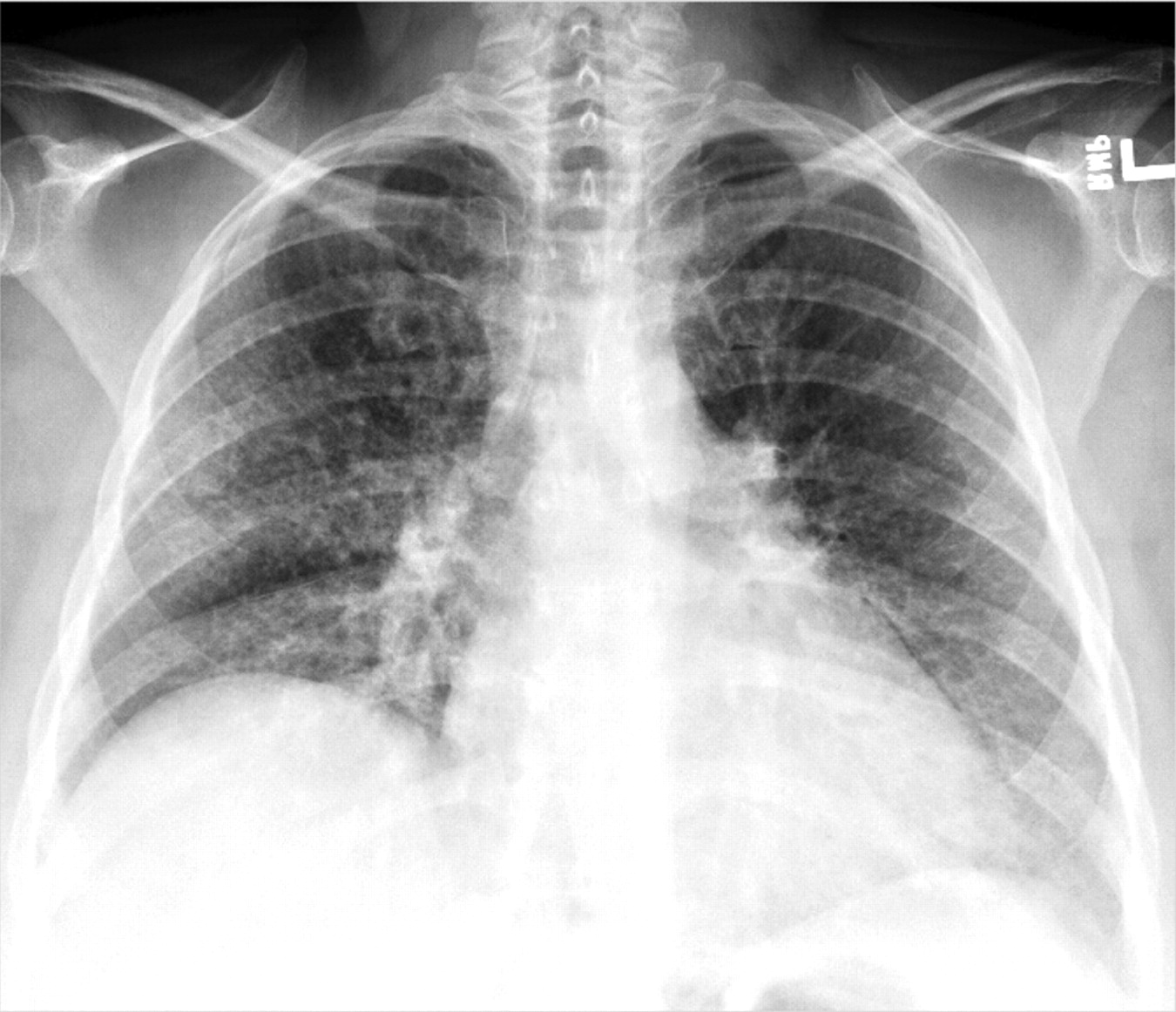
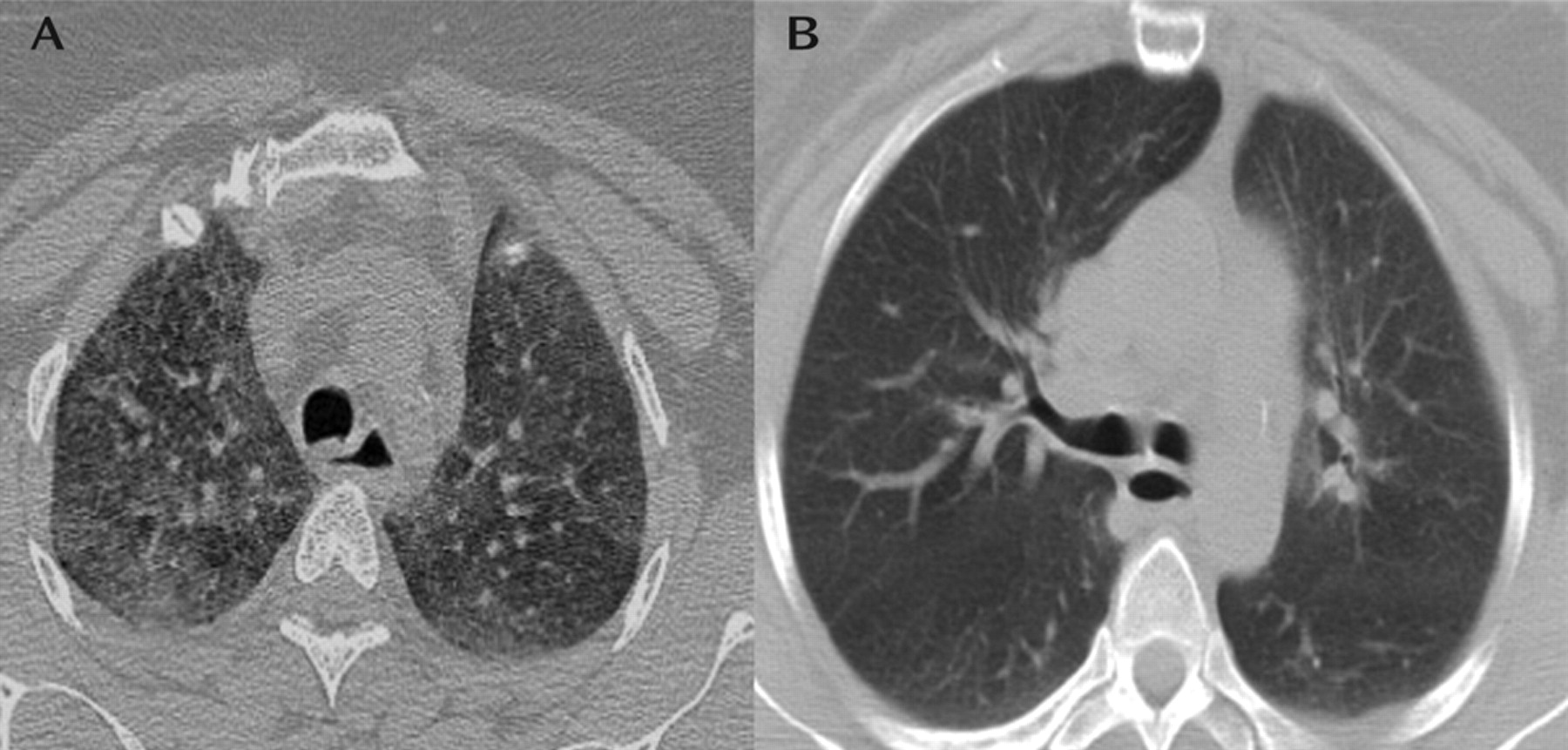
“Mrs. A” was a 41-year-old, Hispanic woman with a history of schizoaffective disorder who was transferred from the psychiatric ward to medical service for evaluation of pulmonary infiltrates. Chest x-ray (Figure 1) and chest computerized tomography (CT) showed diffuse bilateral ground-glass opacities (Figure 2). The patient complained of only mild dyspnea and was able to ambulate without difficulty. She had no cough, chest pain, fever, or chills. She denied any sick contacts or environmental exposures and had stopped smoking several months prior. Her physical examination was unremarkable, and oxygen saturation on room air was 95%.
The patient had a medical history of diabetes, hypertension, and hypothyroidism. Her medications included clozapine, oxcarbazepine, atorvastatin, metformin, and levothyroxine. Two months prior, she had an episode of refractory psychosis and was initiated on clozapine and titrated to a dose of 650 mg/day.
Laboratory data revealed thrombocytosis (689 × 103/μl), elevated liver function (aspartate transaminase level: 75 U/l; alanine transaminase level: 103 U/l), and an increased erythrocyte sedimentation rate (130 mm per hour). There was no peripheral eosinophilia. Rheumatologic serologies and urine toxicology findings were negative, and echocardiogram results were normal. The patient was unable to provide reliable pulmonary function data.
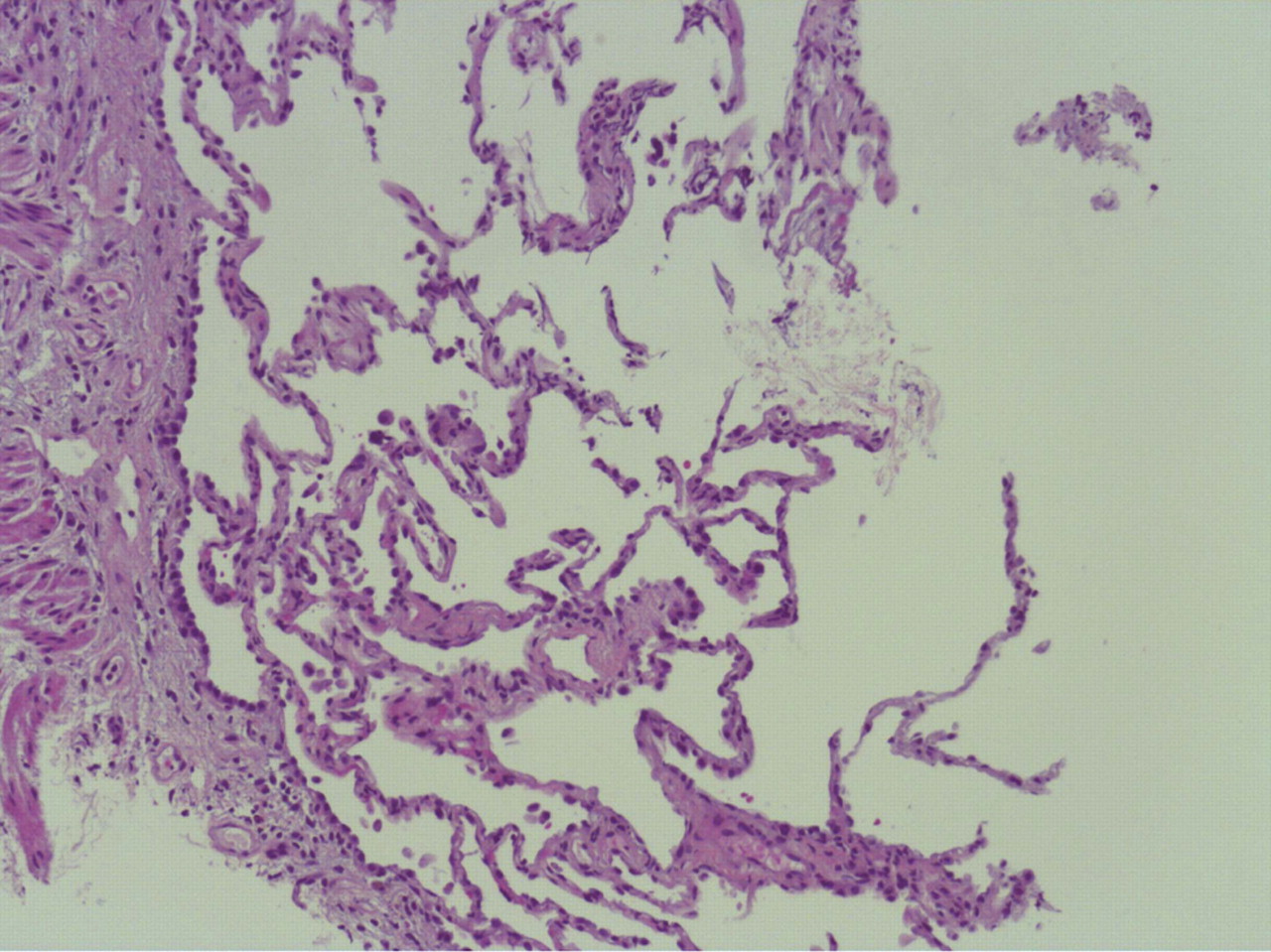
Bronchoalveolar lavage and lung biopsies were performed. Bronchoalveolar lavage showed a predominance of lymphocytes at 54% and eosinophils at 2%. Flow cytometry demonstrated a cluster of differentiation (CD)4/CD8 cell ratio of 0.7. Viral, bacterial, and mycobacterial cultures were negative. Lung biopsies revealed mild chronic inflammation without granulomas (Figure 3).
As a result of the temporal relationship between the initiation of clozapine and abnormal pulmonary findings and the absence of alternative diagnoses, a presumptive diagnosis of clozapine-induced pulmonary toxicity (lymphocytic alveolitis) was made. Clozapine was tapered and discontinued. There were no other changes made to the patient's medication regimen, and she did not receive antibiotics. Two months after discontinuation of clozapine, a repeat chest CT confirmed resolution of infiltrates (Figure 2).
Footnote
References
Information & Authors
Information
Published In
History
Authors
Funding Information
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBLogin options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).

