The best hope for secondary prevention of the often devastating course of psychotic disorders resides in early detection and intervention when individuals first develop symptoms. There is sufficient evidence for attenuated psychosis syndrome as a clinical syndrome with predictive validity to establish this diagnostic class. There is much that clinicians can and should do for care-seeking individuals with distress and dysfunction who manifest early psychotic-like psychopathology. A new DSM-5 diagnosis can focus attention on this syndrome and stimulate the creative acquisition of new knowledge that may be life altering for afflicted persons. There is little reason to rely on less specific diagnostic categories, such as anxiety and depression, if we can reliably give patients and their families a more informative picture of their situation.
—William T. Carpenter
The best hope for early intervention in psychotic disorders resides in public health measures for the population as a whole rather than in attempts to diagnose risk in individuals for what will be a low incidence of future psychosis. Making services more accessible, providing general diagnostic training to primary care workers, and creating community awareness will make the filters on the pathway to mental health treatment more permeable for people with early psychotic symptoms in need of care. Individual treatment should be initiated early but when it is indicated, as when criteria are first met for psychotic disorder not otherwise specified. Creating a diagnostic class that does not unambiguously define a specific group, treatment, or outcome does not add value for patients and their families.
—Jim van Os
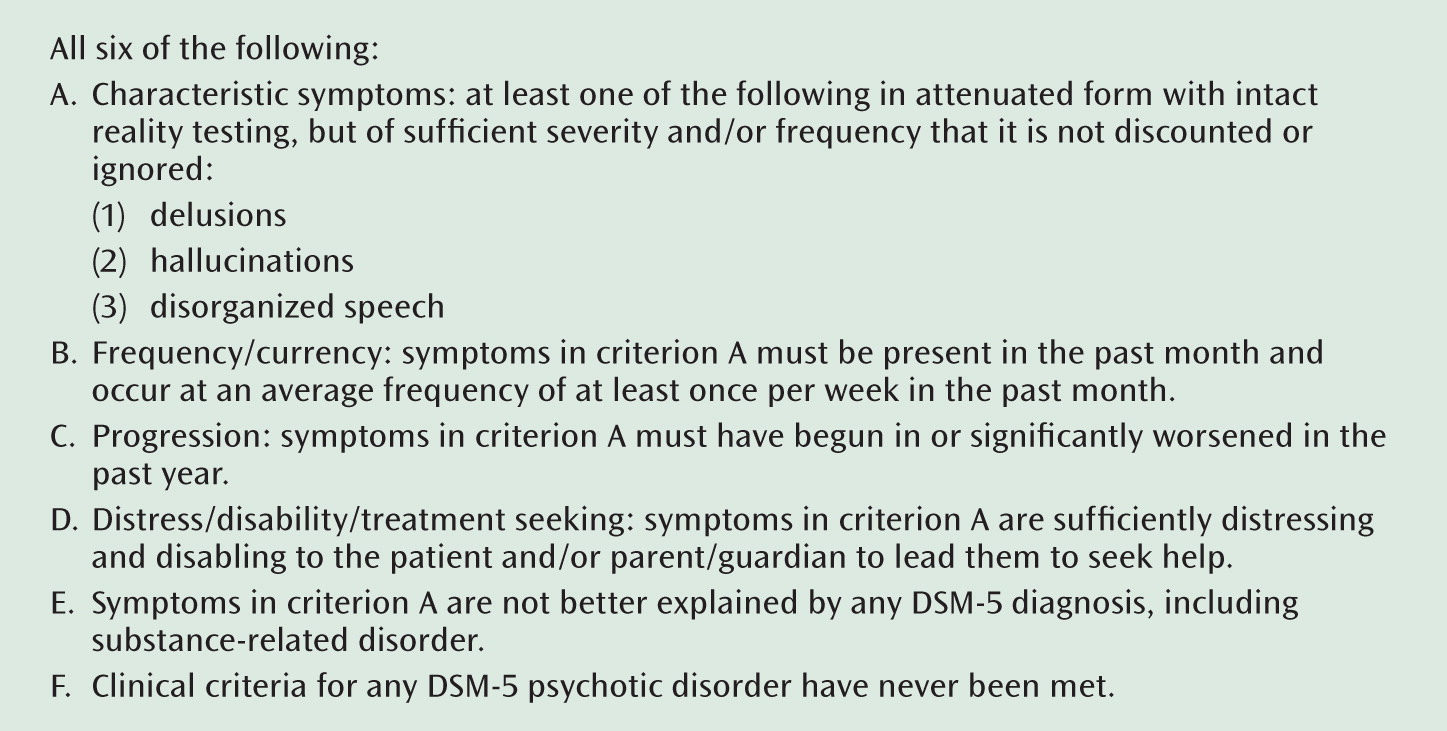
The DSM-5 Psychosis Work Group, of which we are both members, is considering attenuated psychosis syndrome as a new diagnostic category (
Figure 1) (
1,
2). The proposed category reflects the clinical observation that many adolescents and young adults who eventually develop psychotic disorders such as schizophrenia first manifest less severe but still troubling psychotic symptoms in a several-year prodrome before the onset of more severe illness. Although not all individuals with these attenuated symptoms will develop a lifelong psychotic illness, the presence of such symptoms appears to confer a higher risk. An axiom of most medical practice is that early detection and treatment constitute an essential strategy to prevent more serious consequences of illness. However, there is as yet no consensus that this new diagnosis will be helpful in that regard. In this brief commentary we note some of the more controversial points.
Can Increased Risk for Psychosis Be Reliably Diagnosed in Individuals?
A substantial body of prospective research has established that individuals who develop attenuated psychotic symptoms accompanied by dysfunction at school and similar problems at home are much more likely than individuals in the general population to develop schizophrenia or other psychotic disorders within 2 years (at a rate of 10%–30% compared with 0.02%). The research has been conducted at multiple sites in the United States and Europe, and the convergence on a set of criteria that can be diagnosed reliably by different observers and have the external validity of leading to a dire illness has been established (
3–
5).
Attenuated psychosis syndrome arose from attempts to identify individuals who, based on their current symptoms, would likely develop schizophrenia within the next several years. The current diagnostic scheme, which does not contain this prodromal prediction, nonetheless requires prodromal features—specifically, an acceleration in symptom manifestation. Patients and their families can be poor historians, particularly when a time course must be established. Many attenuated symptoms are quite stable and do not lead to more severe illness, as in individuals who have schizotypal personality disorder, who rarely become psychotic, or in the nearly 10% of normal individuals who believe in sorcery or aliens or hear voices. The criterion that the patient must retain reality testing is notoriously subjective and can be met by some individuals who already have schizophrenia. The 10% conversion rate to schizophrenia is provocative, but it occurs in research settings that inevitably attract ill individuals at rates disproportionate to the overall population. However, the clinical care provided may be protective in these settings. It is not clear that if these criteria were to be applied more widely, perhaps even by school guidance counselors dealing with problematic children, they would yield a group with this high a conversion rate.
Will the Diagnosis Promote Helpful Treatment for These Individuals?
It should be emphasized that current distress is a necessary criterion for this diagnosis. These individuals already need help because of behavioral and cognitive problems at school and at home. They need psychological help and, in some cases, medication, which they cannot receive in most health care systems if they have not received a commensurate diagnosis. Without a diagnosis, the consequence is that they cannot get help in the stage of illness when it might be most helpful for the prevention of chronic illness. In Norway, for example, efforts directed at early recognition of individuals with attenuated psychotic symptoms have resulted in an overall reduction in suicide rate because individuals have their treatment relationship initiated before they reach their sickest state. Even if they do not convert to psychosis, however, their distress and dysfunction are severe enough to merit help.
However, there is no proven treatment for this syndrome. Attempts to institute early antipsychotic treatment have shown no long-lasting effect and, of course, exposed the majority of individuals who would not have become ill to medications whose side effects we accept only with clear clinical indication of benefit. There may also be the inevitable tendency to diagnose attenuated psychosis syndrome in individuals who already have schizophrenia, which may paradoxically delay pharmacotherapy.
Will the Diagnosis Stimulate Research to Prevent Psychotic Disorders?
Just as clinical treatment cannot proceed efficiently without a diagnosis, research also requires a consensus among researchers and funding agencies that a population of affected persons can be identified. Since the prodromal syndrome has been identified as attenuated psychotic symptoms, we have had brain imaging studies to identify its neurobiological basis and an initial clinical trial with a safe and now possibly effective dietary treatment (
6).
But most of the factors that influence the development of schizophrenia that can be modified require public health efforts, not the identification and treatment of individuals. Perinatal malnutrition and maternal infection, for example, are much earlier factors that operate on a population-wide basis. At the onset of psychosis, drug abuse and urban crowding are factors that influence outcome. At the population level, these factors are not amenable to individual treatment by physicians but require public health efforts. The early engagement of patients in Norway was an outreach to an entire population with fliers in libraries and schools, and all sector primary care medical doctors were also targeted and educated (
7).
Will the Diagnosis Unnecessarily Stigmatize Individuals, or Will It Actually Promote Their Acceptance?
It was not long ago that clinicians hesitated to inform patients and their families of the initial diagnosis of schizophrenia, because it was feared that it would be devastating to them. The hope that symptoms might abate reinforced reluctance to inform patients and their families prematurely. We now generally believe that the diagnosis of schizophrenia is sufficiently reliable that patients and their families benefit from understanding the severity and likely course of the illness. Individuals are stigmatized by their behavior, not their diagnosis. An understanding that even the onset of an illness may be altering a family member's behavior often leads to greater acceptance.
Still, many of the individuals who receive this diagnosis will be adolescents. Even if they eventually develop schizophrenia, it may be years before they manifest symptoms. Premature diagnosis may have negative consequences on the expectations and acceptance of others in the individual's social environment, both at school and at home, that may be harmful.
What Are the Next Steps?
There is general agreement that this proposed diagnosis, which so far has been made only in research settings, requires field testing outside the expert centers. It has been selected for field testing both in other academic medical centers and in individual practices. Field testing will assess whether the diagnosis can be made reliably over time by different clinicians on the same patient and in agreement with those who have conducted the initial research. If it cannot, the diagnosis may be added in the appendix to DSM-5 for research purposes. If it can be made reliably, then the issues raised above about whether it is a helpful diagnosis will receive further consideration.