Over half this issue of
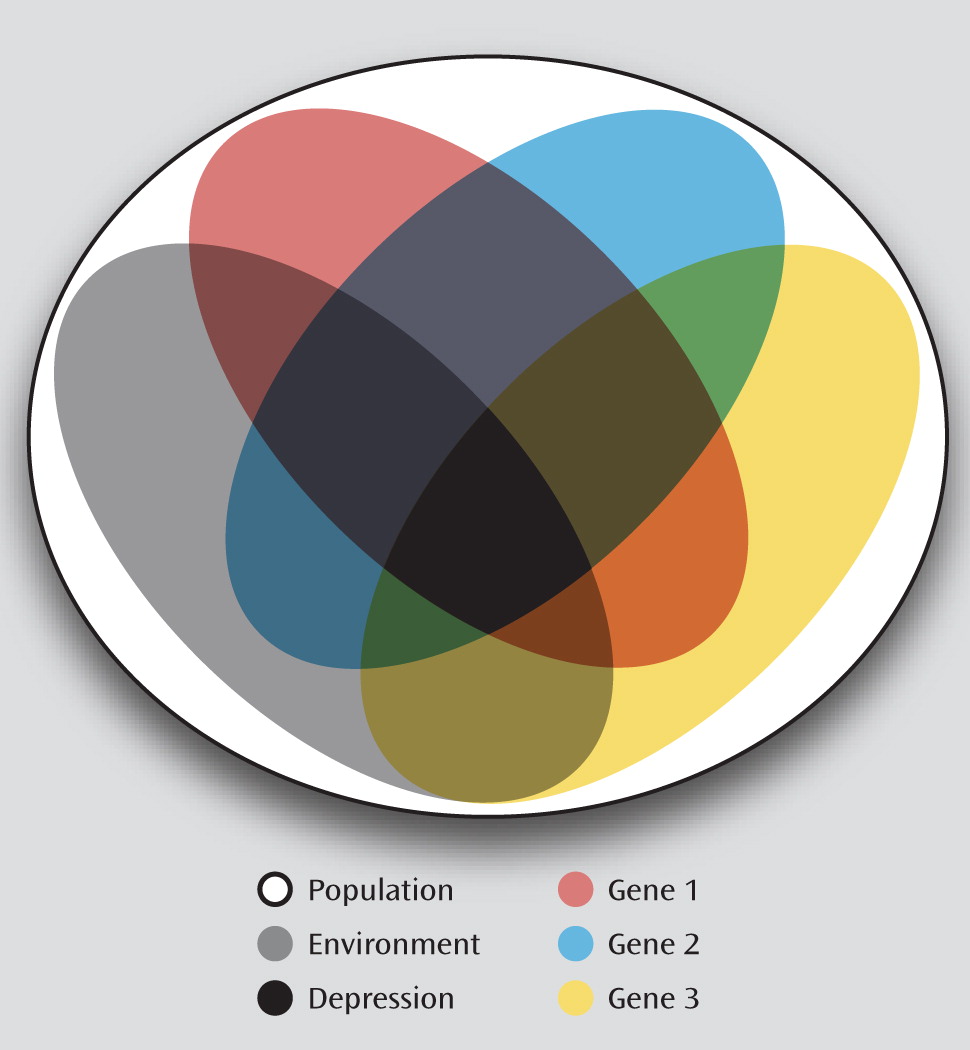
The American Journal of Psychiatry is devoted to articles on the genetics of psychiatric illness. Despite extensive epidemiological evidence for the heritability of many psychiatric illnesses, controversy continues over the reliability of the major genetic findings in this field. Study designs that focus on identifying a single gene cause of disease, while successful for rarer illnesses like cystic fibrosis and muscular dystrophy, have long been abandoned in psychiatry. Most common illnesses, including psychiatric disorders, are not determined by a single gene variant but rather occur because of complex interaction between multiple genes and environmental factors. Two fundamentally different approaches, illustrated by studies in this issue, can help with this complexity. One approach is to increase the complexity of the disease models to better match the likely reality, such as studies that explicitly model gene-environment or gene-gene interactions. While conceptually straightforward, modeling this additional complexity can require larger samples to maintain adequate power. The second approach is to switch from the study of clinical illness to related traits that are hopefully controlled by simpler genetics. A caveat here is that the genetics of these alternative traits actually may be as complex as standard clinical entities. However, if a trait that is more directly controlled by a specific gene variant is identified, it can be more powerful for genetic studies. Such a trait could even be used for studies in well populations, as many healthy individuals will have a genetic variant associated with disease risk (
Figure 1). Additionally, the always imprecise work in human subjects can be complemented by approaches that use animals or human cells that are grown in the laboratory and subjected to strict experimental controls. None of these designs are perfect, and concerns have been raised over each. Indeed, the review and overview article in this issue of the
Journal, by Duncan and Keller (
1), contributes to these concerns about reliability and is appropriately titled “A Critical Review of the First 10 Years of Candidate Gene-by-Environment Interaction Research in Psychiatry.” The purpose of this editorial is not to try to resolve these controversies but rather to let our readers know what these articles, despite appropriate reservations, teach us in order to justify our publishing them for you to read.
A landmark study conducted by Caspi et al. (
2) demonstrated that environmental factors could modulate the effect of a single genetic variant on the onset of depression. Individuals have two copies of the gene for the serotonin transporter, one on each of their maternally and paternally inherited chromosomes. Each copy can contain partially different DNA sequences, classified as long or short variants because of their different length, in a region called 5-
HTTLPR . The short variant produces less mRNA for the serotonin transporter, the protein that recycles serotonin into nerve terminals. The study was part of a lifelong examination of 1,000 individuals from a representative birth cohort, then 26 years old, in Dunedin, New Zealand. Stressful events were identified as unemployment, health problems, or similar losses in the past 5 years. Stressful events increased the new onset of major depression only in individuals who had at least one short variant of 5-
HTTPLR and had no effect in individuals who had two copies of the long variant. Although there was no independent effect of the genetic variant, its effects became manifest when stressful events occurred, a putative gene-by-environment interaction.
Dozens of studies have now examined variants in 5-HTTLPR in a variety of populations. Duncan and Keller argue that in the aggregate, the findings do not support the hypothesis that 5-HTTLPR has a significant interaction with stressful events to produce depression. Most of these studies have positive findings, but the findings frequently involve other genes or alternative definitions of what is stressful or even different outcomes, like posttraumatic stress disorder. None of this is surprising. What is stressful differs across populations. Death of a parent or sibling is certainly a universal trauma, but the paradigm has been applied to other types of trauma as well (e.g., the damage from hurricanes or terrorist attacks). Nor is it surprising that variants in multiple genes should be involved in these interactions, as human behavior is not determined by one gene. However, the failures of replication still are cause for concern. The null hypothesis is not that genes and environment do not interact to produce psychiatric illness but rather that too many genetic variants and environmental factors interact to the point that they cannot be easily disentangled and identified by methods currently in use. For the goal of using genetic research to quickly identify new targets for intervention, the sobering article by Duncan and Keller dims the light of optimism.
The four research articles in this issue use a variety of study designs to dig more deeply to move the field forward. The
FKBP5 gene modulates function of glucocorticoid receptors and has been frequently studied as a risk factor for depression and suicidality. Zimmermann et al. (
3) extended the study of this gene in their article “Interaction of
FKBP5 Gene Variants and Adverse Life Events in Predicting Depression Onset: Results From a 10-Year Prospective Community Study.” This long-term study, conducted in Munich, Germany, found a gene-by-environment effect for minor variants in the gene in the presence of trauma but not deprivation. Both these factors are considered to induce psychosocial stress, but as Duncan and Keller noted in their review, stressors that produce gene-by-environment effects in one study may not easily replicate to another. In this case, Zimmermann et al. successfully found replication in a similar study conducted in the United Kingdom but not in the New Zealand sample in which Caspi et al. found effects for
5-HTTPLR .
In their article, “Effects of the Circadian Rhythm Gene Period 1 (
Per1) on Psychosocial Stress-Induced Alcohol Drinking,” Dong et al. (
4) present another gene-by-environment study, but it included multiple complementary types of experiments. The
Per1 gene was originally discovered as a clock gene that regulates the daily cycle of activity in mice. Because gene expression is modulated by cortisol, it was suspected that it participates in stress response. Since the frequency of alcohol drinking is also influenced by stress, Dong et al. hypothesized that
Per1 might mediate some of these stress effects. A set of genetic analysis provided the means to test this hypothesis. Mice genetically engineered to express less
Per1 were stressed by exposure to a dominant mouse and showed increased alcohol intake compared with genetically normal mice. Frequency of heavy drinking in an epidemiological cohort of human adolescents demonstrated a direct genetic association with a variant in
Per1 as well as a gene-by-environment interaction with psychosocial adversity. A case-control study of adults also showed association of the same gene variant with alcohol dependence. Finally, the authors examined the molecular biology of
Per1 in the peripheral blood cells of people who carried a variant associated with alcoholism and showed that their cells were less able to express the gene when they were stimulated with cortisol. Thus, converging evidence from an animal model, two human populations (one at risk and the other with confirmed alcoholism), and molecular studies on the human gene itself has provided a chain of support for the hypothesis of a role for the
Per1 gene and its response to cortisol as a mechanism modulating the influence of psychosocial stress on alcoholism.
In their study titled “Nitric Oxide Synthase Genotype Modulation of Impulsivity and Ventral Striatal Activity in Adult ADHD Patients and Healthy Comparison Subjects,” Hoogman et al. (
5) utilized functional imaging to examine a trait of interest in ADHD and showed that genetic analysis does not always confirm a hypothesized mechanism.
NOS1 is a gene for nitric oxide synthase, which participates in the signaling of effects of neurotransmitters by forming the intracellular messenger nitric oxide in response to calcium influx produced by a variety of neurotransmitters, ranging from glutamate to acetylcholine.
NOS1 has been associated with increased risk for ADHD and with the trait of impulsivity, one of the cardinal features of ADHD. Since ADHD and, in particular, impulsivity are related to decreased ventral striatal activity, Hoogman et al. hypothesized that the
NOS1 genotype itself might also be related to decreased ventral striatal activity. Such a finding would demonstrate a mechanism for the decreased ventral striatal activity that seems to underlie impulsivity and ultimately ADHD. However, research progress relies on the ability to refute as well as to substantiate hypotheses. Hoogman et al. found instead that
NOS1 variants associated with ADHD are actually associated with increased ventral striatal activity. Thus, the effect of
NOS1 must involve a change in activity elsewhere in the brain, and the decreased ventral striatal activity must happen through other mechanisms.
Finally, in their study titled “Association of the Alzheimer's Gene
SORL1 With Hippocampal Volume in Young Healthy Adults,” Bralten et al. (
6) detected an effect of the
SORL1 gene before the onset of an illness that will only affect some of the study participants much later in life. Genes commonly have variation at multiple locations along their length. Statistical methods exist to sum the effects of many variants, most of them rare, and analyze their effect on a trait of interest. Bralten et al. used these methods in two separate cohorts to show that multiple variants in
SORL1 contributed to decreased hippocampal size. Variants in this gene have previously been established to increase the risk for Alzheimer's disease; these findings suggest a biological basis for this effect and thus raise the possibility that it might be prevented. It is also noteworthy that Bralten et al. were able to distinguish the effects of
SORL1 from those of another common Alzheimer's risk gene,
APOE.A conundrum raised by all four research articles is that the authors necessarily had to select a single gene, a single stressful factor, and a single brain structure or function to examine in detail. Duncan and Keller pointed out that genome-wide association studies (GWASs) rarely identify one of these candidate genes as a major site of heritability. More frequently, GWASs appear to identify novel regions of chromosomes that may or may not contain genes with known function. An equally serious issue is that no strategy currently exists to reaggregate the bits of information from these and other articles into a coherent view of the pathophysiology of illness. Nonetheless, the information that is being gained may have clinical payoff before a complete solution to the problem of how illness occurs is reached. The 5-HTTLPR variant whose effects seem so ephemeral is in fact part of the gene that produces the serotonin transporter, the target of selective serotonin reuptake inhibitors and an effective treatment for depression. If a gene whose effect is so weak as to be seen in only a minority of studies can be an effective target for treatment, then there would seem to be good reason to continue to dig deeply to identify more such targets and to understand how their biological effects contribute to human illness.