Change in Defense Mechanisms During Long-Term Dynamic Psychotherapy and Five-Year Outcome
Abstract
Objective
Method
Results
Conclusions
Method
Design and Study Participants
Therapists
Psychotherapies
Study Procedures
Measures
| Order | Category | Defense Level | Individual Defenses |
|---|---|---|---|
| 7 | Mature | High adaptive | Affiliation, altruism, anticipation, humor, self-assertion, self-observation, sublimation, suppression |
| 6 | Neurotic | Obsessional | Isolation of affect, intellectualization, undoing |
| 5a | Neurotic | Hysterical | Repression, dissociation |
| 5b | Neurotic | Other neurotic | Reaction formation, displacement |
| 4 | Immature | Minor image-distorting (narcissistic) | Devaluation of self or object images, idealization of self or object images, omnipotence |
| 3 | Immature | Disavowal | Denial, rationalization, projection. Although not a disavowal defense, autistic fantasy is scored at this level |
| 2 | Immature | Major image-distorting (borderline) | Splitting of other’s images, splitting of self-images, projective identification |
| 1 | Immature | Action | Acting out, passive aggression, help-rejecting complaining |
| 1–7 | Overall defensive functioning | A summary variable consisting of the mean of each defense used, each weighted by its level |
Statistical Analysis
Results
| Beginning of Therapy | 2.5 Years of Therapy | Raw Difference | Median Effect Size | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Measure | Median | Mean | SD | Median | Mean | SD | Median | Mean | SD | pa | |
| Defense levels | |||||||||||
| 7. High adaptive | 0.087 | 0.093 | 0.042 | 0.117 | 0.133 | 0.080 | 0.036 | 0.039 | 0.075 | 0.80 | 0.04; 0.38 |
| 6. Obsessional | 0.297 | 0.281 | 0.093 | 0.264 | 0.270 | 0.105 | 0.007 | –0.010 | 0.074 | 0.08 | 0.96 |
| 5a. Hysterical | 0.102 | 0.099 | 0.056 | 0.081 | 0.093 | 0.062 | –0.019 | –0.007 | 0.047 | –0.34 | 0.16 |
| 5b. Other neurotic | 0.121 | 0.124 | 0.050 | 0.136 | 0.141 | 0.062 | 0.022 | 0.017 | 0.054 | 0.44 | 0.27 |
| 4. Minor image-distorting | 0.135 | 0.144 | 0.080 | 0.124 | 0.132 | 0.080 | –0.014 | –0.012 | 0.049 | –0.32 | 0.65 |
| 3. Disavowal | 0.158 | 0.156 | 0.033 | 0.140 | 0.150 | 0.063 | 0.009 | –0.006 | 0.073 | 0.26 | 0.51 |
| 2. Major image-distorting | 0.011 | 0.018 | 0.021 | 0.004 | 0.029 | 0.059 | –0.006 | 0.006 | 0.042 | –0.29 | 0.13; 0.007 |
| 1. Action | 0.090 | 0.086 | 0.050 | 0.040 | 0.059 | 0.053 | –0.041 | –0.047 | 0.028 | –0.83 | 0.01; 0.04 |
| Tripartite categories | |||||||||||
| High adaptive (level 7) | 0.087 | 0.093 | 0.042 | 0.117 | 0.133 | 0.080 | 0.036 | 0.039 | 0.075 | 0.80 | 0.04; 0.03 |
| Neurotic (levels 5 and 6) | 0.507 | 0.504 | 0.094 | 0.511 | 0.504 | 0.102 | 0.021 | 0.000 | 0.084 | 0.23 | 0.35 |
| Immature (levels 1, 2, 3, and 4) | 0.383 | 0.403 | 0.084 | 0.333 | 0.363 | 0.139 | –0.056 | –0.039 | 0.115 | –0.67 | 0.14 |
| Summary variables | |||||||||||
| Overall defensive functioning | 4.64 | 4.62 | 0.27 | 4.88 | 4.80 | 0.51 | 0.19 | 0.18 | 0.45 | 0.71 | 0.05; 0.03 |
| Total number of defenses | 58.18 | 54.14 | 17.07 | 47.66 | 51.71 | 19.48 | −5.62 | −2.43 | 13.90 | –0.33 | 0.45 |
| Measure | Correlationa | ||||||
|---|---|---|---|---|---|---|---|
| Defense level | Action | Major imageb | Disavow | Minor image | Other neurotic | Hysterical | Obsessional |
| 7. High adaptive | –0.48* | –0.30 | –0.38 | –0.53* | –0.20 | –0.17 | 0.18 |
| 6. Obsessional | –0.53* | –0.09 | –0.41† | 0.04 | –0.42† | –0.63** | |
| 5a. Hysterical | 0.54* | 0.05 | 0.15 | –0.25 | 0.20 | ||
| 5b. Other neurotic | –0.20 | 0.23 | –0.16 | –0.45* | |||
| 4. Minor image-distorting | 0.31 | 0.11 | 0.14 | ||||
| 3. Disavowal | 0.17 | –0.08 | |||||
| 2. Major image-distortb | –0.09 | ||||||
| 1. Action | |||||||
| Tripartite categories | Neurotic | High adaptive | |||||
| Neurotic (levels 5–6) | –0.02 | ||||||
| Immature (levels 1–4) | –0.57** | –0.74*** | |||||
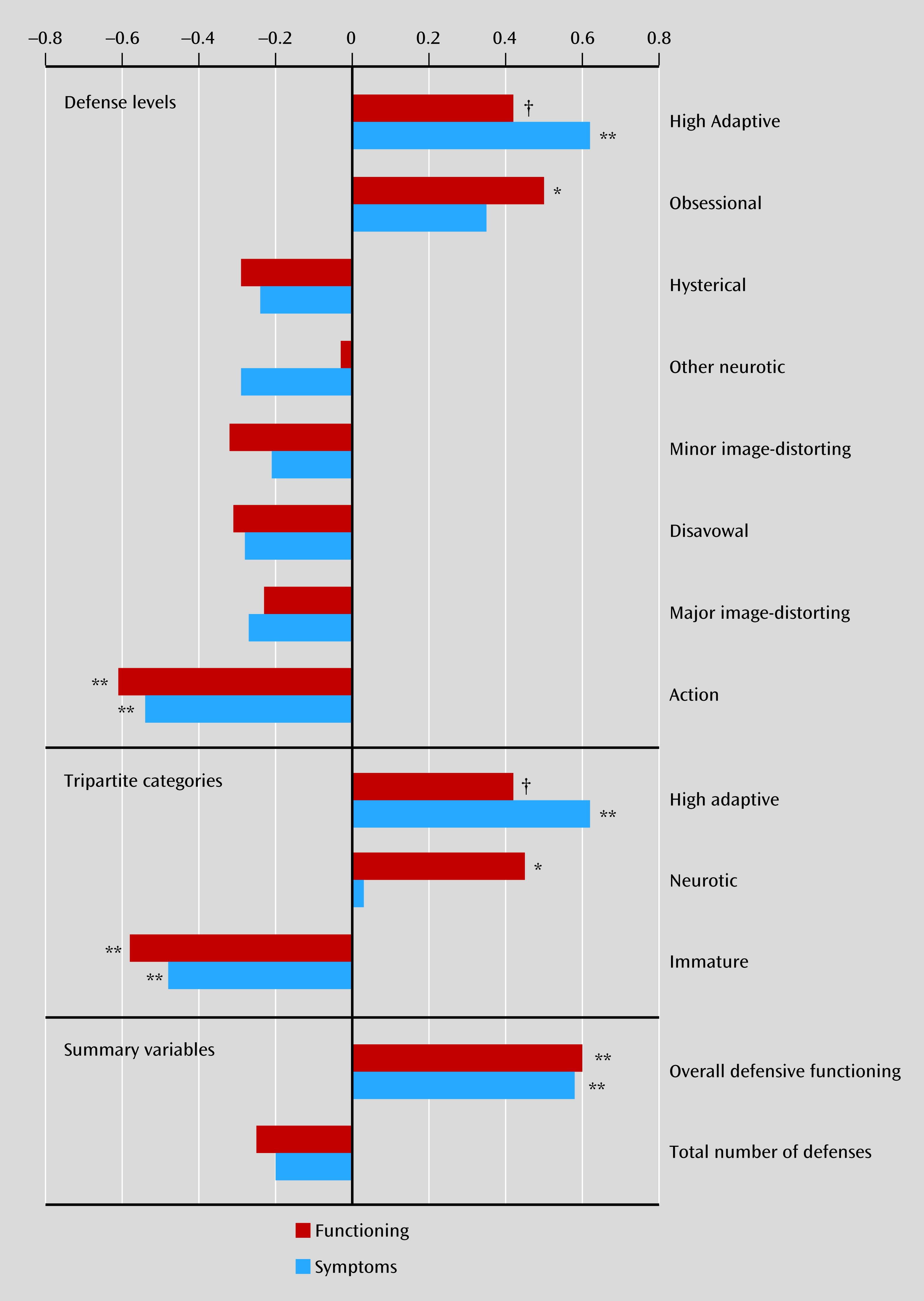
| Measure | rs for Functioning | rs for Symptoms |
|---|---|---|
| Defense levels | ||
| 7 High adaptive | 0.42† | 0.62** |
| 6 Obsessional | 0.50* | 0.35 |
| 5a Hysterical | –0.29 | –0.24 |
| 5b Other neurotic | –0.03 | –0.29 |
| 4 Minor image-distorting | –0.32 | –0.21 |
| 3 Disavowal | –0.31 | –0.28 |
| 2 Major image-distorting | –0.23 | –0.27 |
| 1 Action | –0.61** | –0.54** |
| Tripartite categories | ||
| High adaptive (level 7) | 0.42† | 0.62* |
| Neurotic (levels 5 & 6) | 0.45* | 0.03 |
| Immature (levels 1 through 4) | –0.58** | –0.48* |
| Summary variables | ||
| Overall defensive functioning | 0.60** | 0.58* |
| Total number of defenses | –0.25 | –0.20 |
Discussion
Case 1: Changes in Defenses With Good Outcome
History
Early in Treatment
Later in Treatment and Outcome
Case 2: Minimal Changes in Defenses With Poor Initial Outcome
History
Early in Treatment
Later in Treatment and Outcome
Longer-Term Outcome
References
Information & Authors
Information
Published In
History
Authors
Funding Information
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBLogin options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).