Given that bipolar disorder is strongly genetically determined, children of patients with bipolar disorder (bipolar offspring) constitute an at-risk population that can provide us with better insight into the development and early course of bipolar disorder. In 1997, Lapalme et al. (
1) showed in a meta-analysis (N=2,973) that bipolar offspring have 2.7 times the risk of developing a mental disorder and 4 times the risk of developing a mood disorder compared with children of healthy parents. More recently, two review articles on bipolar offspring reported elevated but varying prevalence rates of bipolar disorder (ranging from 3% to 27%), mood disorders (ranging from 5% to 67%), and non-mood disorders (ranging from 5% to 52%) (
2,
3). However, these studies could not fully address the development and early course of bipolar disorder and other mood disorders because they used either a cross-sectional design or a longitudinal design without follow-up into adulthood (
1–
12). We report here on one of the largest prospective bipolar offspring studies with a follow-up into adulthood: the 12-year follow-up of the Dutch bipolar offspring cohort (
7,
10,
12).
To date, only four bipolar offspring cohort studies have prospectively followed bipolar offspring for more than a decade. The first, a U.S. study conducted by Meyer et al. (
13), has had the longest follow-up to date, although it has a small sample. The study started in 1979 with 76 mothers with a mood disorder, including 25 mothers with bipolar I or II disorder with 48 bipolar offspring (ages 1.5–7 years at baseline), and 45 healthy community subjects. At the young adult follow-up assessment 23 years later, 19% of the 32 bipolar offspring who were still in the study had developed bipolar disorder; of these, 6% were diagnosed with bipolar I disorder and 13% with bipolar II disorder. The second study is the bipolar offspring cohort from the Amish population followed by Egeland et al. for 16 years (
14,
15). This sample included 115 bipolar offspring (ranging from age 13 to beyond age 30) from 15 families with a parent with bipolar I disorder and focused on prodromal symptoms of bipolar I disorder. After 16 years of follow-up, 7% of offspring had developed bipolar I disorder. In addition, bipolar offspring more often showed potentially prodromal characteristics compared with offspring of healthy families (39.2% and 5.9%, respectively). The third study is that of Duffy et al. in Canada (
16), started in 1995 with 36 children (ages 10–25 years) from 23 families (with bipolar I and II disorders). Over the past 15 years, Duffy et al. expanded their cohort to 220 children (ages 8–25 years) with a maximum follow-up of 15 years. At a mean age of almost 25 years, 71.4% of the bipolar offspring had received a DSM-IV axis I diagnosis: 55% had developed a mood disorder, including 16.3% with a bipolar spectrum disorder (2.7% bipolar I disorder, 5.9% bipolar II disorder, 5.5% bipolar disorder not otherwise specified, and 1.8% schizoaffective disorder, bipolar type) (
3,
16,
17). Despite different methods, the main finding of these studies is the same: low rates of bipolar I diagnoses compared with other mood disorders and psychopathology in general.
The fourth study, which we present here, is the Dutch bipolar offspring cohort, a fixed sample of 140 bipolar offspring from 86 families (with bipolar I and II disorders) followed from adolescence into adulthood to a mean age of 28 years (
7,
10,
12). At the 5-year follow-up (mean age, 21 years), we found lifetime prevalence rates of 40% for any mood disorder, 10% for bipolar disorder (3.9% for bipolar I disorder and 6.1% for bipolar II disorder), and 59% for psychopathology in general. Furthermore, in all participants with bipolar disorder, the illness started with a depressive episode. Based on survival analysis, we predicted a further increase in bipolar disorder and unipolar depression in the coming years as the cohort further matured into adulthood (
7). In the present study, we sought to provide a thorough description of the onset and early developmental trajectories of mood disorders and other psychopathology in bipolar offspring.
Results
A total of 108 offspring (58 of them male; mean age, 28.0 years [SD=2.82]) participated in the 12-year assessment.
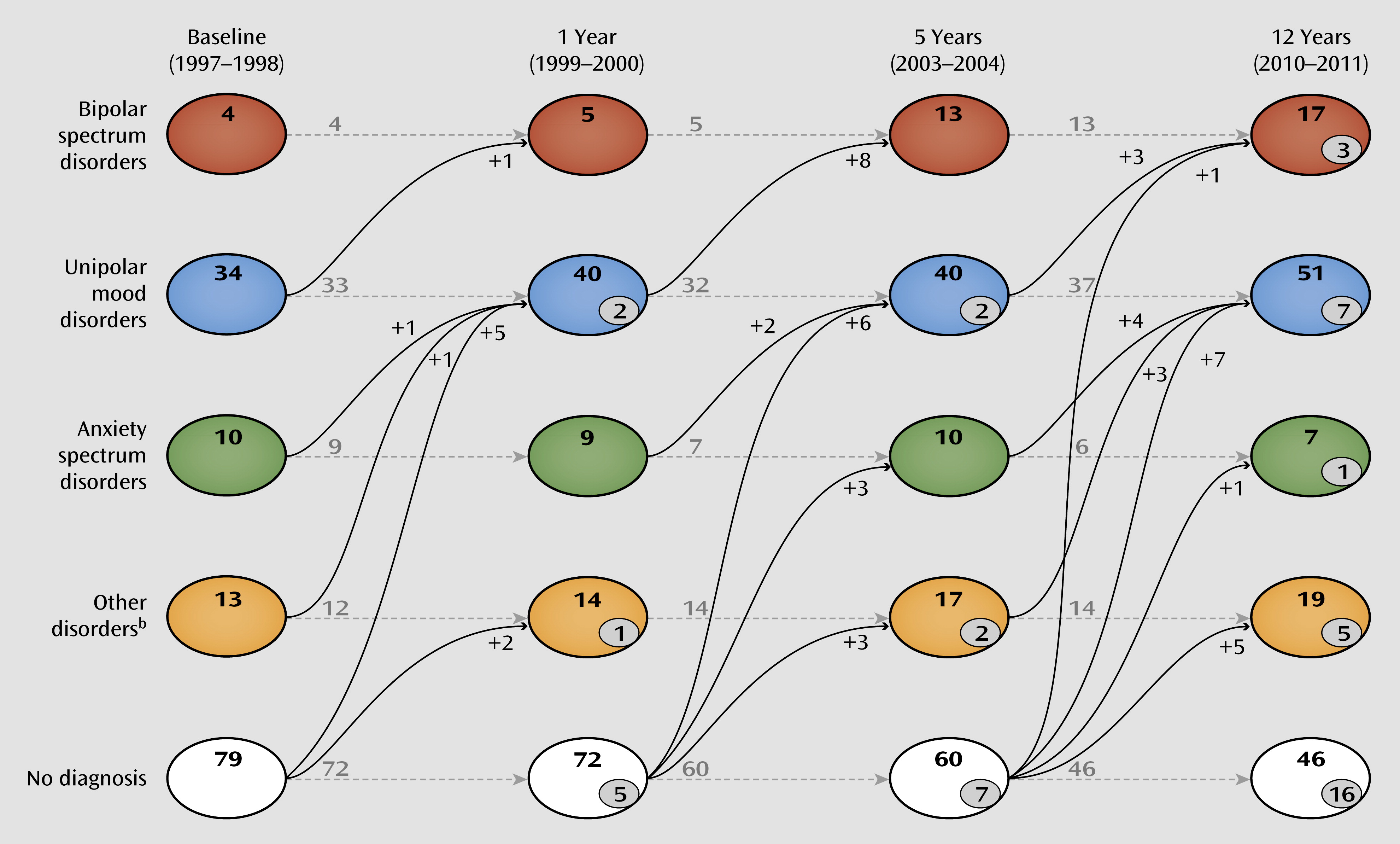
Table 2 presents the prevalence of lifetime psychopathology at baseline and at 12 years. Over the 12 years of follow-up, the prevalence of mood disorders doubled, with the result that now more than half of the cohort is positive for a lifetime mood disorder, including 13% with lifetime bipolar spectrum disorders. None of the bipolar offspring developed a primary psychotic disorder without affective symptoms. Overall, more than 70% of the cohort met the criteria for at least one lifetime DSM-IV axis I disorder.
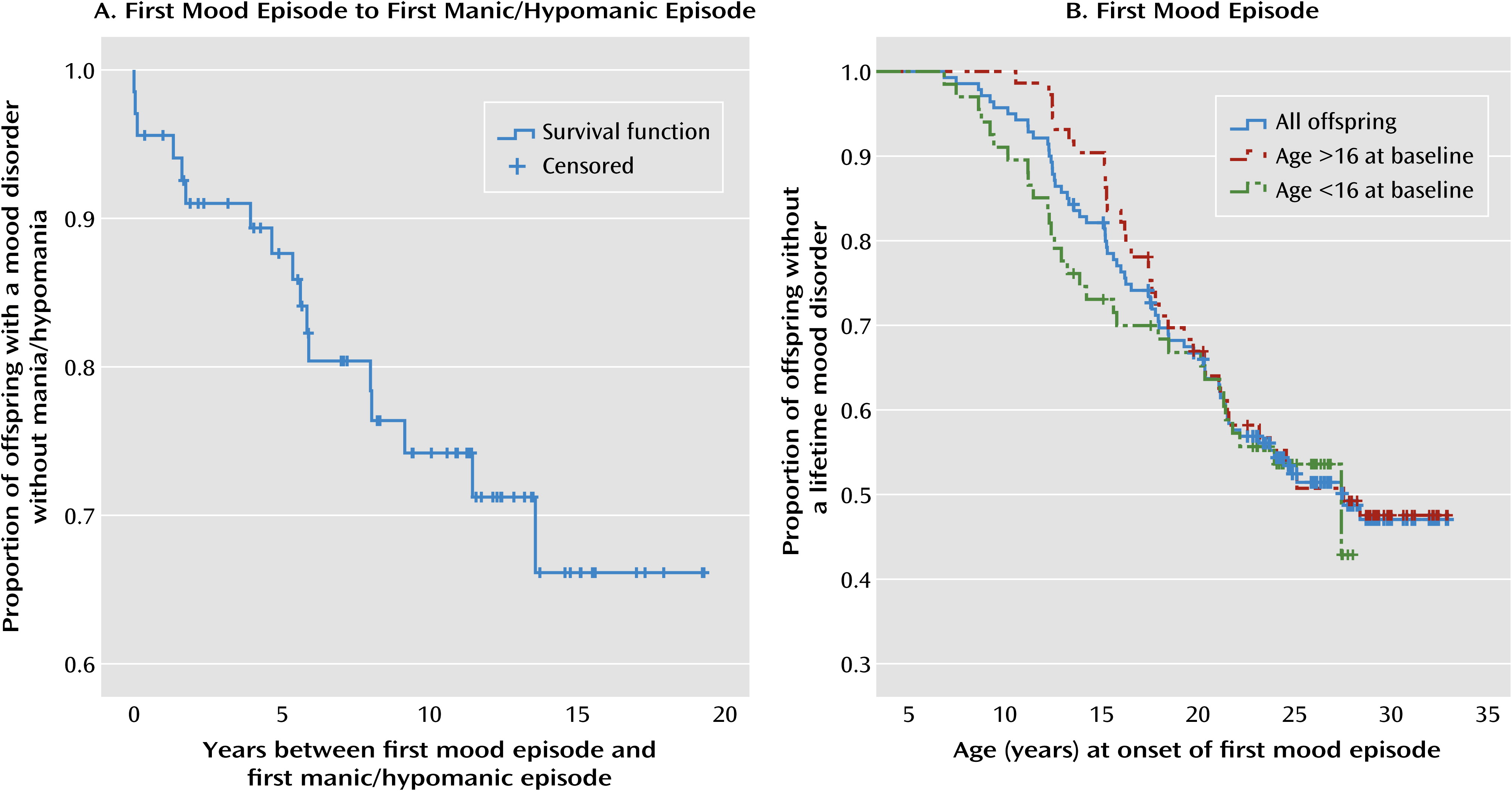
Table 3 summarizes the clinical characteristics of the 17 participants from 15 families who developed a bipolar spectrum disorder during the 12-year follow-up period. Twelve (80%) of the 15 bipolar parents had bipolar I disorder, which is not statistically different from the distribution in the overall group of parents (74%). In 88% of offspring with a bipolar spectrum disorder, the illness began with a depressive episode; in two offspring, the illness started with cyclothymia. The mean age at onset of the first mood episode was 14.6 years (SD=4.65, range=8.6–23.7), and onset of the first manic or hypomanic episode followed on average 5.3 years later (SD=4.10, range=0–13.6; see also
Figure 1A). We found no significant difference between age at hypomania onset (median=17.3 years) and age at mania onset (median=20.2). Five participants (29%) had their first depressive episode before age 12 (i.e., prepubertal onset). None of the participants had a prepubertal hypomanic or manic episode. Two participants were diagnosed with ADHD. Nine participants (53%) had a comorbid anxiety disorder; in four of them, the anxiety disorder was present before the onset of their first mood episode or was diagnosed around the same time. All 17 offspring with a bipolar spectrum disorder received psychiatric treatment (pharmacologic, 71%; counseling, 100%) currently or in the past; six offspring had been hospitalized at least once. With regard to pharmacological treatment, only one participant switched into hypomania after starting treatment with an antidepressant. One participant received a stimulant because of comorbid ADHD (before the onset of bipolar II disorder). For more detail on the characteristics of this group, see Table S1 in the data supplement that accompanies the online edition of this article.
Apart from being at risk for bipolar spectrum disorders, bipolar offspring are at substantial risk for developing mood disorders in general. More than half of the cohort (54%) developed a lifetime mood disorder by a mean age of 28 years. The average age at onset of the first mood episode was 17.2 years (SD=5.33, range=6.8–28.4). Of the 58 bipolar offspring with a lifetime mood disorder, 14 (24%) developed a bipolar spectrum disorder during follow-up, and 19 (33%) had a recurrent unipolar depression; taken together, 33 (31%) of the bipolar offspring had a recurrent mood disorder. Among participants with a lifetime mood disorder (N=58), the lifetime prevalence of psychopathology is much more complex: 67% had a comorbid lifetime disorder, including 34% with an anxiety disorder, 19% with a substance use disorder, 7% with a disruptive behavior disorder, 3% with ADHD, and 34% with other disorders (as defined in
Table 2). Comorbid disorders were present in 64% of offspring with bipolar spectrum disorders and in 68% of those with unipolar mood disorders. Overall, 71% of participants with a lifetime mood disorder contacted mental health care services at some time between the 5-year and 12-year follow-up assessments, and 33% had received pharmacological treatment. To provide a better insight into the developmental course toward the onset of mood disorders, the transition over the four assessments is depicted in
Figure 2.
Because the prevalence of first-onset mood disorders increased significantly over the 12-year follow-up period, we performed a Kaplan-Meier survival analysis to check whether a further increase in first-onset mood disorders can be expected in the future (see
Figure 1B). In contrast to the 5-year assessment, the slope of the Kaplan-Meier survival function appears now to level out after age 25. In total, only four of 52 offspring over the age of 25 have developed a first-onset mood disorder (data not shown).
Discussion
Our aim in this study was to provide data on the onset and developmental trajectories of mood disorders and other psychopathology in bipolar offspring. In summary, at a mean age of 28 years, more than half of the Dutch bipolar offspring cohort had developed a mood disorder, including 13% with bipolar spectrum disorders (3% with bipolar I disorder; 8% with bipolar II disorder; 1% with schizoaffective disorder, bipolar type; and 1% with cyclothymia) and 41% with a unipolar depressive disorder (major depressive disorder; dysthymia; depressive disorder not otherwise specified; or adjustment disorder, mood). None of the bipolar offspring developed a psychotic disorder without affective symptoms. In almost all participants with bipolar spectrum disorders, the illness started with a depressive episode. Among offspring with lifetime unipolar depression, 24% had a manic or hypomanic episode during follow-up, on average 5.1 years after their first unipolar mood episode. None of the offspring had a prepubertal onset of mania or hypomania. The risk of developing a first mood episode was highest up to age 25; only four participants developed a first mood episode after this age. Finally, we found that unipolar mood disorders in bipolar offspring were often recurrent (33% of the cases) and were prone to be complex (68% with comorbid disorders), and that 71% offspring with unipolar mood disorders received treatment from mental health services. Overall, 72% of the cohort developed a lifetime DSM-IV axis I disorder in 12 years of follow-up.
Our study has some limitations. First, it is not a population-based study: participants were recruited through the Dutch Association for Manic Depressives and Relatives and bipolar outpatient clinics across the country, suggesting a selection of better informed and treatment-seeking bipolar parents. Second, we had no control group of children of parents without bipolar disorder; however, we could compare our results with data from a comparable age group in the Netherlands Mental Health Survey and Incidence Study (NEMESIS-2) (
23–
25), a recently published Dutch population study. In that study, 1,123 participants in the age range of 25–34 years were psychiatrically evaluated using the Composite International Diagnostic Interview 3.0 (
26). Lifetime prevalence was 46.5% for any psychiatric disorder and 19.5% for any mood disorder, including 2.4% for bipolar disorder (without further specification). Although the diagnostic instruments were not identical, data from NEMESIS-2 confirm that the lifetime prevalence of mood disorders, bipolar disorders, and psychiatric disorders in general are considerably higher in our bipolar offspring cohort than in the Dutch general population. A third limitation is that at baseline, offspring were already between 12 and 21 years old; therefore, data on prepubertal and early adolescent disorders or episodes may be affected by a recall bias. In additional analyses (see Table S2 in the online data supplement), we divided our cohort into an early adolescence group (ages 12–16) and a late adolescence group (ages 16–21) at baseline and examined whether data on prevalence rates of psychopathology (per category) at baseline and at 12 years and age at onset of the first mood episode were affected by recall bias. We found no evidence for different rates of psychopathology. However, as depicted in
Figure 1B, the age at baseline likely affected the age at onset of mood disorders as reported by offspring and their parents. This supports the notion that diagnoses of internalizing disorders may be more affected by recall bias, since these diagnoses are mainly based on information from offspring (
27). Fourth, not specifically assessing for bipolar disorder not otherwise specified in this study may have affected our findings. However, of the four prospective studies of bipolar offspring that we mentioned earlier, only the Canadian study (
28) used the bipolar disorder not otherwise specified diagnosis, and the lifetime prevalence of bipolar spectrum disorders was also comparable to the three other studies. Despite limitations, the strengths of this study are the long follow-up period and the high retention rate (77%) of 108 bipolar offspring from adolescence into adulthood.
With regard to both age distribution and psychopathology outcome, our results compare best to those of the prospective Canadian bipolar offspring study from Duffy et al. (
3,
17). Cumulatively, their sample consists of 220 offspring with a mean age of 24.6 years (range=8–30) and a mean follow-up of 9.2 years (SD=4.16, range=1–15); 21.4% have been followed for the full 15 years (
28,
29; A. Duffy et al., personal communication, Feb. 2012). Despite some methodological differences, the prevalence rates in their study and ours are remarkably similar: bipolar spectrum disorders, 16.3% and 13%, respectively; mood disorders, 55% and 54%, respectively; and any axis I disorder, 71.4% and 72%, respectively. Moreover, in both studies, bipolar spectrum disorders began in the majority of the bipolar offspring with a depressive episode (86% and 88%, respectively) (
28). These similarities in prevalence rates appear to be at least partly the result of using the same assessment methods and including bipolar families with comparable socioeconomic status. In addition, the Dutch and Canadian health care systems provide easily accessible basic mental health care. Therefore, no sample selection occurred as a result of study participation in exchange for receiving mental health care.
Apart from these convergent findings, there are also some divergent findings worth mentioning between this and other bipolar offspring studies. Compared with the Duffy et al. study (
28), the onset of comorbid anxiety disorders in bipolar spectrum disorders was much later in our study (mean age, 10 years and 17 years, respectively). As described earlier, age at baseline may significantly affect age at onset. Duffy et al. recruited younger offspring and may therefore have detected (mild) anxiety disorders at an earlier stage. In general, we observed much higher rates of comorbid anxiety in bipolar spectrum disorders (28% compared with 52%). Also, whereas some bipolar offspring studies have reported elevated rates of ADHD and disruptive disorders (
4–
6,
11), we observed close to normal rates of ADHD and disruptive disorders, as did Duffy et al. (
3). Again, age at intake may be involved. We may have missed some of these diagnoses because of the age-dependent decline of ADHD symptoms, especially since symptoms of hyperactivity and impulsivity are less overt during adolescence (
30). Another possible factor could be the parental characteristics of these cohorts: all studies reporting high rates of ADHD and disruptive disorders in bipolar offspring also show high rates of ADHD in the parental cohort (
4–
6,
11). Furthermore, we found prevalence rates of substance use disorders close to those in the Dutch general population (23% and 25%, respectively) (
24). A possible explanation lies in the recruitment bias of our participating families. Most of these families (and their offspring) are members of the patient association, often aware of and well informed about the risks of substance use. Also, the relatively high socioeconomic status of our cohort may explain the low prevalence of substance use disorders (
31).
In the end, one of the most remarkable findings of this and the three other longitudinal studies of bipolar offspring with a follow-up into adulthood (
3,
11,
14) is that although the prevalence of mood disorders and other psychopathology in this population is high, the prevalence of bipolar I disorder is low compared with other forms of bipolar disorder. At the same time, the lifetime prevalence rate of recurrent mood disorders in our cohort was 31%. This finding points to the discussion of Kraepelin’s broad concept of manic-depressive illness, which included all recurrent mood disorders (
32). It is tempting to speculate that the genetic vulnerability comprises mainly the risk for mood instability and recurrences rather than the risk of developing full-blown mania. On the other hand, the long delay between the first unipolar mood episode and the onset of the first manic or hypomanic episode as found in this study may also suggest that the recurrent unipolar mood disorders in our cohort rather reflect the early stages of future bipolar disorder. These findings are in concordance with findings from a prospective study in adults by Angst et al. (
33), and this possibility is also proposed in several theoretical staging models (
34,
35). Apart from the meaning of recurrent depression in the concept of bipolar disorder, clinically it is important to realize that the depressive course in bipolar spectrum disorders is especially associated with a high burden of illness (
36). Furthermore, it is worth mentioning that although there is emerging evidence for shared genetic susceptibility and etiology between bipolar disorder and schizophrenia (
37), none of the bipolar offspring—in either the Dutch or the Canadian study—developed a primary psychotic disorder (
3).
In conclusion, after a 12-year follow-up of a large fixed bipolar offspring cohort, we found, like the three other existing prospective bipolar offspring studies, low rates of bipolar I disorders in adult bipolar offspring. Nevertheless, in all bipolar offspring studies, high rates of psychopathology and (recurrent) mood disorders have been observed (
1–
3,
9,
13,
15,
17). Therefore, early intervention appears indicated to enhance normal development and prevent the onset of mood disorders in bipolar offspring. Future follow-up of this and the other adult bipolar offspring cohorts is essential to determine whether recurrent mood disorders in bipolar offspring reflect the early stages of bipolar disorder.