The course of major depressive disorder is most frequently characterized by recurrences, with new depressive episodes causing significant disability and impairment of quality of life (
1). The probability of subsequent episodes increases with the number of previous episodes, and the interval between recurrences decreases with each new episode (
2). The risk of recurrence can be reduced by pharmacological maintenance treatment (
3). However, in clinical practice, long-term pharmacotherapy may be associated with a loss of clinical effects or prolonged side effects. Furthermore, a high level of adherence and acceptance by the patient and an accurate adjustment of the type of medication and dosage by the physician are required to achieve optimal effects (
4,
5).
Psychotherapies, particularly cognitive-behavioral therapy (CBT), which focus specifically on relapse prevention in remitted patients, have been proven effective (
6,
7). These approaches usually combine CBT with additional strategies to prevent recurrence, such as activating cognitive and behavioral skills (continuation phase cognitive therapy) (
8), improving psychological well-being and life balance (well-being therapy) (
9), modifying dysfunctional attitudes (
10), and meditation (mindfulness-based cognitive therapy) (
11–
14).
Although these findings are promising, it is not clear whether the effectiveness of these therapies might at least partially be explained by nonspecific factors. In most trials, the control group received treatment as usual, but in clinical practice this may not correspond to the attention and support provided by a health professional in continuous and regular visits (
15). Furthermore, in most studies, treatments were delivered in group settings, which may be additionally beneficial by providing encouragement and social support from other group members (
16). However, individual treatments are preferred in clinical practice settings. Finally, psychological treatments may implicitly also provide information about possible causes and additional measures for preventing depression. In fact, psychoeducation has been proven to be an effective intervention in the treatment of depression (
17,
18).
The main objective of our multicenter randomized controlled study was to compare the outcome of two active treatments, maintenance CBT and manualized psychoeducation, both added to treatment as usual for remitted outpatients with a history of recurrent depression. We predicted that maintenance CBT would be superior to manualized psychoeducation in the long-term prevention of recurrence. In line with Bockting et al. (
10), we expected the effect of maintenance CBT to be significantly greater in patients with a higher risk of recurrence (i.e., those with five or more previous depressive episodes) (
6,
10–
12).
Method
Overview
The study was designed as a multicenter prospective randomized observer-blinded study with two parallel groups. The patients had to exhibit stable remission for at least a 2-month run-in period before they were randomly assigned to one of two treatment conditions: maintenance CBT or manualized psychoeducation. Randomization stratified by center was employed via fax by the Interdisciplinary Center for Clinical Trials Mainz using permutated blocks to allocate patients to treatment. Treatments were assigned in a 1:1 ratio. Both treatment groups continued to receive the normal standard of psychiatric care. Independent raters who were blind to treatment condition assessed outcome criteria after the 8-month treatment phase and then every 3 months for up to 1 year. The protocol was approved by two independent ethics committees. All participants received a complete study description and gave written informed consent. The trial was conducted according to the International Conference on Harmonization Good Clinical Practices. Clinical monitoring, data management, central randomization, and statistical analysis were provided by the Interdisciplinary Center for Clinical Trials at Mainz University.
Participants
The participants were recruited from psychiatric hospitals, outpatient practices, and advertisements in local newspapers and the Internet. All individuals who were interested in the study took part in a telephone screening, and patients who appeared eligible were invited for a diagnostic interview. Eligibility for the study was determined with the Structured Clinical Interview for DSM-IV Axis I and II Disorders (SCID) (
19).
The study enrolled outpatients who met the following inclusion criteria: 1) diagnosis of recurrent nonpsychotic major depressive disorder, currently in remission; 2) a history of at least three major depressive episodes; 3) a score ≤9 on the Hamilton Depression Rating Scale (HAM-D) over 8 weeks before randomization; and 4) age 18–65 years.
Patients were excluded if they met the following criteria: 1) current or past diagnosis of an organic mental disorder, psychological or behavioral disorders caused by psychotropic substances, schizophrenia, schizoaffective disorder, bipolar disorder, borderline personality disorder, or mental retardation; 2) current diagnosis of adjustment disorder; 3) current acute suicidality; 4) severe comorbid medical condition; and 5) CBT in the 1 year preceding randomization.
Participants who were eligible for randomization entered a 2-month baseline interval in order to assess the stability of their remission. A HAM-D score ≤9 was used as the criterion for determining whether remission had remained stable over the 8 weeks before randomization.
Treatments
The experimental treatments comprised 16 individual sessions conducted over a period of 8 months. The session length was 20 minutes for manualized psychoeducation and 50 minutes for maintenance CBT, which are typical for these kinds of interventions. Both treatments were manualized (
20; unpublished 2006 manuscript of M. Hautzinger). The sessions were videotaped to assess therapist adherence. In addition to maintenance CBT or manualized psychoeducation, all patients received psychiatric treatment as usual, which included pharmacological continuation and maintenance treatment over the whole study period. Treatment with antidepressant medication was based on the guidelines of the German Psychiatric Association (
21), and the type of medication and dosage were individualized. The medication was changed or augmented only if intolerable side effects or depressive symptoms occurred. In this study, treatment as usual was restricted to basic psychiatric care, with long-term medication prescriptions and a 10-minute medication adjustment visit every 3 months.
Maintenance CBT.
Maintenance CBT is based on cognitive-behavioral approaches aimed at preventing recurrence of depressive episodes by using interventions from continuation-phase cognitive therapy (
8), well-being therapy (
9), mindfulness-based cognitive therapy (
11), and CBT (
10). The main elements of this treatment were cognitive case conceptualization (assessment of individual psychological risk factors for past recurrences, deriving a psychological model of recurrent depression); mindfulness meditation exercises; modification of dysfunctional cognitions and beliefs; behavioral activation; behavioral experiments and stress testing; and enhancement of cognitions and reinforcement of behaviors that increase psychological well-being. The sessions were initially scheduled weekly with increasing intervals between them; in the final phase, the sessions were scheduled monthly. Homework and work sheets were used to stimulate the self-guided development of skills to prevent recurrences.
Manualized psychoeducation.
Psychoeducation was intended to improve the clinical management of psychiatric care by delivering information on pharmacological and psychological measures for preventing relapses and recurrences. Tailored to the individual needs of the patient and based on specific information leaflets, psychoeducation covered the following topics: symptoms and course of depression; biopsychosocial model of etiology; pharmacological treatments for acute phase and maintenance; drug side effects and complications; medication compliance; early individual signs of recurrence; and management of relapse and recurrence. Based on the manual, therapists were instructed to give active advice, but they were not allowed to use any specific psychotherapeutic techniques (e.g., analysis of dysfunctional cognitions, skill training, life review, or problem solving) (
22). Therapists listened to the patient, gave space for expressing concerns and personal experiences, and reinforced the patient’s skills and resources, but focused mainly on education and information.
Therapists and Treatment Integrity
All therapists were either psychologists or psychiatrists with a least a master’s-level, doctoral, or medical degree and with advanced or completed postgraduate clinical training. No difference in clinical experience was found between the two therapist groups (maintenance CBT, 1.95 years; manualized psychoeducation, 1.46 years; F=0.27, df=45, p=0.61). A total of 26 therapists (25 psychologists, one psychiatrist) delivered maintenance CBT, and 28 therapists (23 psychologists, five psychiatrists) delivered manualized psychoeducation.
Before the trial began, maintenance CBT therapists attended three 15-hour training workshops in continuation-phase cognitive therapy (led by Robin Jarrett), well-being therapy (led by Giovanni Fava), and mindfulness-based cognitive therapy (led by T.H.) and one refresher workshop (led by U.S. and M.H.) to ensure that maintenance CBT was conducted according to protocol. Manualized psychoeducation training was provided in a 2-day workshop (given in Frankfurt by M.H. and A.B. and in Jena, Germany, by R.S. and Gregor Peikert).
In both interventions, adherence to the treatment protocol was regularly monitored in video-based supervision sessions. After each therapy session, all therapists completed a protocol in which the interventions applied in the session were documented.
To assess treatment integrity, two experienced psychologists were trained in the 15-item maintenance CBT adherence scale (
23) using randomly selected videotapes of 45 maintenance CBT sessions. Interrater reliability was very good; the intraclass correlation coefficient [ICC (2,2)] was 0.95 (p<0.001). Similarly, two raters were trained in the 12-item manualized psychoeducation adherence scale (
24) on the basis of 45 videotapes from manualized psychoeducation sessions, achieving a good interrater reliability of ICC(2,2)=0.81 (p<0.001). Mean scores were 1.12 (SD=0.39) for the maintenance CBT adherence scale and 1.55 (SD=0.33) for the manualized psychoeducation adherence scale. On the purity index (
25), which reflects the ratio of the intended therapy to the presence of intended and unintended therapy components, mean scores were 0.97 (SD=0.06; range, 0.80–1.00) for maintenance CBT and 0.98 (SD=0.08; range, 0.52–1.00) for manualized psychoeducation. Thus, in both treatments, a low proportion of interventions were used that were not part of the manual.
Outcome Measures
Patients were assessed by clinicians blind to treatment allocation 2 months before treatment, at baseline, after randomization, before and after the 8-month treatment, and the every 3 months for 1 year. Evaluators were trained and certified clinical psychologists reviewed by senior investigators (U.S., T.H., M.H.).
The primary outcome measure was defined before the study start as the time to relapse or to recurrence of a major depressive episode, according to DSM-IV criteria, using the Longitudinal Interval Follow-Up Evaluation (LIFE [
26]). Based on SCID criteria for major depressive episode, weekly psychiatric status ratings were recorded separately for the screening interval since the last visit. Raters were trained to use the LIFE by a certified trainer (Claire Walker) of the Keller et al. (
27) group at Brown University. In addition, interrater reliability was determined for all raters (N=16). Based on the weekly ratings of symptoms in four patients with recurrent depression, reliability was good (Kendall’s W=0.81, χ
2=450.77, df=35, p<0.001).
The severity of depressive symptoms was assessed at baseline and at seven consecutive visits using the 17-item HAM-D (
27). Based on the assessment of four patients, interrater reliability between clinical evaluators was again satisfactory (Kendall’s W=0.89, χ
2=18.84, df=3, p<0.001).
Statistical Analysis
The primary outcome was analyzed by a Cox proportional hazards regression model using intervention group and number of previous episodes (<5 or ≥5) as predictors. The primary endpoint of the study was time to first relapse as assessed by LIFE interviews. For individuals who dropped out of the study, the reason for discontinuation was classified. If they dropped out because of inefficacy or dissatisfaction with the therapy, the discontinuation was regarded as a major depressive episode relapse, with event time of the dropout date. Individuals who left for any other reason were considered as censored, with dropout date as censoring time. The number of previous episodes (<5 or ≥5) was further analyzed by log-rank tests, and four groups were derived for this analysis. We used Cox proportional hazards regression models to investigate concomitant antidepressant medication effects. To compare recurrence rates and categorical demographic data between both treatment conditions, we used Fisher’s exact test or the chi-square test; for numerical demographic data, we used t tests. For all tests, the threshold for statistical significance was set at 0.05 (two-tailed). All statistical analyses were conducted with data from the randomized sample according to the intent-to-treat principle and were prespecified in the statistical analysis plan. All analyses were performed using SAS version 9 (SAS Institute, Cary, N.C.).
The power calculation was based on a power of 0.80 (two-tailed significance at 0.05) and an expected difference in relapse rates between maintenance CBT and manualized psychoeducation of 20% at 1-year follow-up. With a total follow-up period of 20 months, the estimated sample size for the log-rank test was 84 patients per group. Because loss to follow-up was considered a relapse, no adjusted sample size for including dropouts had to be established.
Results
Patient Flow and Attrition
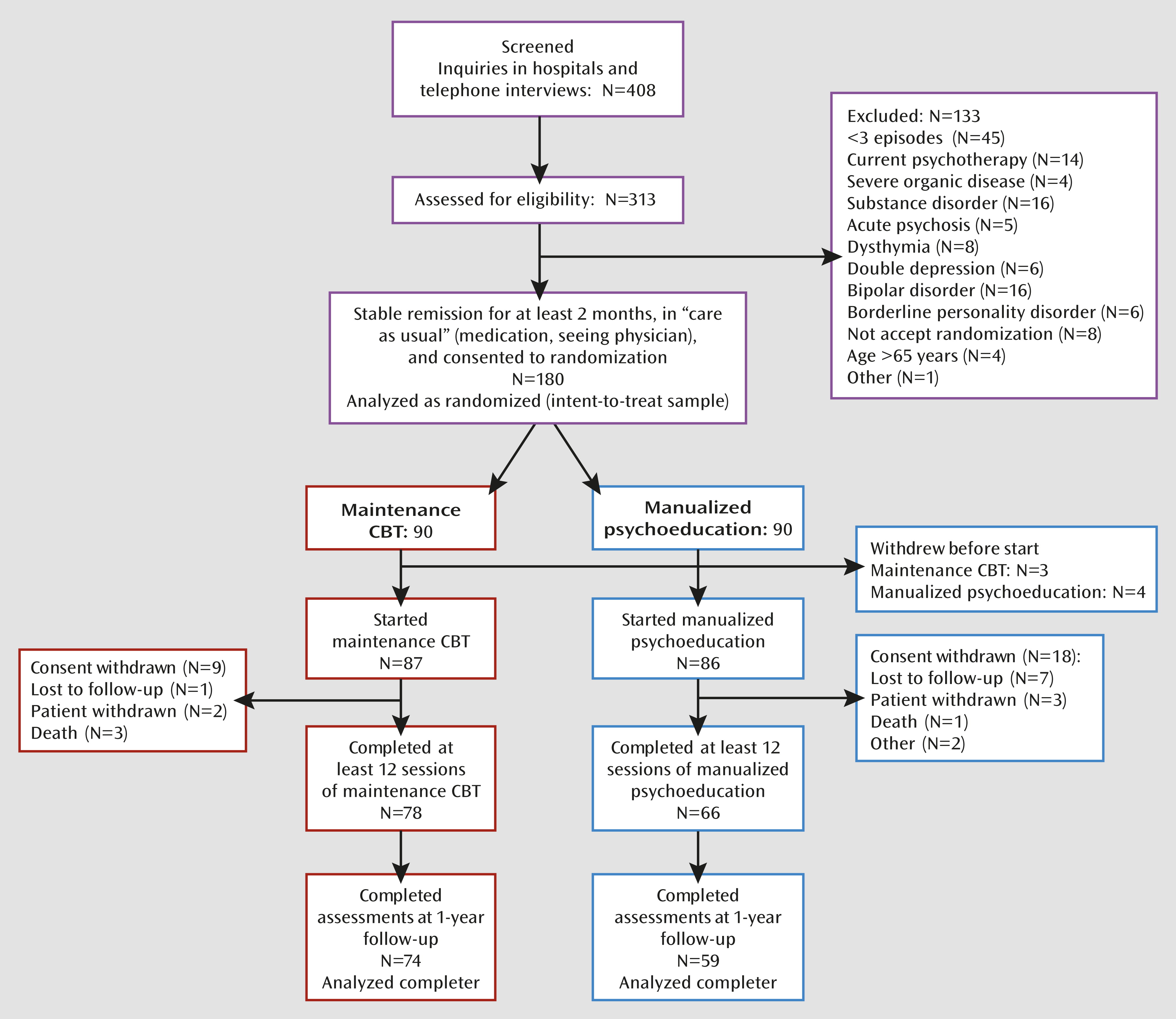
Of 408 patients who underwent initial screening, 313 were assessed for eligibility (
Figure 1). We excluded 133 individuals for the following reasons: a history of fewer than three depressive episodes, bipolar disorder, substance-related disorder, no history of major depressive episode but dysthymia, chronic major depressive disorder, borderline personality disorder, acute psychosis, severe organic disease, current psychotherapy, or age above 70 years. Eight patients did not accept random treatment assignment.
Eighteen patients were not fully remitted when assessed for eligibility, and an additional four patients relapsed during the baseline 2-month screening interval. For these patients, the baseline interval was extended until the patients achieved stable remission for at least 2 months. A final sample of 180 patients was randomly assigned to maintenance CBT or manualized psychoeducation.
Of 180 patients, 46 (25.6%) had discontinued the protocol by the 1-year follow-up. The difference in dropout rate at the 1-year follow-up between maintenance CBT (N=15, 8.3%) and manualized psychoeducation (N=31, 17.2%) was significant (χ2=7.5, df=1, p≤0.01). Two patients died by suicide, one after discontinuing maintenance CBT and one after completing manualized psychoeducation. In addition, two patients died from accidents not related to the study. Dropout of 31 patients, comprising 67% of the total attrition, occurred during the treatment phase. At least 12 sessions were completed by 144 patients (80%; maintenance CBT, N=78; manualized psychoeducation, N=66), who were then considered to be treatment completers. Of these, significantly more were in the maintenance CBT group than in the manualized psychoeducation group (χ2=5.0, df=1, p≤0.03).
Patient Characteristics
Participants’ demographic and clinical characteristics are summarized in
Table 1. Thirty-eight percent of the patients also met diagnostic criteria for one or more other current axis I disorders, and of these, the most frequent were social phobia (11.1%), panic disorder (9.4%), and specific phobia (8.3%). Twelve percent of the patients (N=22) met criteria for one or more personality disorders, primarily anxious (avoidant) personality disorder type (N=5, 22.7%). Overall, 75% of participants received antidepressant medication (of these, 37% received selective serotonin reuptake inhibitors; 30% received serotonin-norepinephrine reuptake inhibitors; 20% received tricyclics; 16% received tetracyclics; 5% received mood stabilizers; 3% received norepinephrine reuptake inhibitors; and 2% received monoamine oxidase inhibitors).
The two treatment groups did not differ significantly in any of the demographic or clinical variables except history of psychiatric hospitalization. Patients in the maintenance CBT group had significantly more inpatient treatments than those in the manualized psychoeducation group.
Relapse and Recurrence
Based on the randomized total sample, Cox regression analysis indicated that the time to relapse or recurrence of major depressive episode did not differ between treatment conditions, indicating no significant difference in risk status. The median time to relapse or recurrence of major depressive episode, from randomization, was 607 days for maintenance CBT and 531 days for manualized psychoeducation. The relapse rate after a 1-year follow-up (patients had then been in the study for 21 months) was not significantly different between maintenance CBT (46/90, 51%) and manualized psychoeducation (54/90, 60%). A post hoc analysis revealed similar results when patients who discontinued the study were considered as censored at the time of dropout, independent of the reason for leaving.
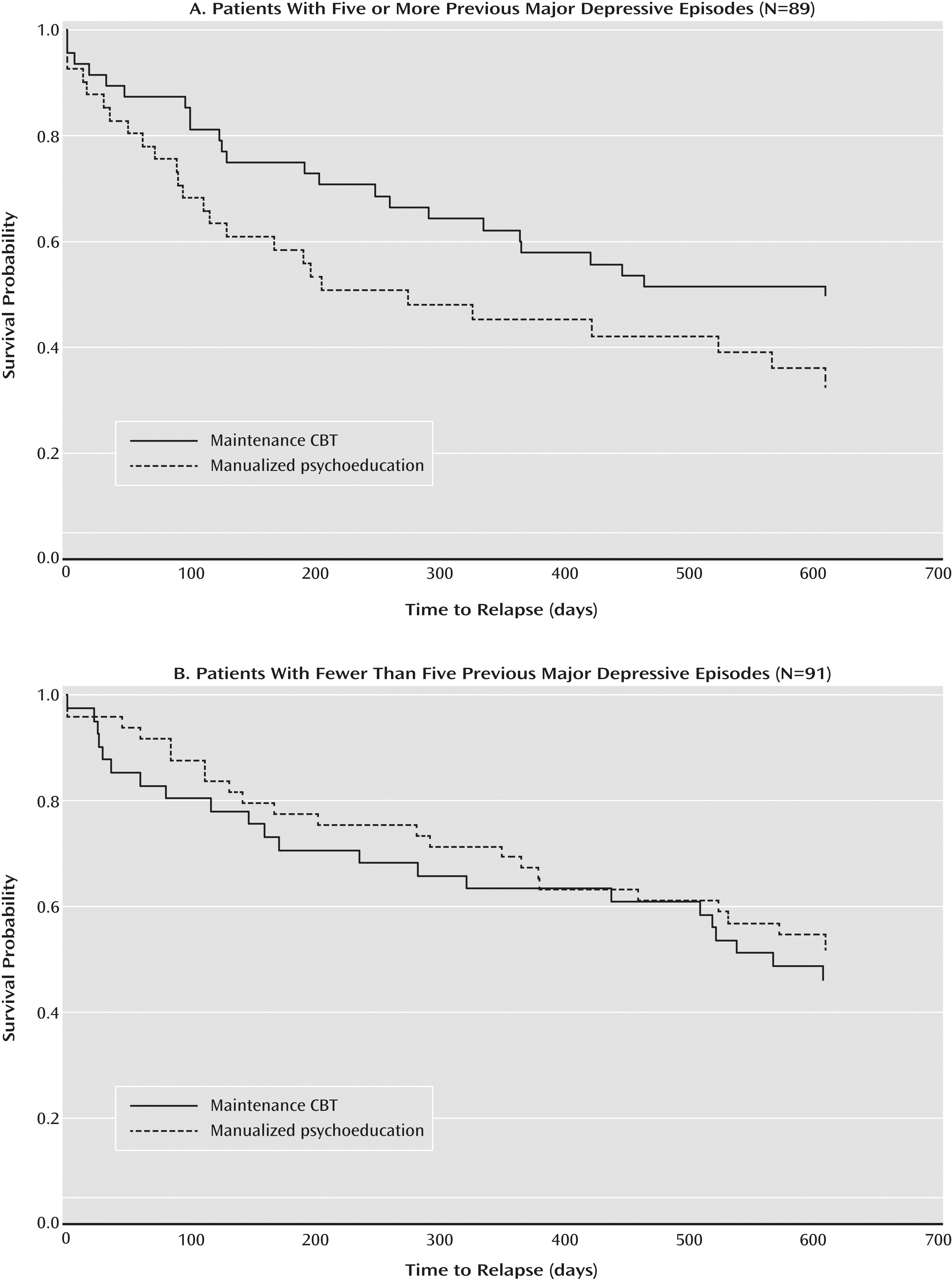
The interaction between intervention group and number of previous episodes (<5 or ≥5) was significant (log-rank χ
2=6.73, df=3, p≤0.02). Within the subsample of patients with five or more previous episodes, a significant difference was observed between treatment conditions (log-rank χ
2=5.36, df=1, p≤0.02). As depicted in
Figure 2A, patients in maintenance CBT had a significantly lower relapse rate (24/48, 50%) than patients in manualized psychoeducation (30/41, 73.2%). The hazard ratio associated with the comparison of maintenance CBT with manualized psychoeducation was 0.622 (95% CI=0.356–0.850), indicating a 38% reduction in relapse risk for maintenance CBT relative to manualized psychoeducation. In contrast, we observed no significant difference for patients with fewer than five episodes (
Figure 2B) in the time to relapse or recurrence of major depressive episode between treatment conditions or in the rate of recurrence at 1-year follow-up.
We also examined changes in the use of antidepressant medication during the trial and its impact on the frequency of relapses or recurrences. No significant differences were observed between maintenance CBT and manualized psychoeducation in the use of antidepressants at baseline (maintenance CBT, 75%; manualized psychoeducation, 74%), during treatment phase (months 0–9: maintenance CBT, 79%; manualized psychoeducation, 76%) or during the 1-year follow-up (maintenance CBT, 72%; manualized psychoeducation, 66%). In addition, we observed no significant main effect or interaction effect of medication with treatment condition on the relapse rates. Furthermore, with respect to additional treatments during follow-up, we observed no significant difference between treatment conditions (maintenance CBT, 11 of the completers [14.9%; seven for psychological treatment and four for inpatient treatment]; manualized psychoeducation, 11 patients [18.6%; nine for psychological treatment and two for inpatient treatment]).
Additionally, Cox regression models were fitted exploring potential effects of other factors that might moderate treatment outcome. However, we found neither a significant main effect of any of these factors (including residual baseline symptoms, unstable remission during baseline, comorbidity with anxiety disorders, comorbidity with personality disorders, age at onset, or gender), nor any interaction effects of these predictors with treatment. Finally, to investigate possible changes in depressive symptoms over time, we computed a mixed-effects model including time and time-by-treatment interaction as factors and HAM-D score as the dependent variable. We observed a significant effect of time (F=3.23, df=7, p<0.02) and a nonsignificant time-by-treatment interaction (F=1.43, df=7, p<0.086). However, for the patients with five or more previous major depressive episodes, we observed a significant effect of time (F=2.39, df=7, p<0.021) and of time-by-treatment interaction (F=2.13, df=7, p<0.046). The mean scores indicated slight increases from baseline to treatment termination, a decrease after termination of treatment, and increases over follow-ups. However, the mean scores were at a low level, never exceeding a HAM-D score of 5.1.
Discussion
Our main objective in this study was to test the efficacy of maintenance CBT for patients with recurrent depression who had achieved stable remission at the time of entry into the study protocol. To control for nonspecific factors, we compared the outcome of maintenance CBT with an active control condition, manualized psychoeducation. Within 1 year after end of treatment, no significant differences were observed between conditions with respect to time to first relapse or the prevention of recurrence of a major depressive episode. However, we saw a significant interaction between intervention and number of previous episodes. In patients with five or more previous episodes, maintenance CBT was significantly superior to manualized psychoeducation in preventing recurrences of depressive episodes, whereas we saw no outcome differences in patients with three or four previous episodes.
This pattern of results is in line with previous studies demonstrating significant treatment effects only in subsamples of patients with higher numbers of previous episodes (
10–
12). Thus, high-risk patients in particular may have benefited from specific elements of maintenance CBT by reducing cognitive vulnerability factors for recurrent depression, such as ruminating, negative attributions and memories (
28,
29), and dysfunctional beliefs (
30), or by maintaining positive emotions when experiencing stress (
8). However, other studies (
31) have not reported this effect of number of previous episodes on outcome for interpersonal psychotherapy.
Because there is evidence that patients may also benefit significantly from attention, advice, and support (
32), we added a structured psychoeducational program (manualized psychoeducation) to treatment as usual in contrast to other studies that control for routine psychiatric care. A recent meta-analysis (
18) established that even less structured types of psychoeducation significantly reduce the acute symptoms of depression. Thus, although manualized psychoeducation may have resulted in a protective effect equal to that of maintenance CBT, at least in patients with a moderate risk of recurrence, the superiority of maintenance CBT in patients with greater risk of recurrence is not exclusively attributable to interpersonal attention, emotional support, or information.
The internal validity of our trial is established by a high level of treatment integrity (
23,
24). To strengthen external validity, both treatments were implemented at several study sites, including psychiatric and psychological outpatient clinics. In addition, treatments were delivered in an individual setting over 8 months, which is representative of outpatient treatment for patients with remitted recurrent depression.
However, there is some evidence that the impairment level of the patients was higher than in most other studies, as indicated by a larger mean number of previous episodes than in other studies (
10,
15) and a higher proportion of patients using antidepressant medication (
10,
13). Although our study sample may have differed from those in other studies, the treatment effects were equivalent to most previous studies, as indicated by risk reduction and relapse rates (
10–
15,
28). Thus, there is some evidence that maintenance CBT in our study performed as well as comparable treatments for relapse prevention in previous studies.
This study has several limitations. First, our design did not include a no-treatment or a treatment-as-usual-only control condition, as several other studies have done (
8–
11). However, our choice to use a control condition that included active elements, such as patient education and supportive interventions, may add important information to the current status of research. Second, we did not control for differences between participants in both treatment conditions with respect to their preferences for pharmacological or psychological treatments. Thus, it is possible that patients who had received psychotherapy before were dissatisfied with being randomly assigned to the manualized psychoeducation condition. Although the number of patients who declined to start treatment was not significantly different between groups, we cannot rule out significant differences with respect to treatment expectations. Third, we did not standardize concomitant pharmacological treatment. Although an individual adjustment of pharmacotherapy is recommended for maintenance treatment (
33), and we saw no evidence of a significant effect on the course of recurrences in our sample, differential fluctuations in use or dosage of medication in both treatment conditions may have influenced the results. Fourth, we cannot rule out the possibility that the amount of attention was the effective component in maintenance CBT in comparison to manualized psychoeducation. Maintenance CBT patients received 16 sessions of 45–50 minutes each, while manualized psychoeducation patients received 16 sessions of 15–20 minutes each. This discrepancy in time spent with a patient represents a typical treatment-related feature but confounds our conclusion about outcome-relevant elements of maintenance CBT. Fifth, our therapists were comparatively young, and most of them were at the beginning of their clinical career. This may have limited the outcome of maintenance CBT in particular. More experienced clinicians are expected to have a higher level of general skills to adapt techniques to patients with recurrent depression.
In summary, our findings confirm previous results indicating that maintenance CBT may be efficacious in preventing relapse by reducing risk in patients who have experienced several previous depressive episodes. To the best of our knowledge, this is the first study to demonstrate the superiority of maintenance CBT to a nonpharmacological active control condition, indicating that intervention effects among patients with five or more previous major depressive episodes may be attributable to specific components of our maintenance CBT. Furthermore, this study achieved a high level of external validity, since treatment setting, sample characteristics, and therapist competence corresponded to clinical practice in routine care, which suggests a good generalizability of our findings. However, in order to evaluate whether patients can expect a complete prevention of future episodes, long-term studies that follow patients over several years are needed.
Acknowledgments
The authors thank Susann Taeger, Berit Wenda, Thomas Vieweg, Gregor Peikert, Katrin Rabisch, Jan Schönebaum, Regina Arnold, Ursula Fritz, Andreas Debus, Gundel Löhn, Dietmar Kohlhepp, Bernhard Wirtz, Martina Oelichmann, Susanne Wiesmann, Anna Konstantina Richter, Burkard Glaab, and Simone Matulis. They also thank their colleagues who served as maintenance CBT or manualized psychoeducation study therapists, as study psychiatrists, or as project interviewers. Rolf Meinert (IZKS) provided statistical planning for the study.