A Trial of Prazosin for Combat Trauma PTSD With Nightmares in Active-Duty Soldiers Returned From Iraq and Afghanistan
Abstract
Objective
Method
Results
Conclusions
Method
Participants
Inclusion and Exclusion Criteria
Randomization and Study Drug Titration
| Men | Women | |||
|---|---|---|---|---|
| Week | Morning Dose (mg)a | Bedtime Dose (mg) | Morning Dose (mg)a | Bedtime Dose (mg) |
| Week 1 | ||||
| Days 1 and 2 | 1 | 1 | ||
| Days 3–7 | 2 | 2 | ||
| Week 2 | 1 | 4 | 1 | 2 |
| Week 3 | 2 | 6 | 1 | 4 |
| Week 4 | 2 | 10 | 2 | 6 |
| Week 5 | 5 | 15 | 2 | 10 |
| Week 6 | 5 | 20 | ||
Assessments
Results
| Treatment Condition | ||||
|---|---|---|---|---|
| Characteristic | Prazosin (N=32) | Placebo (N=35) | ||
| Mean | SD | Mean | SD | |
| Age (years) | 30.0 | 6.6 | 30.8 | 6.5 |
| Educationa (years) | 13.3 | 1.9 | 13.0 | 2.1 |
| Combat Experiences Scale score | 10.9 | 3.8 | 11.9 | 3.6 |
| Number of deployments | 2.6 | 4.0 | 1.9 | 1.2 |
| N | % | N | % | |
| Male | 26 | 81 | 31 | 89 |
| Race/ethnicity | ||||
| African American | 4 | 13 | 5 | 14 |
| Asian | 1 | 3 | 0 | |
| Caucasian | 21 | 66 | 21 | 60 |
| Hispanic | 5 | 16 | 3 | 9 |
| Native American | 0 | 2 | 6 | |
| Other | 1 | 3 | 4 | 11 |
| Marital status | ||||
| Married | 19 | 59 | 26 | 74 |
| Widowed | 1 | 3 | 0 | |
| Separated/divorced | 8 | 25 | 5 | 14 |
| Never married | 4 | 13 | 4 | 11 |
| Major depression | 11 | 34 | 15 | 43 |
| Maintained on any antidepressant | 10 | 31b | 14 | 40c |
| Maintained on SSRI | 7 | 22 | 13 | 37 |
| Treatment Group | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Prazosin (N=32)b | Placebo (N=35)b | Difference in | ||||||||||
| Behavioral Outcome | Baseline | Week 15 | Baseline | Week 15 | Change From Baselinec | t | p | |||||
| Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | |||
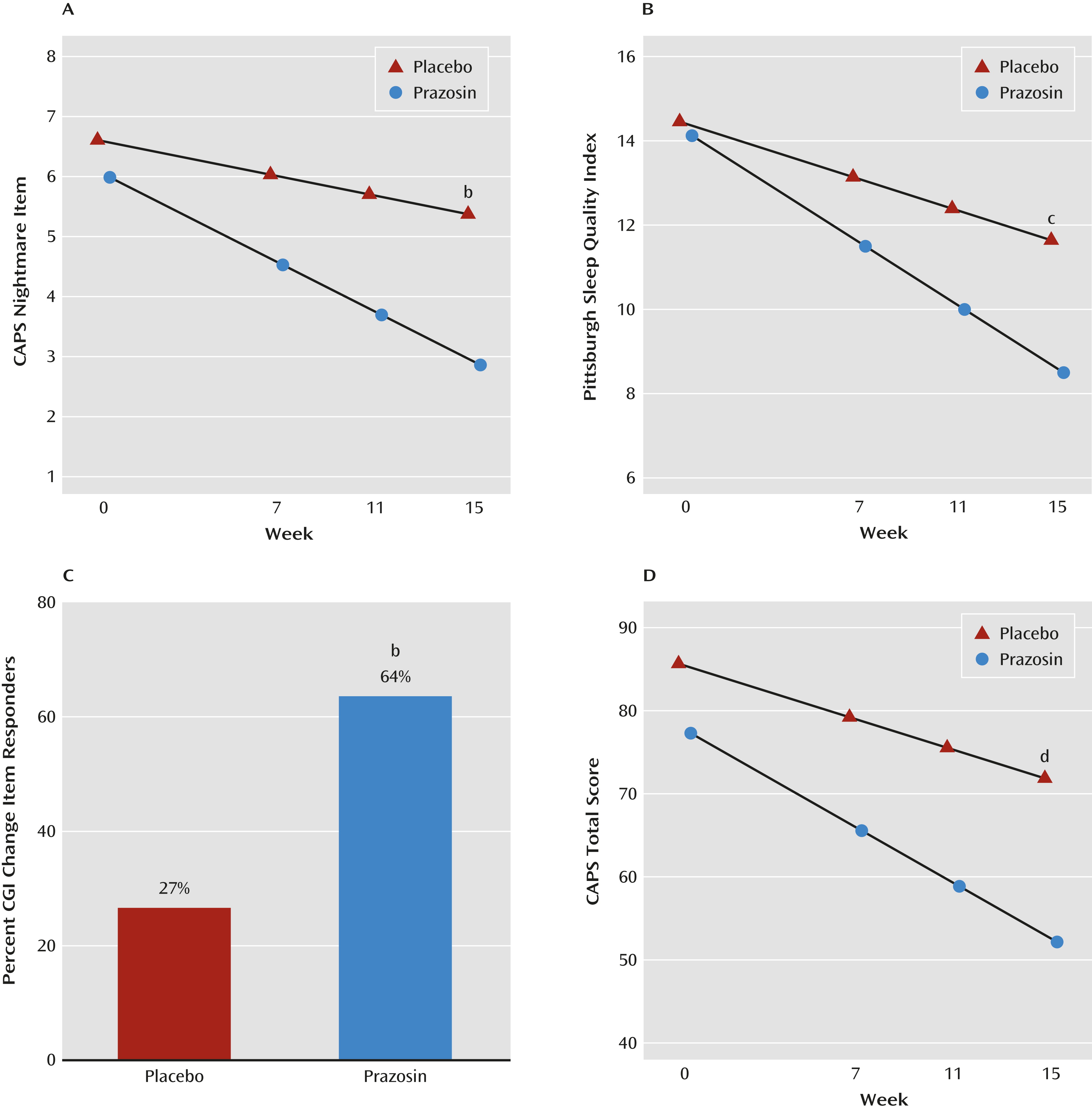
| CAPS nightmare item | 6.0 | 5.4, 6.6 | 2.9 | 2.2, 3.5 | 6.6 | 6.0, 7.2 | 5.4 | 4.8, 6.0 | 1.9 | 1.0, 2.8 | 4.06 | <0.001 |
| Pittsburgh Sleep Quality Index | 14.1 | 12.8, 15.5 | 8.5 | 7.1, 9.9 | 14.5 | 13.2, 15.7 | 11.6 | 10.3, 13.0 | 2.8 | 0.9, 4.7 | 2.98 | 0.003 |
| Clinical Global Impressions Scale change item | 2.3 | 1.8, 2.7 | 3.2 | 2.8, 3.6 | 0.9 | 0.3, 1.5 | 3.13 | 0.003 | ||||
| CAPS total score | 77.3 | 69.1, 85.5 | 52.2 | 43.8, 60.5 | 85.7 | 78.0, 93.3 | 71.9 | 63.9, 79.8 | 11.3 | 2.0, 20.7 | 2.39 | 0.02 |
| CAPS total score without nightmare item | 71.3 | 63.5, 79.1 | 49.3 | 41.3, 57.3 | 79.0 | 71.7, 86.4 | 66.5 | 58.9, 74.1 | 9.5 | 0.7, 18.3 | 2.12 | 0.04 |
| CAPS reexperiencing cluster | 22.3 | 19.8, 24.7 | 15.5 | 13.0, 18.0 | 25.1 | 22.7, 27.4 | 20.6 | 18.2, 23.1 | 2.3 | –1.2, 5.8 | 1.31 | 0.19 |
| CAPS avoidance cluster | 26.8 | 22.6, 31.0 | 18.2 | 13.9, 22.5 | 29.9 | 25.9, 33.8 | 24.7 | 20.6, 28.8 | 3.5 | –0.3, 7.3 | 1.81 | 0.07 |
| CAPS hyperarousal cluster | 28.2 | 25.7, 30.6 | 18.3 | 15.8, 20.8 | 30.7 | 28.4, 33.0 | 26.2 | 23.8, 28.7 | 5.4 | 1.9, 8.9 | 3.05 | 0.003 |
| Hamilton Depression Rating Scale | 11.9 | 9.5, 14.3 | 10.0 | 7.5, 12.5 | 14.7 | 12.4, 17.0 | 14.7 | 12.3, 17.1 | 2.0 | –0.8, 4.8 | 1.39 | 0.17 |
| Patient Health Questionnaire–9 | 12.1 | 9.9, 14.3 | 7.2 | 4.9, 9.4 | 14.7 | 12.6, 16.8 | 11.6 | 9.5, 13.8 | 1.8 | –0.5, 4.2 | 1.53 | 0.13 |
| Blood pressure (mmHg) | ||||||||||||
| Supine systolic | 126 | 123, 130 | 128 | 124, 131 | 126 | 123, 129 | 127 | 124, 130 | 0.1 | –4.1, 4.2 | 0.04 | 0.96 |
| Supine diastolic | 80 | 77, 83 | 81 | 78, 84 | 81 | 79, 84 | 82 | 79, 85 | –0.6 | –4.3, 3.2 | –0.29 | 0.78 |
| Standing systolic | 123 | 120, 126 | 124 | 120, 128 | 125 | 121, 128 | 124 | 121, 128 | –1.3 | –6.5, 3.8 | –0.51 | 0.61 |
| Standing diastolic | 82 | 79, 85 | 83 | 80, 86 | 84 | 81, 86 | 84 | 81, 87 | –0.9 | –4.8, 3.0 | –0.46 | 0.64 |
Discussion
Footnote
Supplementary Material
- View/Download
- 67.74 KB
References
Information & Authors
Information
Published In
History
Authors
Funding Information
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBLogin options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).

