In Denmark and other European countries, longer-term psychoanalytic psychotherapy has been widely practiced as a treatment for eating disorders. However, research has focused on cognitive-behavioral therapy (CBT), which has proven efficacious as a treatment for bulimia nervosa in several randomized controlled studies (
1–
3). Nevertheless, since most bulimia patients remain symptomatic following this treatment (
4), there is a need to develop alternative treatment approaches for this disorder.
It has been proposed that a central feature of bulimia nervosa is the inability to tolerate and regulate affective experience and that the bulimia symptoms serve as an attempt to avoid negative affect (
5–
7). Because a general aim of psychoanalytic psychotherapy is to increase the capacity to recognize and tolerate affects (
8), it was hypothesized that psychoanalytic psychotherapy would result in a reduction of binging and purging through the facilitation of heightened affect tolerance and insight into the psychological function of the symptoms. Accordingly, the purpose of the present study was to test the efficacy of a longer-term psychoanalytic psychotherapeutic treatment specifically designed for patients with bulimia nervosa (
9) by comparing it with the “enhanced” version of the original CBT (
10).
Studies of psychotherapy for bulimia nervosa have established that interpersonal psychotherapy is as effective as CBT but slower to operate (
11–
13). Two studies of psychodynamically oriented treatments have been conducted (
14,
15), but these treatments have been short- or medium-term forms. To our knowledge, no studies of longer-term psychoanalytic psychotherapy have been conducted. The “enhanced” variant of CBT has shown promising results in several studies (
16–
19), but it has not yet been tested in a study exclusively focused on patients with bulimia nervosa.
We compared the treatments using the form in which they are usually implemented, despite the disparity in number of sessions and length of treatment. The main hypothesis was that the percentage of patients with neither binge eating nor purging episodes within the last 28 days would be higher in the psychoanalytic psychotherapy condition than in the CBT condition after 5 months of therapy, at the end of each treatment (5 months after the start of CBT and 2 years after the start of psychoanalytic psychotherapy), and 2 years after the start of each treatment.
Method
Design
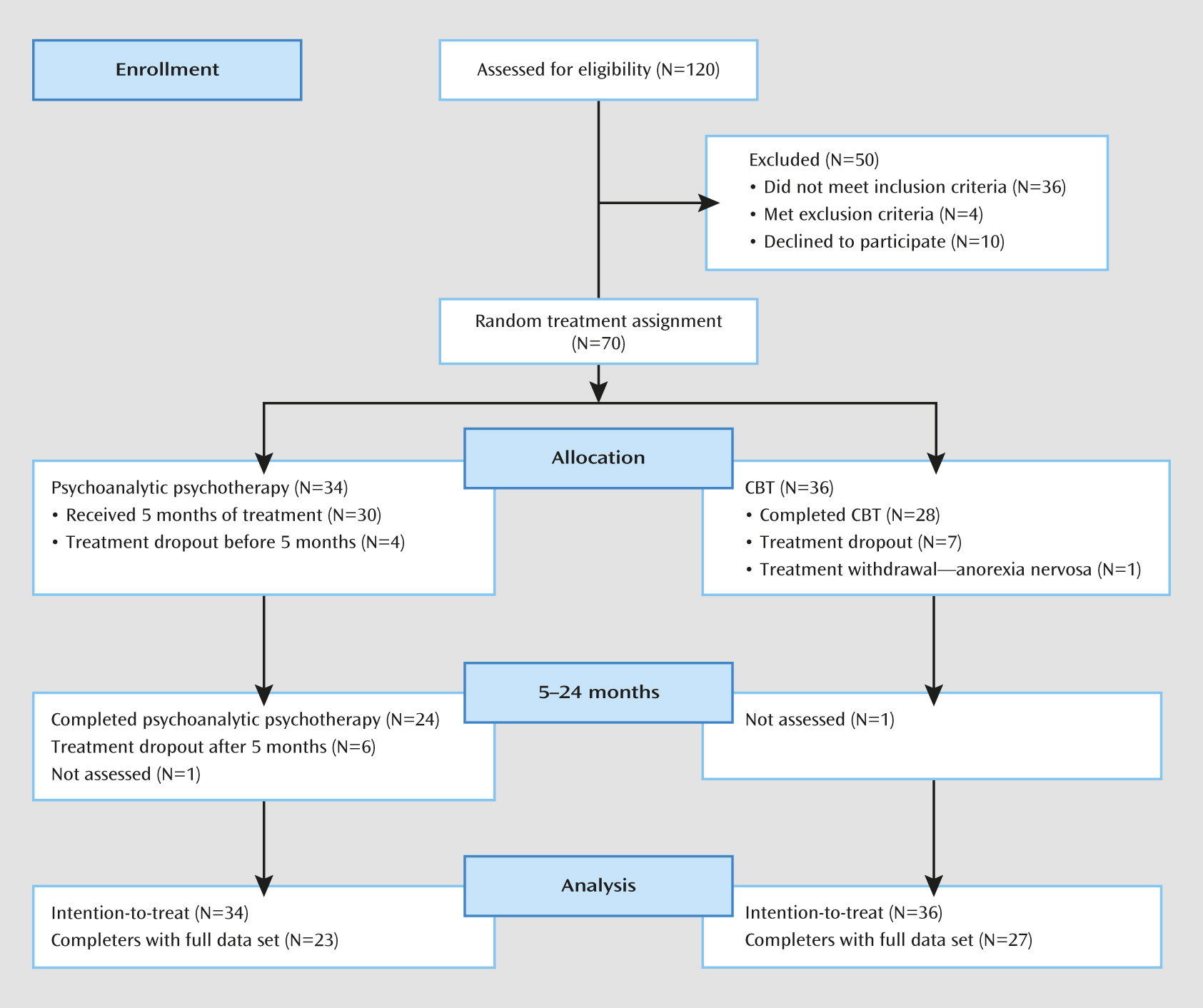
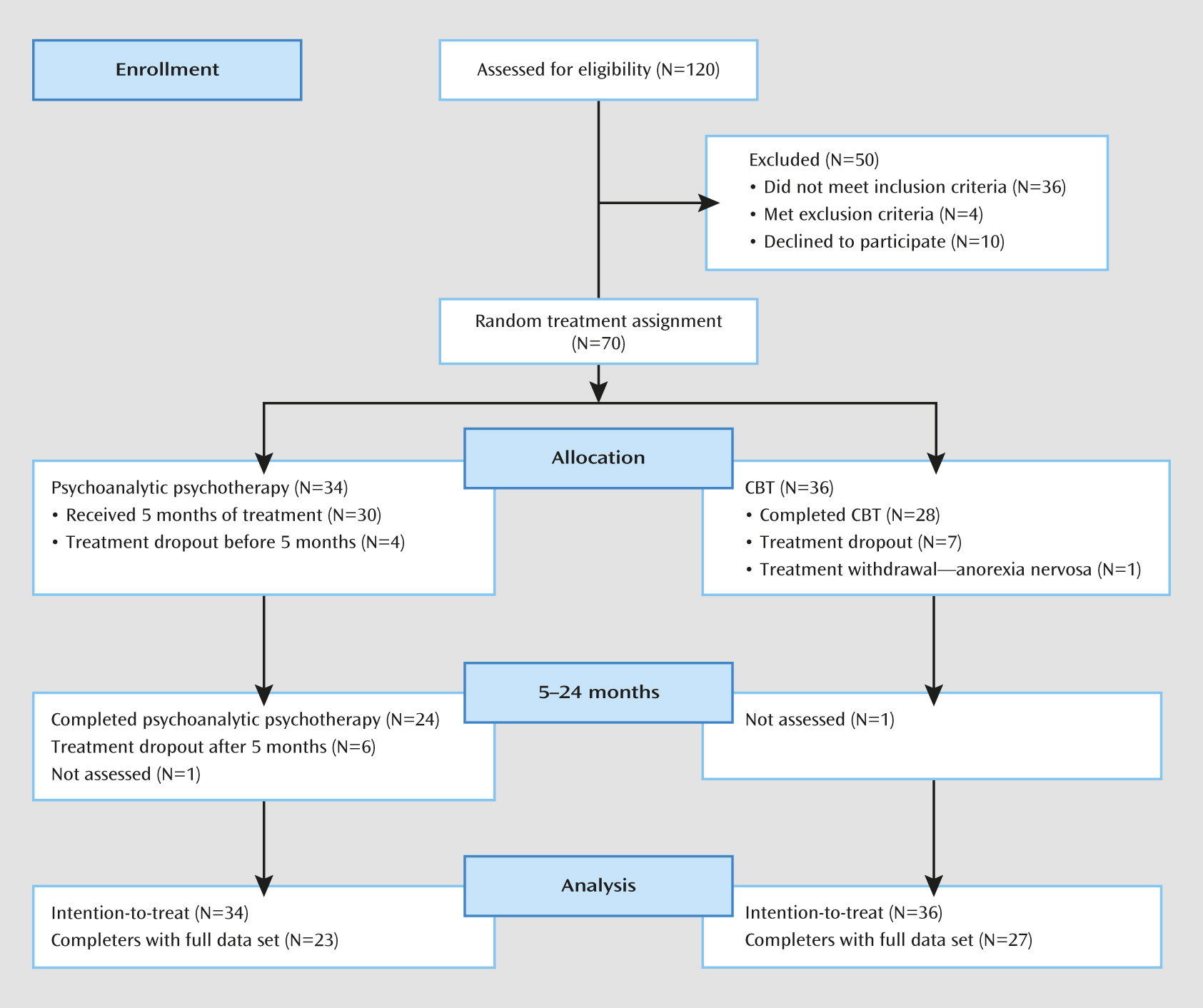
We conducted a randomized controlled trial in which 70 patients with bulimia nervosa were randomly selected to 2 years of weekly psychoanalytic psychotherapy or 20 sessions of CBT delivered over 5 months. We used a randomized block design with a block size of four and a 1:1 allocation ratio, the strata being the need for ongoing psychopharmacological treatment and the diagnosis of a personality disorder. The randomization was conducted using sequentially numbered envelopes by an independent researcher who had no involvement in any other aspects of the study. The study protocol was submitted to the Research Ethics Committee for the Capital Region of Denmark, who decided that it did not require ethical approval.
Recruitment
The study took place in a university outpatient clinic. The participants were recruited by advertisements and by referrals from local clinics. There was an initial telephone-based screening interview followed by a detailed assessment interview with those participants who appeared eligible, which confirmed the participant’s eligibility and provided detailed written and oral information about the trial. Those participants who were eligible to take part and who gave written informed consent then underwent the pretreatment baseline assessment. The remaining individuals were referred for alternative forms of treatment. The participant flow through the study is depicted in
Figure 1.
The inclusion criteria were age at least 18 years, being available for the duration of the longer of the two treatments, and meeting DSM-IV criteria for bulimia nervosa. The exclusion criteria were severe physical and psychiatric conditions that would interfere with treatment (e.g., psychosis), pregnancy, current psychotherapeutic treatment, and difficulty speaking or understanding Danish. Individuals already receiving psychopharmacological treatment as well as individuals meeting ICD−10 criteria for moderate or severe depression but who were otherwise considered eligible for the trial were referred to a consulting psychiatrist. When a stable dose of medication had been reached, the assessment procedure was continued. Patients in psychopharmacological treatments were monitored regularly by the consulting psychiatrist. Patients were withdrawn from the trial if their physical health became a cause for concern.
Treatments
Psychoanalytic psychotherapy.
This treatment was developed by the first two authors specifically for people with bulimia nervosa (
9). It involves weekly 50-minute sessions over 2 years (mean number of sessions in non-dropout cases, 72.3; SD=10.6; range=42–86; N=24). The treatment is based on the assumption that bulimic symptoms are rooted in a need to ward off inner feeling states and desires (
5) and in difficulties acknowledging and regulating such inner states (
20). Accordingly, the therapy aims to increase the capacity to reflect on and tolerate affective experience and to facilitate insight into the mechanisms hiding unconscious and disavowed aspects of the patient (
8). It is characterized by a nondirective approach where the patient is invited to talk as freely as possible, a focus on the therapeutic relationship, and involvement of the patient in a mutual reflection on the function of and the circumstances triggering the symptoms of the disorder (
21). The bulimic symptoms are not necessarily discussed in every session, but the therapist assists the patient in understanding possible connections between the way that he or she eats and his or her affective state. The treatment consists of three phases: an initial phase focusing on establishing the therapeutic frame and alliance and addressing the bulimic symptoms, the work phase where additional attention is directed toward the transference relationship, and the termination phase. The treatment guide is available from the first author (in either Danish or English).
CBT.
The “enhanced” version of the original CBT for bulimia nervosa is characterized by increased focus on engagement, greater emphasis on the modification of concerns about shape and weight, and the development of skills to deal with setbacks. Although it is designed to be “transdiagnostic” in its scope (
22), it can be used with patients with a specific eating disorder such as bulimia nervosa. We used the focused form of the treatment, which concentrates exclusively on modifying the patient’s eating disorder psychopathology. The treatment comprises 20 50-minute sessions that are preceded by one 90-minute preparatory session and followed by one review session 20 weeks after treatment. The sessions are twice-weekly for the first 4 weeks, weekly for the next 10 weeks, and every 2 weeks over the final 6 weeks. A detailed treatment guide is available (
10).
Therapists
Two sets of therapists were used, one for each treatment. Psychoanalytic psychotherapy was provided by six female and two male clinical psychologists. On average, the therapists had 17 years of psychotherapeutic experience. All the therapists had at least 2 years of training in various psychoanalytic or psychodynamic treatment modalities, and all were supervised biweekly by the first and second authors, who devised the treatment (
9).
CBT was provided by one male and two female clinical psychologists and one female psychiatrist. On average, the therapists had 8 years of psychotherapeutic experience. All the therapists had completed a 1-year generic training in CBT, and all had participated in an initial 2-day training workshop in CBT given by the last author. The therapists were supervised biweekly via videoconferencing by the last author, who devised the treatment (
10,
22).
Assessment
The main assessment points were at baseline, after 5 months of treatment (coinciding with the end of CBT), and 19 months later (at the end of psychoanalytic psychotherapy). The assessments were conducted by trained psychologists who had no involvement with treatment and were blind to the patient’s treatment condition.
Eating disorder psychopathology was assessed using the Eating Disorder Examination interview, version 14.4 (
23), which was administered at baseline and 5 and 24 months after starting treatment. All interviews were recorded and subsequently consensus rated.
General psychopathology was assessed at baseline using the Present State Examination (
24). The Symptom Checklist-90-Revised (
25), the Beck Depression Inventory-II (
26), and the State-Trait Anxiety Inventory (
27) were also administered at baseline and 5, 12, 18, and 24 months after starting treatment.
Personality disorder status was assessed at baseline using the Structured Clinical Interview for DSM-IV Axis II Personality Disorders (
28). The interviews were conducted by trained psychologists, and all interviews were recorded and subsequently consensus rated by members of a study group comprising psychologists and an external psychiatric consultant.
Interpersonal functioning was assessed at pretreatment and 5, 12, 18, and 24 months after beginning treatment with the Inventory of Interpersonal Problems (
29).
Patients’ expectations of treatment outcome were rated before treatment randomization on a 5-point Likert scale. Adherence to CBT was assessed using a revised version of the Cognitive-Behavioral Therapy Treatment Protocol Adherence Scale (
30), a measure developed specifically for CBT for bulimia nervosa. This consisted of 20 items rated on a 7-point scale reflecting general aspects of therapy, phase-specific interventions, and the use of noncognitive behavioral techniques. Adherence to psychoanalytic psychotherapy was measured by the Adherence Scale for Psychoanalytic Psychotherapy for Bulimia nervosa (unpublished 2011 manuscript by S. Lunn et al.), a scale specifically developed for the present study. It was rated using the same scheme as the CBT adherence scale. Both adherence measures included three items designed to monitor the use of interventions characteristic of the opposite treatment modality. The adherence scales were completed by six graduate psychology students and a clinical psychologist who had participated in the development of the measures and served as the criterion rater. The students were trained for 30 hours. Before making the study ratings, they had to achieve acceptable levels of interrater reliability compared with the criterion rater (intraclass correlation [ICC] ≥0.60) on a subset of seven training cases for each therapy type (mean ICC was 0.79 for psychoanalytic psychotherapy [range, 0.73–0.89] and 0.73 for CBT [range, 0.62–0.86]). Subsequently, two treatments from each of the eight psychoanalytic psychotherapy therapists and four treatments from each of the four cognitive-behavioral therapists were randomly selected. Within each treatment, an early, middle, and late full session was rated. Accordingly, 96 sessions were rated, 48 from each therapy type. The mean scores of the respective measures were used for the data analyses.
Statistical Analysis
The funding of the trial permitted a sample size of only 70 patients. This sample size provided 80% power at two-sided p<0.05 to detect a difference of around 35% in proportions and an effect size of 0.70. As this sample size is small for a trial comparing two active treatments for bulimia nervosa (
13), the study was underpowered and subject to type II error.
The primary outcome variable was cessation of binge eating and purging, defined as no binge eating or purging over the previous 28 days. Because of the different lengths of the two treatments, three comparisons were made: status 5 months after beginning treatment (corresponding to the end of CBT), status 24 months after beginning treatment (corresponding to the end of psychoanalytic psychotherapy), and status at the end of CBT (i.e., after 5 months) compared with status at the end of psychoanalytic psychotherapy (19 months later).
Group comparisons for binary outcomes are presented as odds ratios with 95% confidence intervals. Group comparisons for secondary outcome measures are presented as estimated marginal means with 95% confidence intervals. Sample means and expectancy and adherence ratings for the two treatment groups were compared using t tests or Fisher’s exact tests. All primary outcome analyses were conducted by intention-to-treat using logistic regression, with treatment expectancy as covariate. Proportions of patients achieving a global Eating Disorder Examination score below one standard deviation above the community mean were compared by logistic regression, controlling in posttreatment analyses for initial global Eating Disorder Examination scores and treatment expectancy. Frequencies of binging and purging (both square root transformed) and values of the other secondary outcome measures were compared using mixed-effect model repeated measures analysis with time, treatment expectancy, personality disorder, psychopharmacological medication, baseline values of the variable × time, and therapy type × time specified as fixed effects and with random intercepts for patients. Categorical analyses were conducted with missing data accounted for by last observation carried forward. All analyses were repeated with data based on multiple imputations. None had a material effect on the overall pattern of results. All analyses were conducted using SPSS, version 20.
Results
Sample Characteristics
Patients were recruited between October 15, 2004, and April 17, 2008. The demographic and clinical characteristics of the sample are summarized in
Table 1. The majority of the patients were in their mid-20s and had eating disorder features for a mean of 12.3 years (SD=6.2). One-third had a history of anorexia nervosa and over half had received prior treatment for an eating disorder. The two treatment groups did not differ significantly on any of the baseline characteristics.
Treatment Expectancy and Adherence
The baseline expectancy ratings were high for both treatments and did not differ significantly (CBT: mean=4.14, SD=0.75; psychoanalytic psychotherapy: mean=4.10, SD=0.76; t=0.50, p=0.62). Among the participants randomly assigned to CBT, no significant differences in expectancy ratings for the two treatments were observed (CBT: mean=4.14, SD=0.72; psychoanalytic psychotherapy: mean=4.31, SD=0.58; t=−1.64, p=0.11). In the psychoanalytic psychotherapy condition, however, expectations for CBT (mean=4.15, SD=0.78) were significantly higher than those for psychoanalytic psychotherapy (mean=3.88, SD=0.88; t=2.06, p<0.05).
The global adherence ratings were high for both treatments (CBT: mean=4.59, SD=0.60; psychoanalytic psychotherapy: mean=4.98, SD=0.73) with particularly high scores on the items differentiating the two treatments (CBT: mean=6.64, SD=0.78; psychoanalytic psychotherapy: mean=6.45, SD=0.64).
Treatment Completion
In all, 34 patients were randomly selected for psychoanalytic psychotherapy and 36 for CBT. Twenty-four (70.6%) of the patients in psychoanalytic psychotherapy completed their 2 years of treatment, and 28 (77.8%) of the CBT patients completed their 5 months of treatment. Two of the patients in psychoanalytic psychotherapy were started on antidepressant medication during the treatment phase. During follow up, 11 of the CBT completers received additional treatment. Three of these patients were in psychiatric outpatient treatment for an eating disorder, one of whom was prescribed antidepressant medication. Eight patients received some form of psychotherapy. It is not known whether this additional psychotherapy was directed at the eating disorder or at other psychological difficulties.
Cessation of Binge Eating and Purging
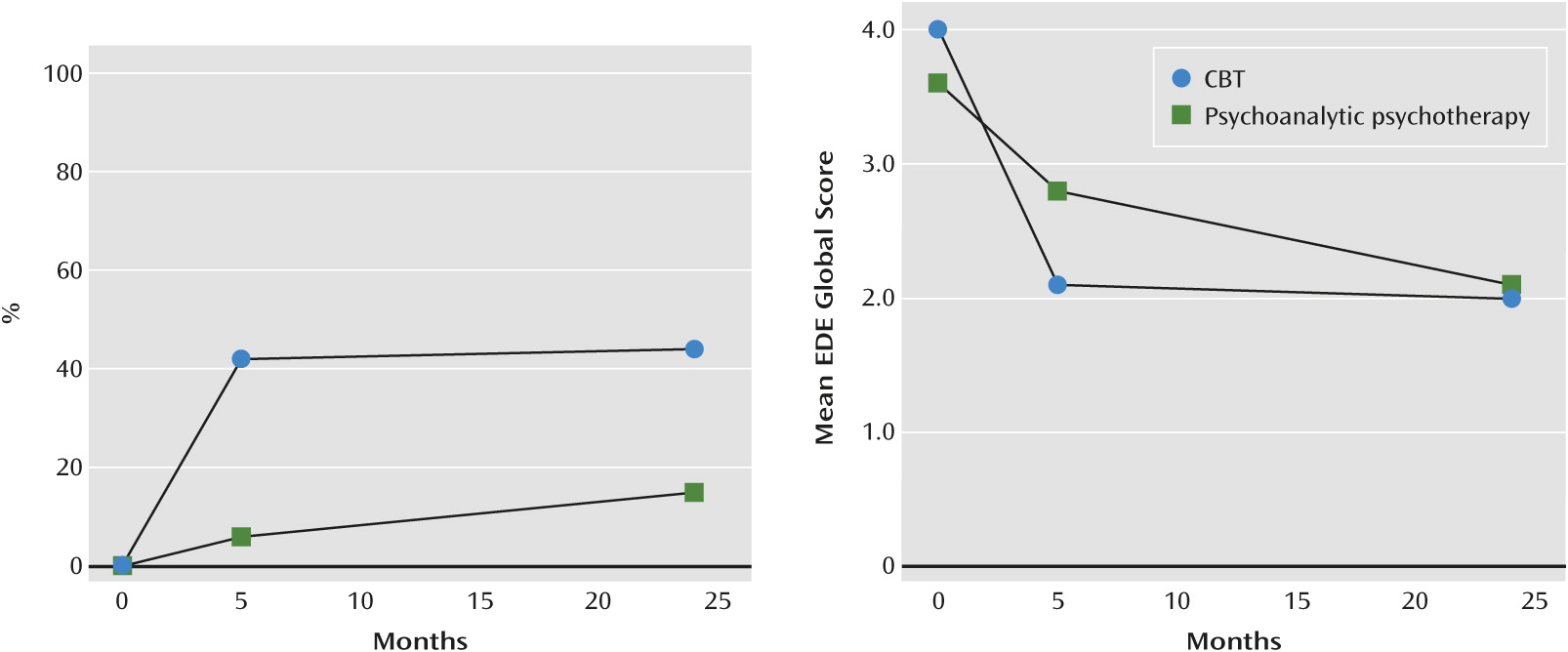
Both treatments resulted in an improvement in the patients’ state, although the improvement was greater among those who received CBT. At their respective endpoints, 15 (42%) of the patients in CBT had ceased to binge eat and purge compared with five (15%) of the patients in psychoanalytic psychotherapy (odds ratio=4.41; 95% CI=1.20–16.15; p=0.03). A marked difference was also observed in the time course of the response to the two treatments. This is depicted in
Figure 2. CBT had a rapid and marked effect whereas the effect of psychoanalytic psychotherapy was slower and more modest. At the 5-month assessment point, 42% (15/36) of the patients in CBT had stopped binge eating and purging compared with 6% (2/34) of those receiving psychoanalytic psychotherapy (odds ratio=13.40; 95% CI=2.45–73.42; p<0.01), and at the 2-year assessment point the cessation rates were 44% (16/36) and 15% (5/34), respectively (odds ratio=4.34; 95% CI=1.33–14.21; p=0.02). Of the 15 patients in CBT who were free from binge eating and purging at the end of treatment, 10 (66%) were binge and purge free at 24 months, while six who were binge eating and purging at month 5 had ceased to do so at month 24. The outcome of CBT completers who received additional treatment did not differ significantly from the outcomes of patients who did not, neither at the end of treatment nor 19 months later.
Changes in Eating Disorder and General Psychopathology
Substantial improvements were also observed in global eating disorder psychopathology (
Table 2). These improvements had occurred by the respective endpoints of the two treatments and to a similar extent (
Figure 2). However, the improvements took place more rapidly in the CBT group (time-by-treatment interaction for global Eating Disorder Examination score, p<0.01); after 5 months, the patients in CBT achieved lower (better) scores than patients in psychoanalytic psychotherapy, but the difference between the groups 2 years after starting treatment was not statistically significant.
A similar pattern was observed with regard to the other secondary outcome measures (
Table 2). Thus, while patients in CBT had significantly lower values after 5 months on all measures except BMI and state anxiety, after 2 years the significant differences remained only for number of binging and purging episodes. However, improvements occurred more rapidly in the CBT group for the majority of variables (time-by-treatment interaction for all measures except purging, BMI, and state and trait anxiety, p
<0.05). The proportion of patients achieving a global Eating Disorder Examination score below one standard deviation above the community mean did not differ between the two treatments at either 5 months or 2 years (
Table 3).
Discussion
The aim of this study was to compare a psychoanalytic psychotherapy designed specifically for the treatment of bulimia nervosa with the enhanced form of CBT for bulimia nervosa. The number of treatment sessions and the duration of treatment were markedly lower in CBT compared with psychoanalytic psychotherapy. The decision to compare two treatments of different lengths was made in order to strengthen the external validity of the study by conducting each treatment in a format that was in accordance with clinical practice. The therapists were supervised throughout the study, and their supervisors developed the two treatments in question. The data on therapist adherence indicate that the treatments were implemented well.
The results clearly indicate that CBT was more efficacious than psychoanalytic psychotherapy in the treatment of core bulimic symptoms. In the CBT group, 42% of patients were free from binging and purging at the end of treatment and 44% were free after 24 months. In contrast, 15% of the patients in psychoanalytic psychotherapy had ceased to binge and purge after 24 months of therapy. Both treatments had substantial effects on global eating disorder psychopathology and general psychopathology, but in general these improvements took place more rapidly in the patients in the CBT condition. The data do not indicate adverse effects of CBT in terms of symptom substitution.
The results are noteworthy for a number of reasons. First, the results are contrary to the frequently reported absence of significant differences in outcomes between two bona fide psychotherapeutic treatments (
31). Second, after 2 years the effect of psychoanalytic psychotherapy on global eating disorder psychopathology was apparently more substantial than its effect on binging and purging. This outcome suggests that psychoanalytic psychotherapy addresses issues relevant to patients with eating disorders but that more directive and behavioral interventions are needed to influence binge eating and purging.
Indeed, the most likely reason for the marked difference in the effects of the two treatments seems to be their different approach to the bulimic core symptoms. CBT is a symptom-focused treatment that is designed to produce a rapid reduction in the frequency of binge eating (
10), a change that is highly predictive of the patients’ eventual response (
32). In contrast, the psychoanalytic psychotherapy tested in this trial was designed as a nondirective therapy with no specific behavioral procedures directed at the control of binge eating. The more indirect approach to symptoms in psychoanalytic psychotherapy may be insufficient, because binge eating and purging can both be viewed as maladaptive coping strategies that provide an immediate, albeit short-term, relief from negative emotions (
5–
7). Accordingly, to enable the patient to let go of the symptoms, a directive approach providing concrete alternative problem-solving techniques may be needed.
The study has several limitations. Nonsignificant findings cannot be interpreted because of the small sample size. Another limitation is the fact that only the focused version of the CBT was tested (
10). Furthermore, the fact that CBT has been tested and revised extensively, whereas this is the first trial of the present version of longer-term psychoanalytic psychotherapy for bulimia nervosa, may have also contributed to the difference in outcome. Further testing of revised approaches to psychoanalytic psychotherapy (e.g., a more intensive therapy with two weekly sessions) might yield better results. Finally, while it was hypothesized that psychoanalytic psychotherapy would lead to symptom reduction through insight and an increased capacity for affect tolerance, the choice of cessation of binging and purging as the primary outcome variable for psychoanalytic psychotherapy, which has a more indirect focus on symptoms than CBT, may be debated.
With these reservations in mind, however, the results have two clear implications for the treatment of bulimia nervosa. First, CBT is the preferred treatment for the disorder when compared with the version of psychoanalytic psychotherapy tested in this trial. Second, at the 2-year follow-up, 56% of the patients in CBT still had episodes of binge eating and purging, 31% still met the diagnostic criteria for bulimia nervosa, and several patients received additional treatment during follow-up. Accordingly, further treatment developments are needed. One could be the continued development and extension of CBT. Another could be the development of a more structured and symptom-focused version of psychoanalytic psychotherapy, possibly augmented with cognitive and behavioral strategies (
33,
34). A diversified approach in which treatments are matched to certain subtypes of bulimia nervosa (
10,
35,
36) may also be of value.