We live in a literate world. In developed countries such as the United States, reading is taught starting in early school years, and reading ability increases progressively from grade school to high school to university. In developed countries, reading ability even as early as third grade is substantially related to future achievement in school, work, and family and societal roles (
1), while adult literacy levels are strongly related to income and occupational achievement (
2). Reading ability is also closely tied to the integrity of sensory brain systems, with strong visual and auditory (phonological) abilities needed for fluent reading of written information (
3–
5).
Over the years, deficits in early sensory processing ability have been increasingly well-documented in schizophrenia, involving both visual and auditory functions known to be related to reading ability (
6–
8). Moreover, while visual deficits appear to represent a trait component of the illness, auditory deficits develop during the years immediately surrounding illness onset, leading to significant declines in cognitive function (
9). Given sensory contributions to reading ability, the present study investigates the degree to which sensory dysfunction produces secondary impairments in reading ability.
Acquisition of reading skills during childhood requires the complex integration of visual and auditory functions. Because of this, many individuals have difficulty in initial acquisition of reading skills, a condition termed developmental dyslexia. For most individuals, however, once reading skills are acquired in childhood they remain intact into adulthood. Therefore, formal tests of the ability to fluently read passages of information (“connected text”) are rarely tested in adults. Instead, reading is typically assessed using single-word reading tests such as the Wide Range Achievement Test (WRAT) (
10), which assesses an individual’s ability to correctly pronounce irregularly spelled words such as “stalk,” “quarantine,” or “synecdoche.” Because of their irregularity, pronunciation of these words cannot be determined using standard phonological principles. Instead, the ability to pronounce these words correctly indicates prior exposure to them, which in turn reflects the complexity of reading material to which a person has been exposed. In schizophrenia, performance in single-word reading is typically preserved relative to other cognitive domains (
11–
13), leading to the tacit assumption that underlying passage reading abilities are relatively retained as well and that literacy is preserved. The present study, however, explicitly tests this assumption using tests drawn from the development reading literature.
In general, reading ability depends on two sets of interrelated processes. Visual processes permit individuals to accurately scan passages of text and are linked to function of the visual magnocellular system (
14–
16). Auditory phonological processes permit individuals to “sound out” words and are tied to auditory tonal discrimination abilities as reflected in the generation of mismatch negativity or other early event-related potential components (
17–
19). Different individuals use visual or phonological processes to different extents during reading and, in general, strengths in one set of processes can be used to compensate for weaknesses in the other. Patients with deficits in both sets of processes, however, show a “double-deficit” pattern associated with highly impaired reading ability (
20,
21).
For the present study, patients with schizophrenia were evaluated using several batteries that assess not only ability to use written materials but also underlying mechanistic processes. The Gray Oral Reading Test (
22), for example, assesses both fluency of reading (combined rate and accuracy) and comprehension to obtain an overall reading quotient. The Comprehensive Test of Phonological Processing (
23) provides separate indices of phonological awareness versus rapid naming ability and thus is useful for differentiating phonological, visual, or double-deficit subforms of dyslexia. The Woodcock-Johnson III Tests of Achievement (
24) assess a wide range of basic reading skills. The Nelson-Denny Reading Test (
25) uniquely provides grade equivalent performance levels through end of college (equivalent to 16th grade). At present, there is no gold standard assessment for reading skills. The above tests, therefore, were chosen to provide a comprehensive assessment.
In addition to reading ability, patients were assessed on measures of sensory function, including visual contrast sensitivity (
6), auditory tone-matching ability (
8,
26), and mismatch negativity (
9) as well as on more global outcome measures including personal and parental socioeconomic status (
27) and scores on the Independent Living Scales, which measure capacity for independent living (
28). General cognitive ability was assessed using the processing speed index of the WAIS-III (
29) and the working memory index of the Wechsler Memory Scale (WMS) (
30), which consistently capture the general cognitive deficits associated with schizophrenia (
31,
32).
In addition to a sample of 45 patients with schizophrenia, which represents our primary cohort, we also obtained reading scores from 19 patients who were considered at high clinical risk for schizophrenia and age-matched comparison subjects. Patterns of deficit were compared between patients and healthy comparison subjects and between the two patient groups. Given our findings of auditory and visual sensory-level dysfunction, we predicted that schizophrenia patients would display significant deficits in reading ability, and that these deficits would correlate with both impaired visual contrast sensitivity and auditory mismatch negativity generation.
Method
Participants
The primary sample consisted of patients meeting DSM-IV criteria for schizophrenia (N=37) or schizoaffective disorder (N=8) and similar-age comparison subjects (N=24) recruited at the Nathan S. Kline Institute for Psychiatric Research and affiliated institutions. All participants completed the Structured Clinical Interview for DSM-IV (
33) and met the following inclusion criteria: IQ≥85, native English speaking, absence of neurological impairment or current substance abuse or dependence, and near vision corrected to 20/32 (
Table 1). Patients had been ill an average of 16.8 years (SD=9.4) and were receiving antipsychotics at a mean daily dosage of 944.3 chlorpromazine equivalents (SD=702.7). Twenty-one patients (51%) were inpatients at the time of testing, whereas 20 (49%) were living in supervised residential care settings.
A second sample consisted of individuals (N=19) ages 12–30 years who were considered to be at high clinical risk for schizophrenia based on the Structured Interview for Prodromal Syndromes/Scale of Prodromal Symptoms (
34) and similar-age comparison subjects (N=41). Recruitment and ascertainment relied on clinician referrals, Internet resources, and the mailing of brochures. Exclusion criteria included any major medical or neurological disorder, significant risk of harm to self and others, an inability to speak English, and symptoms occurring solely in the context of substance intoxication or withdrawal. Additional exclusion criteria for healthy comparison subjects included any current axis I disorder within the past 2 years, as assessed by structured diagnostic interview, and any personal or familial (first-degree relative) history of psychosis. Because of time constraints, contrast sensitivity scores and mismatch negativity were not obtained in this sample.
The study was approved by the institutional review board associated with the New York State Office of Mental Health. Adult participants provided written consent after being informed of all study procedures, while minors provided assent, with written informed consent provided by a parent.
Instruments
Reading measures.
The full battery consisted of complete versions of the four test batteries described in the Introduction (
Table 2). The primary measure that was used to assess overall current (passage) reading level across analyses was the oral reading quotient of the Gray Oral Reading Test. Visual reading ability was assessed using an average of the rapid naming and alternative rapid naming measures in the Comprehensive Test of Phonological Processing, while phonological ability was assessed using an average of the phonological awareness and alternate phonological awareness scores.
Based on initial experience with these tests, we also developed a briefer battery consisting of a subset of tests that required only 45 minutes (
Table 2). Most, but not all, reading tests are normed with a mean of 100 and standard deviation of 15, permitting direct comparison to standard IQ scores. The Nelson-Denny Reading Test provides grade equivalent scores and has been validated through grade 16.
Clinical Measures
Neurocognitive.
Neurocognitive ability was assessed using the processing speed index of the WAIS-III.
Symptoms.
Ratings were obtained for patients using the Positive and Negative Symptoms Scale (PANSS) (
35). Mean scores were 72.0 (SD=13.6), 17.4 (SD=5.5), 18.7 (SD=4.5), and 36.6 (SD=8.8) for total, positive, negative, and general factors, respectively.
Functional.
Both individual and parental socioeconomic status were assessed using the Hollingshead Index (
27), which considers both education and occupational function (
Table 1). Functional cognition for patients was assessed using the problem-solving factor subscale of the Independent Living Scales (
36,
37). The mean score for patients was 41.7 (SD=11.7), reflecting, in general, the need for supervised living.
Sensory Measures
Auditory.
Auditory function was assessed using simple tone-matching and mismatch negativity paradigms, as previously described (
8,
9). Mismatch negativity recordings were obtained with a Biosemi system (Amsterdam, the Netherlands) using a standard 10-10 channel layout. Separate measures were obtained for pitch, duration, and intensity mismatch negativity at the FCz electrode using analysis approach and latency intervals (
9).
Contrast sensitivity.
Early visual processing was evaluated using contrast sensitivity (
6). Stimuli (0.5, 7, or 21 cycles/degree) were presented for 32 ms in a 3-down/1-up adaptive staircase method to determine detection threshold. Contrast sensitivity was calculated as 1/(detection threshold).
Statistical Analyses
Demographic characteristics between groups were analyzed with t tests and Mann-Whitney U tests as appropriate. Group differences on main dependent measures were analyzed with univariate or repeated-measures multivariate analysis of variance (MANOVA), with post hoc analyses by least significant difference. The relationship between measures was assessed using stepwise multiple regression, which yields measures for R2 change for successive steps of the model, as well as partial correlations (rp) for individual variables. Categorical analyses were performed using likelihood ratio chi-square. All statistical tests were performed using SPSS, version 20 (SPSS Inc., Chicago). All statistics are two tailed, with a preset alpha level for significance of p<0.05.
Results
Patients displayed highly significant impairments in reading relative to comparison subjects across all test batteries (F=6.70, df=18, 24, p<0.001) with an overall large effect size across batteries (mean d=1.6) (
Table 2). Effect sizes for summary measures such as the oral reading quotient of the Gray Oral Reading Test (d=2.3) or the broad reading measure of the Woodcock-Johnson (d=2.8) were substantially larger than deficits in either general cognitive measures or sensory measures alone (
Table 3).
On subscales, patients displayed significantly greater impairment in reading fluency than reading comprehension in both the Gray Oral Reading Test (group × subtest: F=21.6, df=1,67, p<0.0001) and the Woodcock-Johnson (group × test: F=21.6, df=1,41, p<0.0001), which provide parallel measures (
Table 2). On the Comprehensive Test of Phonological Processing, phonological processing scores in schizophrenia patients were strongly different from comparison subjects (mean scaled score=74.5 [SD=13.7] compared with 89.1 [SD=14.2], t=4.17, df=45, p<0.0001, d=1.0), as were visual reading scores (mean scaled score=79.8 [SD=14.1] compared with 103.2 [SD=14.9], t=5.21, df=45, p<0.0001, d=1.6). As a result, there was a strongly significant main effect of group (F=15.9, df=1, 45, p<0.001), whereas the group-by-test interaction was not significant (F=2.18, df=1, 45, p=0.15). In order to assess the degree to which reading impairments reflected an acquired dyslexia (i.e., regression in performance from a prior nonimpaired state) compared with neurodevelopmental dyslexia in schizophrenia, we performed two sets of analyses.
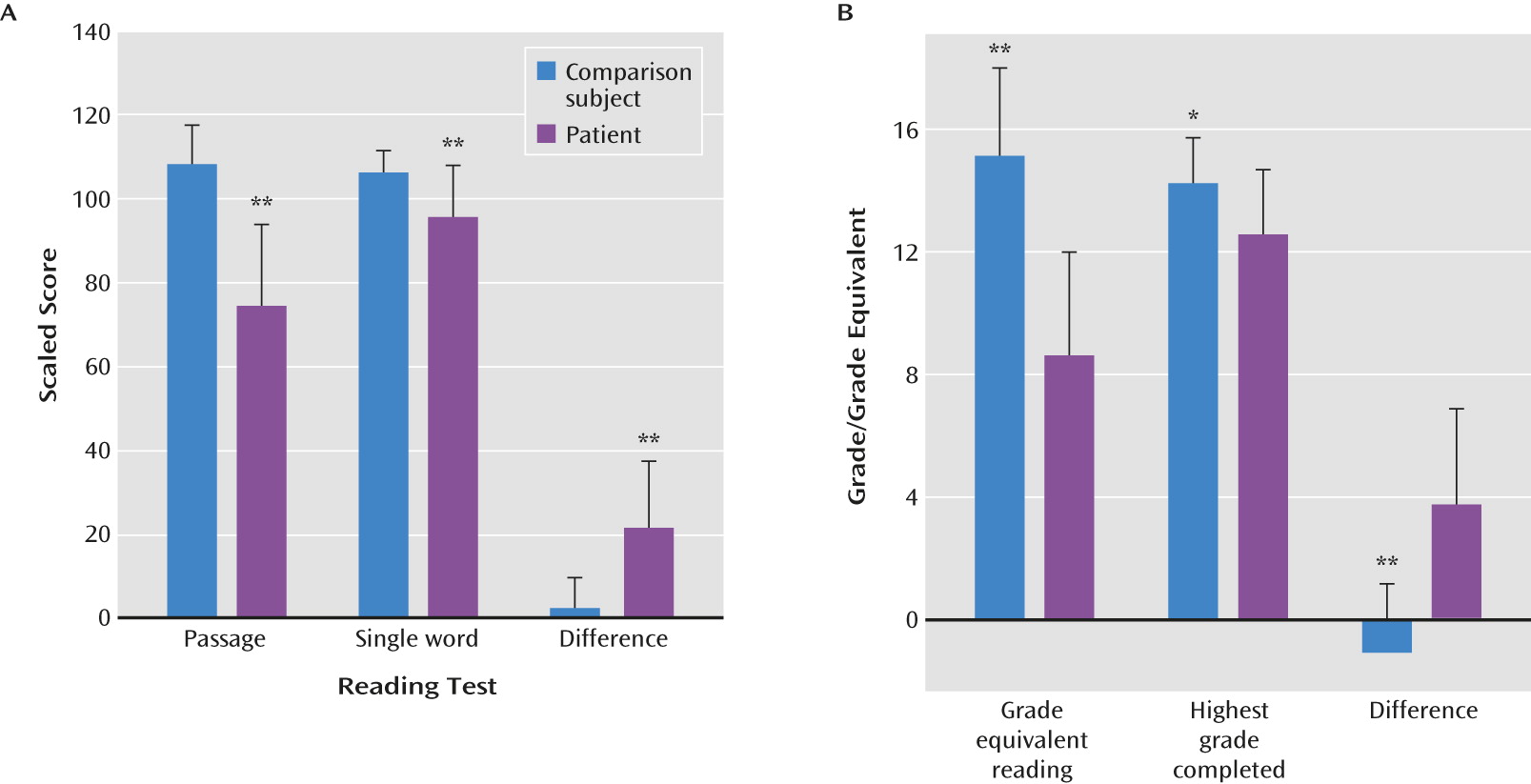
First, we compared performance on passage reading ability (i.e., ability to read paragraphs of information) with performance predicted using single-word reading (WRAT) (
Figure 1A). For comparison subjects, these two scores were highly similar (paired t=1.46, df=23, p=0.16). In contrast, for patients, passage reading ability was significantly reduced both relative to comparison subjects (p<0.0001) and relative to within-subject levels predicted by WRAT reading (paired t=8.97, df=44, p<0.0001). The group-by-test interaction was therefore highly significant (F=46.6, df=1, 67, p<0.0001), confirming differential impairment in passage compared with single-word reading ability in schizophrenia.
Second, we compared grade equivalent reading, as determined by the Nelson-Denny Reading Test, to years of education completed. In this analysis, comparison subjects had grade-equivalent scores closely matching their years of education completed (
Figure 1B). In contrast, patients showed grade-equivalent scores that were substantially reduced relative to years of education completed (paired t=6.35, df=27, p<0.0001), leading again to a highly significant group-by-type of achievement (reading level/grade level) interaction (F=16.37, df=1, 41, p<0.001).
Moreover, although patients had completed fewer years of education, between-group differences in Nelson-Denny scores remained strongly significant (F=27.4, df=1, 40, p<0.0001) even after covariation for this difference. Patients were far more likely than comparison subjects to have attended special school (12/41 compared with 1/23, likelihood ratio χ2=7.2, p=0.007). However, no significant relationship was found between school type and reading scores (F=0.7, df=1, 39, p=0.4), and between-group deficits remained highly significant even when differences in school type were considered (F=26.1, df=1, 39, p<0.0001). All patients denied a history of developmental dyslexia.
Finally, passage reading scores were similar among patients drawn from inpatient settings (mean=72.3 [SD=19.5]) compared with outpatient settings (mean=77.5 [SD=21.4]) (t=0.8, df=39, p=0.4). Passage reading scores were unrelated to length of illness (r=−0.04, N=41, p=0.8) and were significantly reduced relative to comparison subjects even in the small subgroup (N=6) who were within their first year of illness (mean reading score=66.7 [SD=12.9], t=9.07, df=28, p<0.0001).
Reading Compared With Sensory Measures
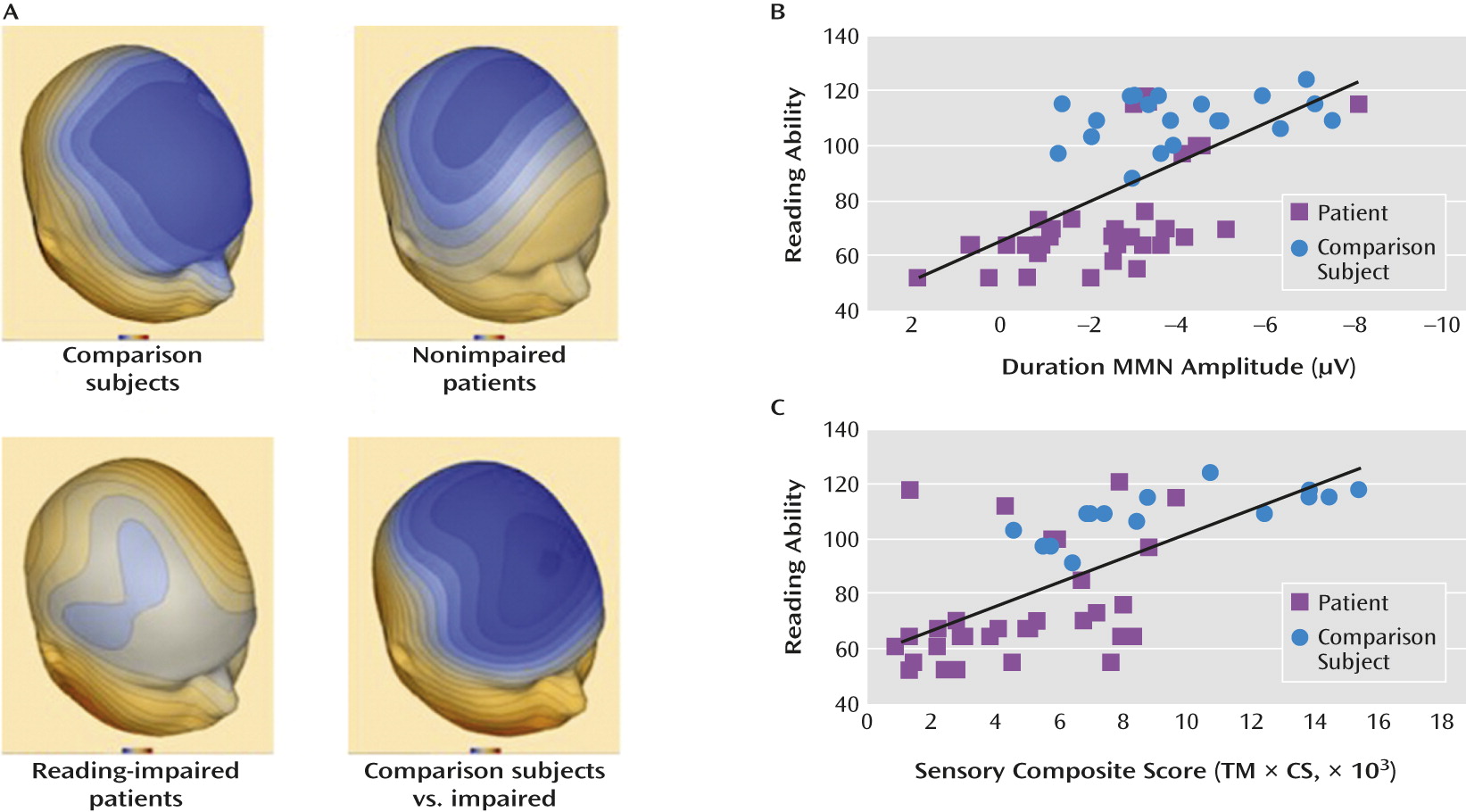
The integrity of early auditory processing was evaluated using mismatch negativity (
Figure 2A) and tone matching (
Table 3), while the integrity of visual processing was assessed using contrast sensitivity across spatial frequencies. As reported previously (
6,
9) patients displayed significant deficits relative to comparison subjects across all measures.
Relationship to overall reading ability was assessed using stepwise regression controlled, in step 1, for group status. A significant multivariate correlation was observed for mismatch negativity across deviant types (multivariate R
2=0.13, p=0.001). This correlation was driven primarily by response to duration deviants (r
p=0.50, df=46, p<0.001) (
Figure 2B) and remained significant even within patients alone (r
p=0.62, N=30, p<0.001).
Significant independent correlations were also observed for tone matching (r
p=0.44, df=45, p=0.002) and contrast sensitivity (r
p=0.37, df=45, p=0.01). A composite measure combining these two factors correlated highly both across groups controlling for group status (r
p=0.43, df=45, p=0.003), and within patients (r=0.42, N=33, p=0.016) and comparison subjects (r=0.73, df=15, p=0.002) independently (
Figure 2C). The relationship between reading ability and sensory measures also remained significant even when processing speed was used to control for between-group differences in overall cognition (r
p=0.48, df=47, p=0.001).
Prevalence of Impairment
Thirty of 41 (73%) schizophrenia patients met criteria for current dyslexia based on a score >1.5 standard deviations below adult norms for passage reading, compared with zero of 24 comparison subjects (χ2=42.0, p<0.0001). By contrast, only one of the 41 patients (2.4%) had single-word reading (WRAT) scores >1.5 standard deviations below adult norms, suggesting relatively intact premorbid function. Thus, the large majority of patients with present reading impairment (29/30, 97.0%) displayed a discrepancy between premorbid and present reading abilities. When reading was considered at a grade-equivalent level based on the Nelson-Denny test, 14/28 patients (50%) receiving the full battery, but only one comparison subject, were found to be reading at below eighth-grade reading level (χ2=9.45, df=1, p=0.002). Eight of 28 (29%) were reading at fifth-grade level, which represents the lower cutoff of the test.
When schizophrenia patients who had received the full Comprehensive Test of Phonological Processing (N=32) were subdivided into subtypes based on impaired visual (rapid naming/alternative rapid naming) compared with phonological (phonological awareness/alternate phonological awareness) scores <1.5 standard deviations below norms, 11 (34.4%) were categorized as normal readers, four (12.5%) as visual subtype, 10 (31.3%) as phonological subtype, and seven (21.9%) as double-deficit dyslexia. Overall reading scaled scores varied significantly across subtypes (F=3.96, df=3, 28, p=0.02) and were worse in patients with phonological (mean=66.20 [SD=11.5], post hoc p=0.008) and double-deficit (mean=65.3 [SD=8.6], post hoc p=0.012) dyslexia than in those with neither visual nor phonological impairments (mean=86.6 [SD=19.6]). Mismatch negativity to duration stimuli (
Figure 2A) also differentiated strongly between patients with and without reading impairment (t=3.56, df=29, p=0.001).
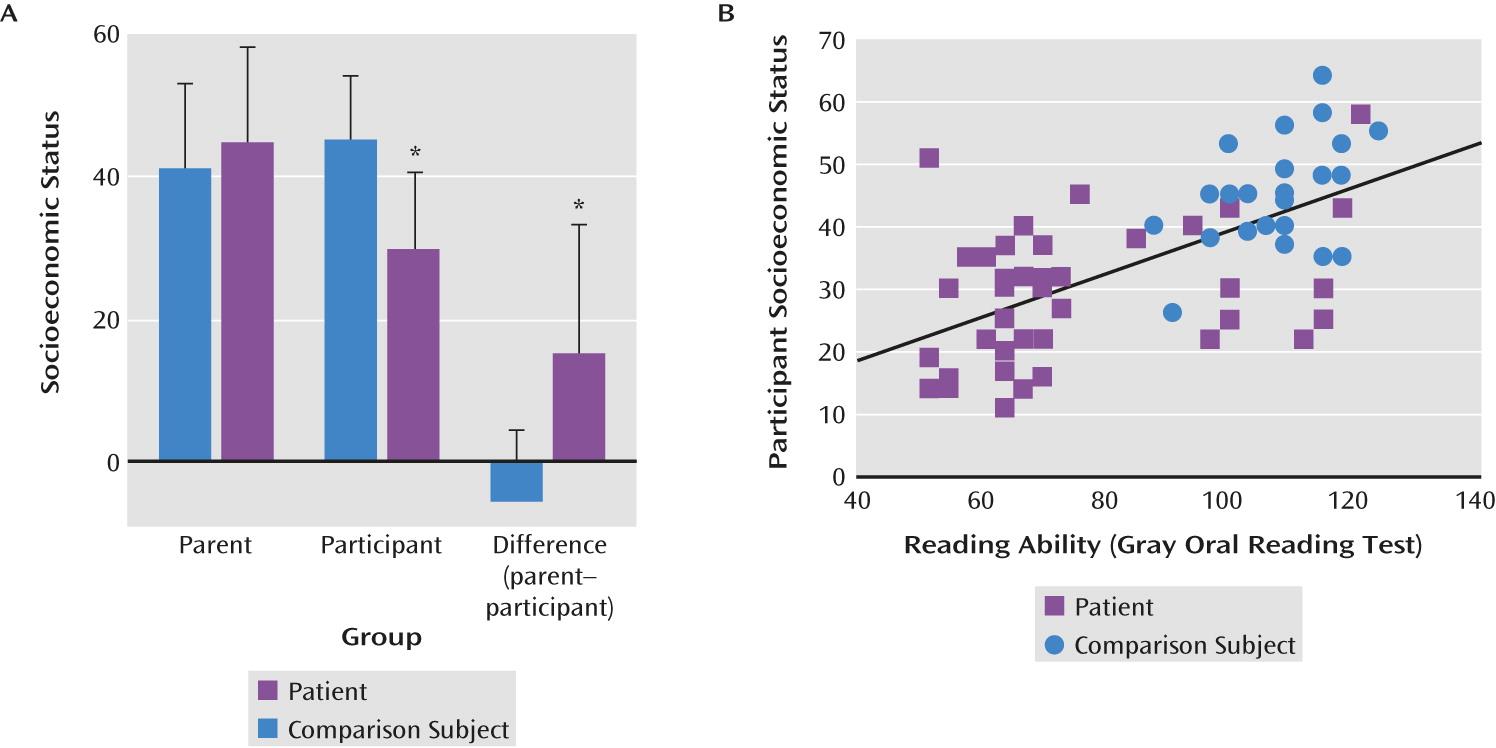
Relationship to Socioeconomic Status, Functional Outcomes, and Symptoms
As expected, schizophrenia patients in this study differed significantly in socioeconomic status not only from comparison subjects (
Figure 3A), but also from their parents (paired t=3.94, df=25, p=0.001). In contrast, healthy comparison subjects had similar scores to their parents (paired t=1.62, df=20, p=0.12), leading to a highly significant group-by-generation interaction (F=15.7, df=1, 45, p<0.0001). The group-by-generation interaction remained significant even following covariation for reduced educational achievement (F=7.86, df=1, 44, p=0.008).
Given the potential importance of reading to occupational function, a multivariate regression analysis was performed to assess the effects of reading and control variables on socioeconomic status. Impaired reading ability correlated significantly with reduced socioeconomic achievement over and above the contribution of diagnosis (r
p=0.37, N=68, p=0.002) (
Figure 3B). By contrast, no significant correlation was observed for either processing speed (r
p=0.13, N=54, p=0.4) or working memory (r
p=0.11, N=55, p=4).
Furthermore, when control (education, processing speed, and working memory) and reading scores were entered simultaneously, only reading remained a significant predictor of socioeconomic status (r
p=0.37, N=50, p=0.01). Finally, as observed in our pilot study (
38), reading ability in patients correlated strongly with score on the Independent Living Scales (r=0.42, N=41, p=0.007). No significant correlations of reading ability with PANSS scores or with medication dosage were observed.
Clinical High-Risk Patients
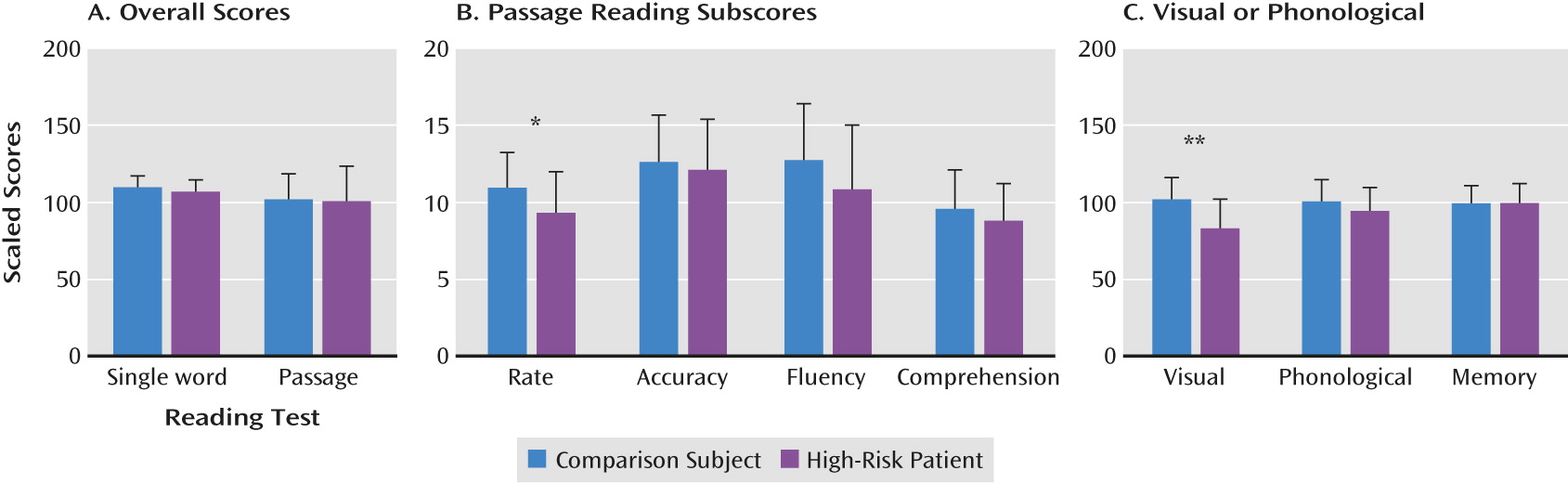
Reading measures were also obtained in a group of 19 high-risk individuals and 41 comparison subjects of similar age and gender. On global indices, high-risk patients had single-word (WRAT) and passage reading scores that were not significantly different from comparison subjects (
Figure 4A). By contrast, reading rate was significantly reduced (t=2.24, df=58, p=0.03) (
Figure 4B), although comprehension and accuracy scores were not significantly different from either comparison subjects or published norms.
On the Comprehensive Test of Phonological Processing (
Figure 4C), phonological processing scores in clinical high-risk patients were not significantly different from comparison subjects (t=1.47, df=56, p=0.15, d=0.4). By contrast, rapid naming scores were significantly reduced (t=4.30, df=56, p<0.0001, d=1.1), resulting in both a significant main effect of group (F=13.2, df=1, 56, p=0.001) and a significant group-by-test interaction (F=7.15, df=1, 56, p=0.01). Furthermore, visual reading scores were statistically similar to those in patients with established schizophrenia (t=0.8, df=45, p=0.4), whereas phonological measures were significantly superior (t=4.97, df=58, p<0.0001, d=1.1), again leading to a significant group-by-test interaction (F=7.12, df=1, 45, p=0.011). Tone-matching scores (90.6% correct [SD=7.5]) were also not significantly different between high-risk individuals and healthy comparison subjects.
Finally, despite similar ages (mean=21.0 years old [SD=2.8]), schizophrenia patients in their first year of illness nevertheless had significantly lower passage reading scores (mean=66.7 [SD=12.9]) than comparison subjects (mean=100.8 [SD=23.1]) (t=3.42, df=23, p=0.002) and significantly lower phonological processing scores (mean=71.3 [SD=10.7]) than comparison subjects (mean=94.7 [SD=15.3]) (t=3.46, df=23, p=0.002). However, visual reading scores were not significantly different (mean=85.7 [SD=12.0] compared with mean=82.8 [SD=19.7], t=0.34, df=23, p=0.7).
Discussion
The ability to read is one of the most basic necessities for personal and occupational success in developed countries. For some individuals, learning to read may be difficult. However, for the vast majority of individuals, once these skills are developed they are retained for life. The present study demonstrates that such a situation may not be true in schizophrenia. In the present study, even relatively young schizophrenia patients showed deficits that were not only extreme in magnitude (effect size, d>2.0), but were also much larger than the approximately one standard deviation of general cognitive impairment and sensory dysfunction associated with the disorder.
In a previous pilot study that focused only on individuals with schizophrenia who nevertheless had preserved overall cognitive abilities (
38), we observed that these patients were reading on average at the 10th-grade level despite having completed more than 12 years of education. In this more representative sample of persistently ill schizophrenia patients drawn primarily from long-term inpatient and residential care facilities, over 70% of patients met criteria for dyslexia, with 50% of patients reading below an eighth-grade level, and 29% reading at or below fifth-grade levels corresponding to percentile scores <10%. These levels constituted reductions of about 20 scaled score points relative to premorbid reading ability (
Figure 1A), corresponding to approximately four grade levels compared with objective years of schooling completed or estimated premorbid reading levels (
Figure 1B).
Furthermore, deficits in reading significantly predicted poor “real world” function as reflected in socioeconomic status (
Figure 3B). In contrast, parental socioeconomic status did not affect either educational achievement or reading ability, suggesting that the “downward drift” associated with schizophrenia is a consequence of impaired functional ability rather than familial circumstances (
39,
40). Previous studies have demonstrated significant contributions of cognitive disability in schizophrenia to a range of real-world outcome measures, including interpersonal skills, community activity, work skills (
41), and quality of life measures (
42,
43). How reading disability interrelates with other cognition and outcome impairments in schizophrenia beyond socioeconomic status will need to be pursued in future investigations.
Relative to patients with established schizophrenia, clinical high-risk individuals displayed passage reading abilities that did not differ significantly from comparison subjects in this limited sample, although further studies are required to determine whether some degree of deficit may nevertheless be present. Despite the lack of a significant between-group difference in overall passage reading ability in this sample, their level of visual processing was nevertheless significantly reduced relative to both test norms and matched comparison subjects (
Figure 4), and was similar to levels observed in patients with established schizophrenia, suggesting that visual deficits may pre-exist illness onset and may predispose to development of later functional reading impairments. Whether or not phonological processing deficits also exist prior to illness onset remains to be determined.
In addition to confirming prior findings of impaired reading in established schizophrenia, the present findings are consistent with an emergent literature suggesting that visual processing deficits represent a stable, trait/risk factor for schizophrenia, whereas loss of auditory function occurs in the years immediately surrounding illness onset and thus may represent the proximate cause of the decline in absolute reading ability associated with schizophrenia onset (
9). Thus, deficits in visual neurophysiological measures are present even in unaffected family members of schizophrenia patients (
44), and, in schizophrenia, are unrelated either to premorbid function or length of illness (
9). In contrast, deficits in mismatch negativity generation in response to duration deviants first develop during the years preceding illness onset and are among the strongest cognitive predictors of conversion to psychosis (
45,
46), while deficits in mismatch negativity to frequency deviants may progress even following illness onset (
47,
48), and thus may represent extension of dysfunction to primary sensory regions. In follow-back studies, mismatch negativity deficits, especially to duration deviants, are strongly related to premorbid educational attainment, consistent with the notion that regression of these pathways during the perionset period limits achievement (
9).
Database Studies
The present findings are also consistent with follow-back studies of reading ability performed using retrospective databases. For example, in studies using Iowa Scholastic Test scores of individuals who ultimately developed schizophrenia, reading scores were observed to decline from the 45th to 37th percentile from eighth to 11th grade even before illness onset (
31,
49). Similarly, small (d=0.2–0.4) but significant (p<0.05) deficits in reading and reading comprehension were found in follow-back studies using the Israeli army conscription database (
50,
51). Those follow-back scores correspond well to the premorbid 41st percentile reading levels estimated based on WRAT reading scores in the present study.
Our present study demonstrates that further reduction to 17.5th percentile scores on passage reading (equivalent to scaled score of 74.2) occurs early in the course of the illness, suggesting functional decline in the years either directly preceding or immediately following illness onset. The decline in performance is not only larger than that for overall cognitive function (
Table 2) or simple sensory measures (
Table 3) considered independently, but may be more disruptive in terms of occupational function, given the extremely strong correlation between reading ability and socioeconomic status (
Figure 3)
Clinical Implications
On a clinical level, individuals with schizophrenia typically present in the second to third decades of life, i.e., during the late high school or early college years. Individuals developing schizophrenia typically experience academic difficulty even prior to symptom onset and rarely return to their prior level of academic performance (
52,
53). Although academic difficulties are often attributed to symptoms, general cognitive dysfunction, or outside factors (e.g., substance abuse), the present study suggests that regression in reading ability, best conceptualized as a secondary or acquired dyslexia, must also be considered as a potential cause. A major unexplained finding in schizophrenia in general is the superior outcome in developing countries relative to developed countries, especially with outcomes such as employment (
54,
55). Given the present findings, the differences in base literacy rates in such countries may represent at least a partial explanation for the differential outcome.
In summary, the present study demonstrates deficits in reading ability that were more severe than would be expected based on general cognitive impairment alone in this sample, with 73% of schizophrenia patients meeting criteria for dyslexia despite intact prior reading ability, including 29% of patients reading at the fifth-grade level or below, which is a widely used cutoff for functional illiteracy (
2). Significant, albeit less-pronounced, deficits in visual reading scores were present in individuals at high clinical risk for schizophrenia and may be deserving of future investigation. Although deficits in phonological processing were not observed in the limited sample of high-risk patients who were tested, these may emerge when studies are extended to larger populations. The decline in reading ability from premorbid levels, which appears to occur during early stages of the illness, correlates highly with the failure to meet socioeconomic expectations, and may thus represent a remediable cause of persistent occupational disability in schizophrenia.
Patients were selected for this study only if they showed IQ levels ≥85, and thus were “underimpaired” on measures such as processing speed and working memory compared with typical schizophrenia outpatients (
56). It may be that in a more globally impaired sample, the reading scores would be even more impaired and contribute even more strongly to functional outcome, but this issue can only be addressed through future large-scale investigation.