An “Alternative DSM-5 Model for Personality Disorders” was published in Section III (“Emerging Measures and Models”) of the manual. The foundations of this hybrid model for the assessment and diagnosis of personality pathology are dimensional ratings of 1) the severity of impairment in personality (self and interpersonal) functioning and 2) 25 pathological personality trait “facets” organized into five broad trait “domains.” When combined with other inclusion and exclusion criteria, these assessments redefine the construct of personality disorder consistently in terms of personality functioning and personality traits, provide for an efficient stepwise approach to personality disorder assessment, and enable the diagnosis of six specific personality disorder categories, along with “personality disorder–trait specified” for all other presentations. The “Alternative Model” was the product of the DSM-5 Personality and Personality Disorder Work Group, was approved by the DSM-5 Task Force, and was intended for inclusion in Section II of DSM-5, “Diagnostic Criteria and Codes.” However, the APA Board of Trustees voted to put the new model in Section III and to continue with the categories and criteria from DSM-IV for the personality disorders in DSM-5 Section II.
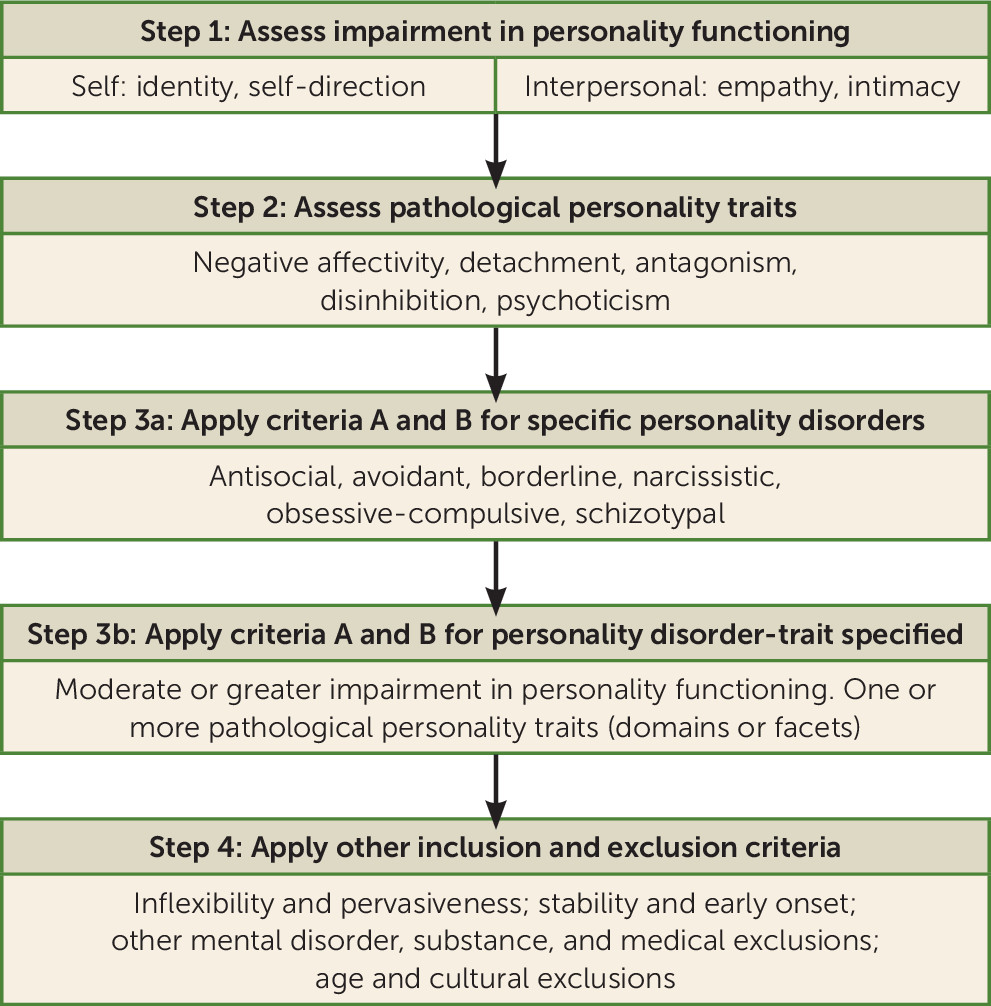
Figure 1 illustrates a stepwise approach to assessing personality disorder. The Alternative Model was deliberately designed to be flexible and “telescoping” in its clinical application, such that assessments might be made at the level of personality functioning (e.g., to screen for personality disorder or to track progress in treatment over time), pathological personality traits (whether or not a person also has a personality disorder), and/or personality disorder, based on available time, information, and expertise. The assessment begins with an evaluation of impairments in four elements of personality functioning—identity, self-direction, empathy, and intimacy—that were identified in the existing clinical literature as core aspects of personality disorder that can be reliably assessed (
1) and were shown in secondary data analyses to have good diagnostic efficiency for DSM-IV personality disorders diagnosed via semistructured interview (
2). These impairments are measured in combination on a single 5-point scale of severity, the Level of Personality Functioning Scale (see DSM-5, pp. 775–778). Research indicates that generalized severity of personality psychopathology is the most important single predictor of concurrent and prospective dysfunction (
3). It is widely agreed (e.g.,
4–
8) that assessment of severity is essential to any dimensional system for personality psychopathology. The score of 2 (moderate impairment) or greater that is required for a diagnosis of a personality disorder was determined empirically to identify personality disorder with a maximal combination of sensitivity and specificity (
9), so that a clinician would have a very good sense of whether or not a person had a personality disorder based on the single-item Level of Personality Functioning Scale score.
The second step in the assessment of a personality disorder is an evaluation of pathological personality traits. The Alternative Model describes pathological personality according to five personality trait domains—negative affectivity, detachment, antagonism, disinhibition, and psychoticism—which correspond to the pathological “poles” of the well-known and widely validated five-factor model of personality. Each trait domain consists of three to six more specific personality trait “facets” (e.g., emotional lability in the negative affectivity domain; impulsivity in the disinhibition domain). A trait judged to be moderately or very descriptive of a person is counted as present. The personality trait assessment serves as a personality trait “review of systems” and describes the myriad manifestations of personality disorder. With a profile of descriptive traits and a Level of Personality Functioning Scale score, a clinician would have general knowledge of the characteristics of a person’s personality psychopathology and its severity.
The third step in the assessment is to apply the A and B criteria for the six specific disorders included the Alternative Model. The A criteria refer to impairments in personality functioning characteristic of each personality disorder and the B criteria refer to specific personality disorder trait manifestations. The diagnostic thresholds for the A criteria (two or more) and the number and configuration of traits needed to meet the B criteria were also empirically determined to maximize correspondence with DSM-IV personality disorder diagnoses and thus to be minimally disruptive to practice and research in shifting from DSM-IV to the new DSM-5 model, to minimize overlap with other personality disorders to reduce comorbidity, and to maximize relationships to general impairment in psychosocial functioning (
10). Patients who meet criteria A and B for a specific personality disorder may be given a “provisional diagnosis” of that personality disorder (
Figure 1, step 3a). Patients who do not meet the criteria for a specific personality disorder may qualify for a diagnosis of personality disorder–trait specified if they have moderate or greater impairment in personality functioning and one or more pathological personality traits (
Figure 1, step 3b).
The fourth and final step in the assessment is to apply the other inclusion and exclusion criteria of the Alternative Model’s general criteria. The impairments in personality functioning and the individual’s personality trait expressions should be 1) relatively inflexible and pervasive across a broad range of personal and social situations; 2) relatively stable across time, with onsets that can be traced back to at least adolescence or early adulthood; 3) not better explained by another mental disorder; 4) not solely attributable to the physiological effects of a substance or another medical condition; and 5) not better understood as normal for an individual’s developmental stage or sociocultural environment. If these additional conditions are met, then the diagnosis of a personality disorder can be made.
The Alternative Model for Personality Disorders met with considerable resistance from some quarters in the personality disorder field. The arguments for and against it have been made in a number of journal special issues on personality disorder over the past 5 years (for example,
Personality Disorders: Theory, Research, and Treatment, vol. 2, no. 1 [January 2011];
Journal of Personality Disorders, vol. 25, no. 2 [April 2011]; and
Personality Disorders: Theory, Research, and Treatment, vol. 4, no. 4 [October 2013]). In brief, the Alternative Model was perceived by some as too complicated for general clinical use and was predicted to be too disruptive to clinical practice and research to be useful because of its extensive revisions. However, many of the critiques of the proposed new model were speculative and unsupported by data. For example, clinicians with little or no training can make reliable judgments about impairments in personality functioning using the Level of Personality Functioning Scale and about pathological personality traits (
11–
13). In the DSM-5 Field Trials (
12), the reliability of diagnoses of borderline personality disorder defined according to Alternative Model criteria was comparable to that of bipolar I disorder, greater than those of schizophrenia and major depressive disorder, and exceeded only by those of major neurocognitive disorder and posttraumatic stress disorder. In a study comparing patients on all DSM-IV and DSM-5 personality disorder criteria and dimensions, the correlations between criterion counts of DSM-IV and DSM-5 diagnostic concepts in 337 patients were as follows: borderline personality disorder, 0.80; antisocial personality disorder, 0.80; avoidant personality disorder, 0.77; narcissistic personality disorder, 0.74; schizotypal personality disorder, 0.63; and obsessive-compulsive personality disorder, 0.57 (
10). In most instances, these values are comparable to the established joint interview reliabilities of these diagnoses under DSM-IV, suggesting that the agreement between DSM-IV and DSM-5 Section III personality disorder diagnoses is likely to be as high as that between two diagnosticians on DSM-IV (and now DSM-5 Section II) diagnoses. Furthermore, in a recent study of the perceived clinical utility of the Alternative Model compared with DSM-IV personality disorder (now DSM-5 Section II) criteria, the DSM-5 trait model was judged to be more useful with respect to ease of use, communication with patients, comprehensive description of personality pathology, formulation of effective treatment interventions, and description of an individual’s global personality—by both psychiatrists and psychologists (
14).
The Alternative Model is not in Section III’s “Conditions for Further Study” chapter. Therefore, clinicians can regard it as a true “alternative” to the standard approach in Section II and can use it for patient assessment and diagnosis. Furthermore, the Alternative Model is prominently featured in recent textbooks published by American Psychiatric Publishing, including in the “Personality Disorders” chapter of
The American Psychiatric Publishing Textbook of Psychiatry, 6th Edition (
15), where it is compared and contrasted in detail with the Section II model, and throughout
The American Psychiatric Publishing Textbook of Personality Disorders, 2nd Edition (
16)—both “DSM-5 Editions.” Thus, in this article, we demonstrate the clinical application of the Alternative Model to a case with probable personality disorder (presented in the vignette) to facilitate clinicians’ use of the model with their own patients. The clinical utility of elements of the Alternative Model are highlighted.
Differential Diagnosis
Ms. B, the patient in the vignette, presented for treatment in the midst of a period of depression of relatively recent onset following a significant career disappointment. The depression meets DSM-5 criteria for a major depressive episode with persistently depressed mood (feeling empty), hypersomnia, fatigue, feelings of worthlessness, diminished ability to concentrate, and recurrent thoughts of death for more than 2 weeks that cause significant distress and are not attributable to the physiological effects of a substance or another medical condition. In the absence of evidence of a psychotic disorder or a manic or hypomanic episode, a diagnosis of major depressive disorder should be made. Although the patient also currently reports worry about her future, these worries are insufficiently pervasive, persistent, distressing, or impairing for a diagnosis of generalized anxiety disorder.
Ms. B also reports, however, a more long-standing problem with social anxiety and avoidance. This anxiety does not conform to the pattern of social anxiety disorder because it is less about fear of social situations and of showing anxiety symptoms that will be humiliating or embarrassing, and more about a pattern of social inhibition, feelings of personal inadequacy, and hypersensitivity to negative evaluation. Because she avoids social activities for fear of disapproval or rejection, is unwilling to get involved with people unless she is certain that she will be liked, is restrained in intimate relationships because of feelings of shame, and views herself as socially inept and personally unappealing, a DSM-5 Section II diagnosis of avoidant personality disorder applies.
More significant, however, is her pattern of variable and vulnerable self-esteem, with attempts at regulating self-esteem through approval seeking and covert grandiosity, which is characteristic of DSM-5 Section III narcissistic personality disorder. The patient clearly does not conform to the Section II diagnosis of narcissistic personality disorder, which requires a pervasive pattern of overt grandiosity. According to the Alternative Model, a rating of moderate or greater impairment in personality functioning is required for a personality disorder diagnosis to be made.
Thus, there are several ways in which Ms. B’s personality problems should be approached from the perspective of the Section III Alternative DSM-5 Model for Personality Disorders (see
Figure 1). First, an assessment should be made with the Alternative Model’s Level of Personality Functioning Scale. In this instrument’s “self” domain of
identity, the patient shows excessive dependency on others for identity definition, vulnerable self-esteem with exaggerated concern about external evaluation, a sense of inferiority with compensatory self-appraisal fluctuating between an inflated and a deflated sense of self, and emotional regulation that depends on positive external appraisal with anger and shame when her self-esteem has been threatened (e.g., by being passed over for partnership). In the Level of Personality Functioning Scale domain of
self-direction, the patient has often set goals and acted to gain external approval, has very high personal standards, and has little capacity to reflect on internal experience. In the “interpersonal” domain of
empathy, she pays attention to others inasmuch as they meet her needs for approval but has little actual understanding of others’ experiences or perspectives, and she has little appreciation of the effects of her behavior on others. Finally, in the domain of
intimacy, the patient has a few friends whom she sees occasionally. She desires a close relationship with a man but feels she will not be appreciated or understood, and she looks mostly to others in order to feel better about herself. According to the Level of Personality Functioning Scale, this patient would be rated as having moderate impairment (a rating of 2) in personality functioning.
The patient also appears to exhibit numerous pathological personality trait facets from the DSM-5 trait model, including depressivity, withdrawal, intimacy avoidance, anhedonia, grandiosity (covert), attention seeking, and rigid perfectionism. Thus, it is likely that this patient meets criteria either for one of the six specific personality disorders in DSM-5 Section III or, if her pattern of impairment in personality functioning and traits does not conform to the criteria for a specific personality disorder, for personality disorder–trait specified.
Section III avoidant personality disorder or narcissistic personality disorder (or both) should be considered (
Tables 1 and
2). According to the A criterion for avoidant personality disorder, a patient’s identity problems should include low self-esteem with self-appraisal as socially inept and personally unappealing. In certain circumstances, particularly social ones, this description fits Ms. B, but her self-esteem vacillates, so that sometimes she feels superior to others, such as when she received top grades in school or received positive feedback about her work performance. Self-esteem problems that shift between inflated and deflated self-appraisal are more consistent with the identity problems of narcissistic personality disorder than of avoidant personality disorder. Both avoidant personality disorder and narcissistic personality disorder are characterized by impaired self-direction that is governed by unrealistic standards of behavior. These high standards have made Ms. B reluctant to pursue a social life and outside interests, and her strict work ethic has led her to feel superior to coworkers. Furthermore, her tendency to avoid activities in which she is not obviously talented or is not likely to be immediately successful may actually be a reflection of low standards (i.e., a view of herself as perfect without a need for training or practice)—a form of narcissistic entitlement.
In the interpersonal sphere, Ms. B is attuned to others’ opinions of her and she is very sensitive to criticism and rejection, consistent with avoidant personality disorder. However, she is also unaware of the feelings and needs of others and underestimates how her behavior affects them, in common with narcissistic personality disorder. Finally, the A4 criterion for avoidant personality disorder in the Alternative Model requires intimacy problems manifested by the person’s reluctance to get involved with others for fear of being ridiculed or shamed, while the A4 criterion for narcissistic personality disorder states that relationships are largely superficial and mainly bolster self-esteem and that the person has little genuine interest in others unless there is the potential for personal gain. The latter characterization appears to fit Ms. B’s interpersonal functioning better. The A criterion for personality disorders according to the Alternative Model requires difficulties in at least two of the four areas of identity, self-direction, empathy, and intimacy. Technically, Ms. B has impairments in personality functioning typical of both avoidant personality disorder and narcissistic personality disorder, although her personality functioning seems to fit better with the A criterion manifestations of narcissistic personality disorder.
The B criterion for avoidant personality disorder in the Alternative Model (see
Table 1), however, also requires three of the following four pathological traits: anxiousness, often in reaction to social situations (required); withdrawal; intimacy avoidance; and anhedonia. Judgments about the presence of pathological personality traits are based on how descriptive they are of a patient, from “not at all,” to “mildly,” “moderately,” or “extremely” descriptive. Moderately or extremely descriptive would count as the required level of descriptiveness for a pathological personality trait to be noted. Although Ms. B is anxious in social situations and generally avoids them, she does not, in general, appear to have the intense feelings of nervousness, tenseness, or panic, the pervasive worry about the past and future, and the fear, apprehension, and threat of uncertainty that define the DSM-5 trait facet of anxiousness. The B criterion for narcissistic personality disorder requires both grandiosity and attention seeking. It may not seem as if Ms. B is grandiose, but a major difference between DSM-5 Section II and Section III criteria for narcissistic personality disorder is that feelings of entitlement and self-centeredness can be “covert,” as well as “overt,” in the Section III disorder (
17). This change is in keeping with modern concepts of pathological narcissism and narcissistic personality disorder, which include both inflated (i.e., grandiose) and deflated (i.e., vulnerable) presentations and overt and covert expressions (
18–
20). Ms. B’s belief that she is smarter and more diligent than many of her coworkers and her condescension toward them is self-evident. Finally, although it may not look as if Ms. B is attention seeking in the typical sense, much of her behavior is motivated by the desire to receive the admiration and approval of others.
According to the Alternative DSM-5 Model of Personality Disorders, Ms. B meets criteria A and B for narcissistic personality disorder, but not avoidant personality disorder, because she lacks the general trait of anxiousness. Her impairments in personality functioning and personality traits appear to be relatively inflexible and pervasive; long-standing and relatively stable; not better explained by her major depressive disorder; not attributable to a substance or to another medical condition; and not normal for her developmental stage or culture. Therefore, a diagnosis of narcissistic personality disorder can be made. Using the Alternative Model, it is also possible to individualize a personality disorder diagnosis with additional relevant trait “specifiers.” Thus, Ms. B would receive a diagnosis of narcissistic personality disorder, with depressivity, withdrawal, anhedonia, and intimacy avoidance (several traits of the so-called vulnerable narcissist) (
19), plus rigid perfectionism.
If one conceptualized personality psychopathology solely according to the dimensional components of the Alternative Model, however—that is, without the categorical personality disorder diagnoses—then a complex disturbance such as Ms. B’s would be represented by the moderate impairment in personality functioning and the traits she exhibits. The traits can be represented at the level of the DSM-5 trait domains of negative affectivity (depressivity), detachment (withdrawal, anhedonia, intimacy avoidance) and antagonism (grandiosity, attention seeking) or by the specific individual trait facets themselves. Focusing on the degree of impairment in personality functioning and itemizing applicable pathological traits provides the most detailed personality profile of a patient and sometimes may be more helpful than a particular personality disorder diagnosis in planning and focusing treatment (
21).
Clinical Utility
Various specific types of psychotherapy focus on aspects of impairments in sense of self and in interpersonal relationships, as well as on pathological trait domains such as negative affectivity, detachment, and antagonism. For example, the goal of transference-focused therapy, an object relations model of treatment, is to change a state of identity diffusion into a more coherent identity by increasing self-reflective functioning and self-modulation of negative emotions (
22). Mentalization-based therapy challenges automatic, distorted, and simplistic assumptions of the patient about self and others, in a fashion similar to some cognitive therapies. Traditional cognitive-behavioral therapy uses cognitive restructuring, exposure, and intimacy skills training to decrease social anxiety and social avoidance, either in individual or group treatment (
23). Schema-focused therapy is based on the premise that rigid patterns of avoidance and other compensatory behaviors develop to avoid triggering painful schemas about self and others. Modification of maladaptive schemas formed early in life leads to reduced expression of pathological traits (e.g., withdrawal, intimacy avoidance).
Self-interpersonal problems such as insecure attachment and maladaptive schemas have been shown to be associated significantly with personality disorder psychopathology and impairments in psychosocial functioning in general, as well as to affect treatment alliance and outcome (e.g.,
24–
34). Furthermore, self pathology has been shown to have incremental validity over interpersonal pathology in predicting overall severity of personality pathology (
35), so both components are represented in the DSM-5 Level of Personality Functioning Scale. The severity of impairment in self and interpersonal functioning also has predicted important factors such as treatment utilization and treatment course and outcome (e.g.,
27,
33–
39); thus, personality functioning is measured on a dimensional scale of severity in the Alternative Model. Finally, personality functioning constructs align well with the National Institute of Mental Health Research Domain Criteria domain of social processes (
40), which includes “perception and understanding of the self,” “perception and understanding of others,” and “affiliation and attachment” as core constructs. Thus, the Alternative Model approach to personality pathology is likely to influence and be influenced by future research on the fundamental mechanisms involved in personality and other psychopathology.
In addition to the independent utility of personality functioning constructs and of pathological personality traits, a number of recent studies support a model of personality psychopathology that specifically
combines ratings of disorder and trait constructs (i.e., a hybrid model). Each approach has been shown to add incremental value to the other in predicting important antecedent (e.g., family history, history of child abuse), concurrent (e.g., functional impairment, medication use), and predictive (e.g., functioning, hospitalization, suicide attempts) variables (
41–
44).
A survey of clinicians’ assessments of their patients examined the relationships between DSM-IV categorical personality disorder diagnoses and DSM-5 personality disorders and their components to clinical judgments concerning 1) current psychosocial functioning, 2) risk for self-harm, violence, and criminality, 3) optimal level of treatment intensity, and 4) prognosis (
9,
11). DSM-5 components together and individually (personality functioning level and traits) had appreciably stronger unadjusted and corrected correlations with these judgments than DSM-IV personality disorder categories in 11 of 12 comparisons. The only exception was for the prediction of perceived risk, which was more associated DSM-IV personality disorders than with DSM-5 level of personality functioning ratings. (However, DSM-5 traits in isolation and DSM-5 Level of Personality Functioning Scale ratings and traits combined were superior to DSM-IV categories in predicting perceived risk.)
The incremental validity of the DSM-IV and DSM-5 personality disorder systems, that is, the associations between each of the two personality disorder systems and the above-mentioned four clinical judgments, while controlling for the effects of the other, was also examined. The partial multiple (and corrected) correlations showed that DSM-5 personality disorder renderings significantly incremented DSM-IV personality disorders in predicting all four clinical judgments, while DSM-IV did not provide any information above and beyond that provided by DSM-5. Thus, virtually all valid variance in DSM-IV personality disorder diagnoses was captured by DSM-5, but the converse was not true.
Conclusions
The Alternative DSM-5 Model for Personality Disorders provides clinicians with a clear, consistent, and coherent system for identifying personality psychopathology, quantifying its severity, and characterizing its myriad clinical manifestations in terms of impairments in personality functioning and pathological personality traits. The most important specific personality disorders are identified with diagnostic criteria, and all other presentations can be diagnosed and described using the diagnosis of personality disorder–trait specified. All aspects of the Alternative Model have been developed on the basis of empirical data, including the elements of personality functioning (
1,
2), assignment of criteria to the personality disorders (
11,
45–
47), and diagnostic threshold for the Level of Personality Functioning Scale and for the specific personality disorders (A and B criteria) themselves (
9,
10). The Alternative Model has been judged to be more clinically useful than the DSM-IV (now DSM-5 Section II) approach in the DSM-5 Field Trials (
48) and in a large national survey of psychiatrists and psychologists (
14). The various components of the Alternative Model have been shown to be useful in planning treatment and predicting its outcome. We encourage clinicians to try it without prejudgment. Our expectation is that it will be easy and straightforward to use and that it will change for the better the way clinicians think about their patients with personality pathology.