Mild traumatic brain injury (mild TBI; also known as concussion), previously believed to be an almost uniformly benign event, has garnered increased attention as a potential source of adverse neuropsychological outcomes in civilians (e.g., athletes who play contact sports) and military personnel alike (
1–
4). With respect to mental health outcomes, many observational studies—the earliest from military settings (
5,
6)—have established an association between mild TBI and posttraumatic stress disorder (PTSD) (
7–
15). Although most of these studies have been cross-sectional and/or retrospective in design, or have relied on hospitalized, treatment-seeking or other potentially nonrepresentative samples, a few studies of longitudinal prospective cohorts have clearly demonstrated an association between TBI and subsequent PTSD (
15,
16).
Numerous questions about the association between TBI and PTSD remain unanswered. Among them are uncertainties about the specificity of this association. Is PTSD a unique or particularly prevalent outcome of TBI, or is risk of developing (certain) other mental disorders comparable? A civilian study of 1,084 traumatically injured individuals found that TBI was a strong risk factor not only for PTSD but also for a wide range of depressive and anxiety disorders (
16). Another area of controversy pertains to the importance of the severity of TBI, particularly with regard to whether “very mild” (i.e., dazed but no loss of consciousness or amnesia) TBIs have a salient impact on subsequent mental health. To the best of our knowledge, neither of these questions has been addressed in a large, prospective longitudinal cohort and never in a military setting. The present study uses data from the Pre/Post Deployment Study (PPDS), a prospective, longitudinal component of the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS) (
17), to examine the relationships of deployment-acquired TBI with postdeployment PTSD and related disorders, controlling for a range of other known and hypothesized pre- and perideployment predictors of these outcomes.
Results
Participant Characteristics at Predeployment Baseline (T0)
All reported percentages and means are weight-adjusted. The sample was predominantly male (94.7% [SE=0.6%]) and less than 30 years of age (71.6% [SE=1.4%]). The majority of participants were White (71.8% [SE=0.8%]), with smaller proportions identifying their race as Other (12.2% [SE=0.6%]), Black (12.0% [SE=0.7%]), and Asian (4.0% [SE=0.3%]), and 16.1% (SE=0.6%) identifying their ethnicity as Hispanic. For 44.8% (SE=1.2%) of soldiers, the index deployment to Afghanistan was their first, with others reporting one (23.3% [SE=0.7%]) or multiple (31.8% [SE=1.1%]) previous deployments.
Estimated lifetime prevalence of mental disorders at the baseline (T0) interview was 12.0% (SE=0.6%) for PTSD, 9.3% (SE=0.6%) for major depressive episode, 8.3% (SE=0.4%) for generalized anxiety disorder, and 10.7% (SE=0.5%) for suicidality. Prior to deployment, mean PTSD symptom severity as measured by the 6-item PTSD Checklist was 7.87 (SD=3.49; median=6, range=6–30, interquartile range=6–8), and mean general distress was 11.03 (SD=14.51; median=6, range=0–96, interquartile range=2–13).
Approximately one-third of soldiers reported having sustained TBI(s) prior to the index deployment (T0), with 14.8% (SE=0.6%) endorsing one and 19.5% (SE=0.8%) endorsing two or more lifetime TBIs.
Deployment Stress and Deployment-Acquired TBI
The mean number of deployment stressors in the index deployment endorsed by respondents at T1 was 4.02 (SD=2.76; median=4, range=0–15, interquartile range=2–6). Approximately 1 in 5 soldiers reported exposure to TBI(s) during the index deployment, with 13.2% (SE=0.6%) endorsing probable very mild TBI (i.e., dazed only, no loss of consciousness or amnesia), 4.8% (SE=0.4%) endorsing probable mild TBI, and 1.2% (SE=0.2%) endorsing probable more-than-mild TBI.
Mental Health Outcomes at 3 Months Postdeployment (T2)
At the T2 follow-up, approximately 3 months postredeployment to the United States from Afghanistan, past-30-day DSM-IV PTSD was reported by 7.8% (SE=0.5%) of soldiers. The mean PTSD Checklist score at T2 was 24.80 (SD=10.78; median=21, range=17–85, interquartile range=17–28).
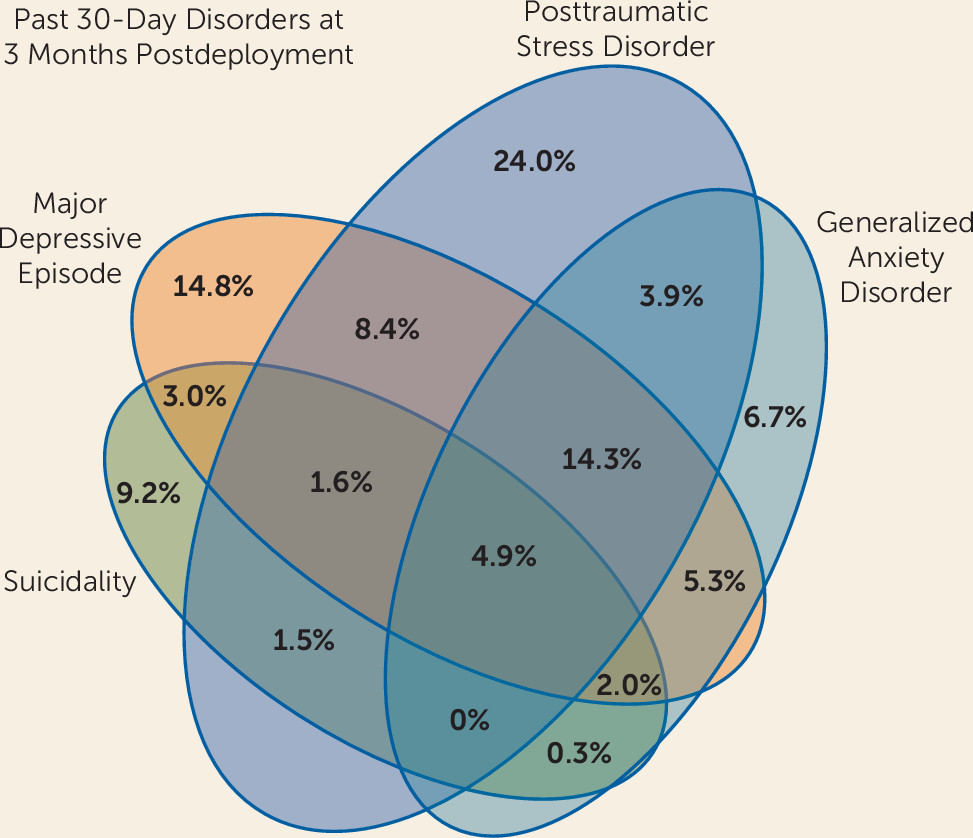
Past-30-day prevalence of other mental disorders at T2 was 6.8% (SE=0.4%) for major depressive episode, 4.8% (SE=0.3%) for generalized anxiety disorder, and 2.9% (SE=0.2%) for suicidality. The combined prevalence of any past-30-day PTSD, major depressive episode, generalized anxiety disorder, or suicidality at T2 was 12.9% (SE=0.6%; see
Figure 1 for depiction of comorbidity rates). The mean general distress score at T2 was 11.97 (SD=16.02; median=6, interquartile range=1–15).
Association of deployment-acquired TBI with posttraumatic stress outcomes.
In a logistic regression analysis adjusting for age group, sex, ethnicity, race, Brigade Combat Team, number of prior deployments, predeployment TBI history, lifetime PTSD predeployment, PTSD symptoms at baseline (6-item PTSD Checklist score at T0), and deployment stress severity, deployment-acquired TBI was strongly associated with increased odds of postdeployment (T2) past-30-day PTSD (adjusted odds ratio=1.81, 95% CI=1.32–2.46, p<0.0005; see
Table 1).
The above model was rerun stratifying TBI-positive subjects into those with probable “very mild,” “mild,” and “more than mild” concussions. Whereas all TBI-positive groups displayed increased odds for past 30-day PTSD at T2, a dose-response relationship was observed whereby odds of PTSD increased as TBI severity worsened (adjusted odds ratios=1.66, 1.76, and 3.90 for “very mild,” “mild,” and “more-than-mild,” respectively; p<0.0005).
Whereas the previous models evaluated presence or absence of PTSD as a dichotomous outcome, we also evaluated whether deployment-acquired TBI was associated with increased PTSD symptoms at T2. Having sustained a TBI during the index deployment was associated with increased odds of a nonzero score on the PTSD Checklist (i.e., having some PTSD symptoms versus none; adjusted odds ratio=1.47, 95% CI=1.03–2.08, p=0.04) and a 1.35-fold increase in PTSD Checklist score when symptoms were present (i.e., when the PTSD Checklist score was nonzero; fold change=1.35, 95% CI=1.21–1.51, p<0.001; see
Table 2).
Association of deployment-acquired TBI with other mental health outcomes.
In logistic regression analyses adjusting for age group, sex, ethnicity, race, Brigade Combat Team, number of prior deployments, lifetime history of the outcome in question (major depressive episode, generalized anxiety disorder, or suicidality) predeployment (T0), general distress predeployment (T0), and deployment stress severity, deployment-acquired TBI was associated with postdeployment (T2) risk of past-30-day major depressive episode (adjusted odds ratio=1.45, 95% CI=1.02–2.04, p=0.037) and generalized anxiety disorder (adjusted odds ratio=1.81, 95% CI=1.21–2.70, p=0.004). The association between deployment-acquired TBI and past-30-day suicidality did not reach the threshold for statistical significance (adjusted odds ratio=1.39, 95% CI=0.97–2.01, p=0.076).
Deployment-acquired TBI was associated with increased odds of the composite of any of these past-30-day outcomes (adjusted odds ratio=1.74, 95% CI=1.33–2.27, p<0.0005; see
Table 3). When the composite outcome was rerun stratifying TBI-positive subjects into those with probable “very mild,” “mild,” and “more than mild” concussions, a dose-response relationship between severity of TBI and odds of the composite outcome was observed (adjusted odds ratios=1.57, 1.78, and 4.28 for “very mild,” “mild,” and “more than mild,” respectively; p<0.0005).
Mental Health Outcomes at 9 Months Postdeployment (T3)
At the T3 follow-up, approximately 9 months postredeployment to the United States from Afghanistan, past-30-day DSM-IV PTSD was reported by 11.7% (SE=0.5%) of soldiers. The mean PTSD Checklist score at T3 was 25.79 (SD=12.70; median=19, interquartile range=17–30).
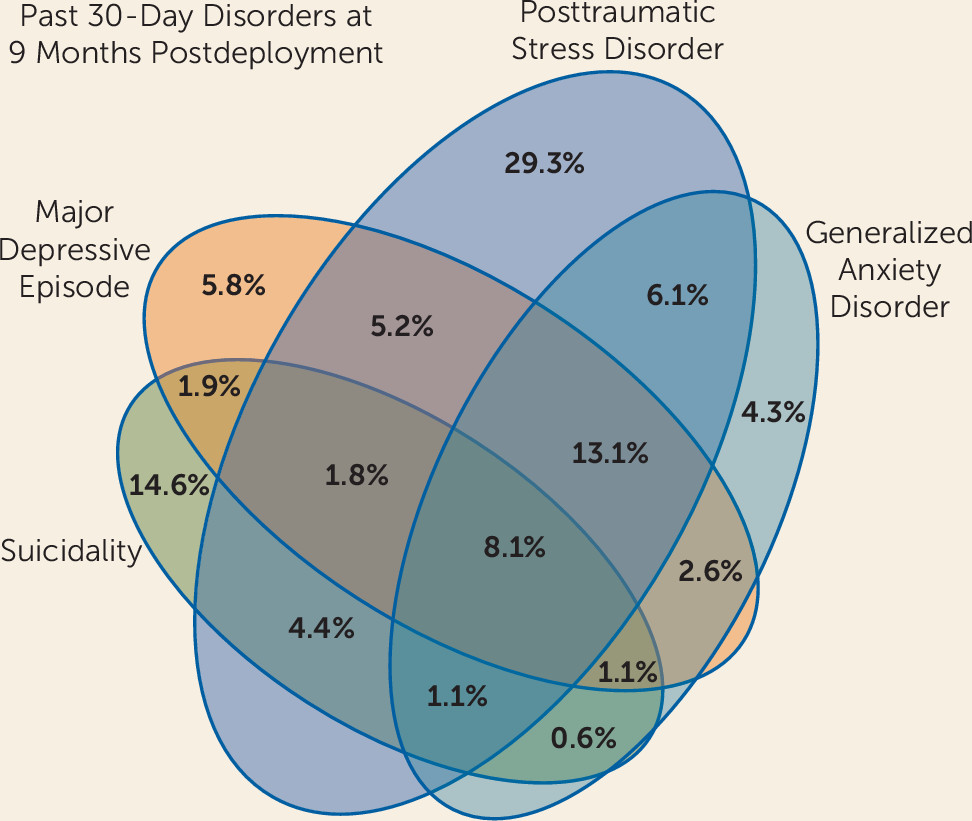
Past-30-day prevalence of other mental disorders at T3 was 6.7% (SE=0.3%) for major depressive episode, 6.2% (SE=0.4%) for generalized anxiety disorder, and 5.7% (SE=0.4%) for suicidality. The combined prevalence of any past-30-day PTSD, major depressive episode, generalized anxiety disorder, or suicidality at T3 was 16.8% (SE=0.6%; see
Figure 2 for depiction of comorbidity rates). The mean general distress score at T3 was 14.32 (SD=18.12; median=6, interquartile range=2–21).
Association of deployment-acquired TBI with posttraumatic stress outcomes.
In a logistic regression analysis adjusting for age group, sex, ethnicity, race, Brigade Combat Team, number of prior deployments, predeployment TBI history, lifetime PTSD predeployment, PTSD symptoms at baseline (6-item PTSD Checklist score at T0), and deployment stress severity, deployment-acquired TBI was strongly associated with increased odds of past-30-day PTSD at 9 months postdeployment (T3) (adjusted odds ratio=1.48, 95% CI=1.21–1.83, p<0.0005; see
Table 1).
When the above model was rerun stratifying TBI-positive subjects into those with probable “very mild,” “mild,” and “more-than-mild” concussions, a dose-response relationship with TBI severity was seen such that increasing severity of TBI was associated with increasing odds of T3 past-30-day PTSD (adjusted odds ratios=1.21, 1.78, and 4.49 for “very mild,” “mild,” and “more than mild,” respectively; p<0.0005). However, the adjusted odds ratio for “very mild TBI” (1.21) was not significantly elevated relative to the “no TBI” reference group (p=0.13).
Whereas the previous models evaluated presence or absence of PTSD as a dichotomous outcome, we also evaluated whether deployment-acquired TBI was associated with increased PTSD symptoms at T3. Having sustained a TBI during the index deployment was associated with increased odds of a nonzero score on the PTSD Checklist (i.e., having some PTSD symptoms versus none; adjusted odds ratio=1.82, 95% CI=1.22–2.70, p=0.005) and a 1.20-fold increase in PTSD Checklist score when symptoms were present (i.e., when the PTSD Checklist score was nonzero; fold change=1.20, 95% CI=1.10–1.31, p<0.001; see
Table 2).
Association of deployment-acquired TBI with other mental health outcomes.
In logistic regression analyses adjusting for age group, sex, ethnicity, race, Brigade Combat Team, number of prior deployments, lifetime history of the outcome in question (major depressive episode, generalized anxiety disorder, or suicidality) predeployment (T0), general distress predeployment (T0), and deployment stress severity, deployment-acquired TBI was associated with postdeployment (T3) risk of past-30-day generalized anxiety disorder (adjusted odds ratio=1.81, 95% CI=1.21–2.70, p<0.0005). The association of deployment-acquired TBI with T3 past-30-day major depressive episode did not reach statistical significance (adjusted odds ratio=1.28, 95% CI=0.97–1.69, p=0.08), nor was its association with T3 past-30-day suicidality significant (adjusted odds ratio=1.12, 95% CI=0.86–1.46, p=0.40).
Deployment-acquired TBI was associated with the composite of any of these outcomes at T3 (adjusted odds ratio=1.53, 95% CI=1.29–1.82, p<0.0005; see
Table 3). When the composite outcome was rerun stratifying TBI-positive subjects into those with probable “very mild,” “mild,” and “more-than-mild” concussions, a dose-response relationship with TBI severity was seen such that increasing severity of TBI was associated with increasing odds of T3 past-30-day composite of these outcomes (adjusted odds ratios=1.28, 1.87, and 4.22, p<0.0005, for “very mild,” “mild,” and “more than mild,” respectively).
Discussion
Consistent with studies of individuals who sustained traumatic injury in civilian settings (
16,
23,
24), we found evidence from this large, prospective military cohort study that deployment-acquired TBI is associated with substantially increased risk for having PTSD at 3 and 9 months postdeployment. This association was robust across models that adjusted for multiple concurrent risk factors (particularly lifetime PTSD, baseline PTSD symptoms, prior TBI history and deployment stress severity) and that considered multiple indicators of the outcome of interest (PTSD diagnosis; presence and severity of PTSD symptoms). These findings converge with results of considerable observational research that has shown mild TBI to be among the most salient risk factors for the development of PTSD (
3,
14,
15).
Few studies have attempted to investigate the impact of TBI severity on subsequent mental health outcomes. However, a recent study of military personnel found that blast-related mild TBI with loss of consciousness (versus no loss of consciousness) was associated with increased risk for PTSD (
25). An Israeli study of civilian motor vehicle collision survivors with head injuries similarly found that the risk of PTSD was increased if the injury included loss of consciousness (
26). We found a dose-response relationship between “very mild” (dazed but no loss of consciousness or amnesia), “mild” (some loss of consciousness or amnesia), and “more-than-mild” TBI and the observed outcomes. More-than-mild TBI was associated with the greatest elevations of risk for PTSD and the composite outcome of any PTSD, major depressive episode, generalized anxiety disorder, or suicidality, with odds ratios reflecting approximately 4 times greater risk relative to those without deployment-acquired TBI. Mild TBI conveyed an intermediate elevation of risk for the same outcomes, with odds ratios suggesting a near-doubling of risk relative to those without deployment-acquired TBI. Very mild TBI was also associated with increased odds of PTSD and the composite outcome; however, the elevation of risk was smaller in magnitude (range of adjusted odds ratios=1.21–1.66) and, in the case of PTSD, was only statistically significant at T2.
Some TBI studies suggest that memory of the traumatic event increases risk for PTSD (
27). Our results stand in contrast with that observation, in that risk for PTSD became more elevated as TBI severity (including extent of amnesia) increased. The impact of trauma memory on PTSD risk merits further study; however, it seems clear that PTSD can, indeed, occur after TBI characterized by incomplete or partial memories of the injury or postinjury period (including disorienting and painful medical procedures, such as those that may occur during intensive care unit stays) (
28).
The present findings related to TBI severity further suggest that extent of injury to the brain moderates the likelihood of the development of mental health sequelae. This is hardly a radical notion, as considerable neuroimaging and neuropsychological research supports a model wherein TBI impairs functioning of prefrontocortical and networked systems that are believed to be integral for inhibiting fear responses and promoting fear extinction (
29). But there also exists a contrarian view that concussions increase risk for mental disorders not by virtue of their mechanical impact on the brain, per se, but rather by their emotional impact on the individual’s psyche as a result of their occurrence within a potentially life-threatening and otherwise stressful context (i.e., military combat) (
30). Which of these accounts is most true—and it is likely that both have explanatory power—remains to be determined by future studies that can more accurately gauge these factors (i.e., extent of physical and emotional injury) and disaggregate their effects.
Another important finding from the present study is the observation that whereas PTSD is, indeed, a frequent consequence of deployment-acquired TBI, so are other mental disorders. In addition to PTSD, postdeployment major depressive episode and generalized anxiety disorder were both significantly associated with deployment-acquired TBI. These data are again consistent with the aforementioned study of civilian traumatic injury survivors (
16), where TBI was associated with increased incidence of multiple psychiatric disorders. These observations highlight the myriad mental health sequelae of TBI (
29) and indicate that surveillance must extend beyond the relatively narrow framework of PTSD. It is evident that mental disorder incidence following TBI is sufficiently high that routine screening might be worth implementing (
7), but precisely if, how, and when to conduct such screening remains to be empirically determined. Moreover, researchers have begun to recognize that symptoms and impairment post-TBI do not neatly fall into any one diagnostic psychiatric or neurologic (including postconcussive syndrome) category (
23) and that much additional work will be needed to characterize and classify the full and complex range of cognitive, emotional, and behavioral symptoms that can occur.
Suicidality has until very recently been an understudied potential consequence of TBI. A large Swedish population-based study found that TBI was associated with a threefold increased risk of suicide compared with the adjusted risk in the general population (
31). A study of 161 U.S. military personnel referred to a TBI clinic in Iraq for suspected head injury found that multiple episodes of TBI, which were common among U.S. military personnel, were associated with increased risk for lifetime suicidal thoughts and behaviors, as well as for current suicidal ideation (
11). Baseline assessment of the Veterans After-Discharge Longitudinal Registry (Project VALOR), an observational registry of over 1,600 veterans with and without PTSD who deployed in support of the wars in Iraq and Afghanistan and were enrolled in the Veterans Affairs health care system, found that a history of TBI was associated with increased risk for current suicidal ideation, though only in men (
9). The present longitudinal cohort study failed to clearly demonstrate an increase in risk for suicidality in individuals who sustained TBI during deployment. Whereas a modest, nearly significant association was seen at 3 months postdeployment, by the 9-month follow-up this association was no longer evident. It may be that suicidality should be a greater concern for the first few months postconcussion but that this risk may wane with time. Additional longitudinal research will be required to resolve this question. Thus, although inconclusive, these data call for increased attention to TBI, along with what is already known about other susceptibility factors such as pre-existing mental disorders (
32,
33), as a potentially modifiable risk factor for suicide among military personnel.
Strengths of this study are its large sample size and its detailed, systematic longitudinal prospective assessment of three Army Brigade Combat Teams about to be deployed to Afghanistan. A limitation is that diagnostic data were collected by self-report rather than by direct clinical interviews, but this is mitigated by the extensive testing and clinical calibration of our diagnostic measures (
21). A second limitation is that information about the main exposure of interest, TBI, was obtained by self-report and further lacked specification about presumed mechanism of injury (e.g., blast versus impact). Studies show, however, that mild TBIs are often medically undiagnosed (
1,
34) or underreported (
35), and our own attempts to corroborate TBI self-reports with military medical records revealed poor concordance (data not shown). The presence of a dose-response relationship between severity of self-reported TBI—even within the mild spectrum—and the outcomes of interest provides some reassurance that the observed associations are valid. Nonetheless, future studies that can more deliberately and deeply debrief participants about the circumstances of their TBI(s) are needed. A third limitation is that the nature of our survey, wherein we tracked soldiers within their Brigade Combat Teams, would have resulted in very few cases of moderate or severe TBI being included, as many if not most of those soldiers would have been hospitalized and probably inaccessible to us for the follow-up assessments. Accordingly, it is important to recognize that this study is, essentially, a study of persons with a range of TBI severity within the mild spectrum. A fourth limitation is the unavailability of survey data about other concurrent physical injury that respondents may have sustained. It is well established that extent and severity of physical injury increases risk for PTSD (
36). It is therefore possible that those with TBIs may have also had more serious nonhead injuries than other soldiers and that an increased aggregate burden of injury may have contributed to the observed increase in PTSD and related disorders in those individuals. This hypothesis can be tested in future studies with access to more granular data about the type, timing, and extent of physical injuries sustained.
In summary, we found in this large, prospective cohort study of military personnel about to be deployed to Afghanistan that mild TBI is common during deployment and that it is associated with substantially increased risk for PTSD observed 3 and 9 months after redeployment to the United States. We also found that the risk for mental health problems following mild TBI is not restricted to PTSD, implying that the focus on surveillance and intervention needs to be broadened to include other anxiety and depressive disorders. Finally, the process(es) by which mild TBI increases risk for these disorders, which may include inflammatory or other neurodegenerative etiologies that impair brain network function (
37–
39), perhaps especially involving systems that mediate executive functioning (
40), should be further studied in order to arrive at more mechanistic approaches to prevention and treatment.
Acknowledgments
The Army STARRS team consists of Co-Principal Investigators: Robert J. Ursano, M.D., (Uniformed Services University of the Health Sciences) and Murray B. Stein, M.D., M.P.H. (University of California San Diego and VA San Diego Healthcare System); Site Principal Investigators: Steven Heeringa, Ph.D. (University of Michigan) and Ronald C. Kessler, Ph.D. (Harvard Medical School); National Institute of Mental Health (NIMH) collaborating scientists: Lisa J. Colpe, Ph.D., M.P.H., and Michael Schoenbaum, Ph.D.; Army liaisons/consultants: Col. Steven Cersovsky, M.D., M.P.H. (USAPHC) and Kenneth Cox, M.D., M.P.H. (USAPHC); Other team members: Pablo A. Aliaga, M.A. (Uniformed Services University of the Health Sciences); Col. David M. Benedek, M.D. (Uniformed Services University of the Health Sciences); K. Nikki Benevides, M.A. (Uniformed Services University of the Health Sciences); Paul D. Bliese, Ph.D. (University of South Carolina); Susan Borja, Ph.D. (NIMH); Evelyn J. Bromet, Ph.D. (Stony Brook University School of Medicine); Gregory G. Brown, Ph.D. (University of California San Diego); Christina Buckley, B.A. (Uniformed Services University of the Health Sciences); Laura Campbell-Sills, Ph.D. (University of California San Diego); Catherine L. Dempsey, Ph.D., M.P.H. (Uniformed Services University of the Health Sciences); Carol S. Fullerton, Ph.D. (Uniformed Services University of the Health Sciences); Nancy Gebler, M.A. (University of Michigan); Robert K. Gifford, Ph.D. (Uniformed Services University of the Health Sciences); Stephen E. Gilman, Sc.D. (Harvard School of Public Health); Marjan G. Holloway, Ph.D. (Uniformed Services University of the Health Sciences); Paul E. Hurwitz, M.P.H. (Uniformed Services University of the Health Sciences); Sonia Jain, Ph.D. (University of California San Diego); Tzu-Cheg Kao, Ph.D. (Uniformed Services University of the Health Sciences); Karestan C. Koenen, Ph.D. (Columbia University); Lisa Lewandowski-Romps, Ph.D. (University of Michigan); Holly Herberman Mash, Ph.D. (Uniformed Services University of the Health Sciences); James E. McCarroll, Ph.D., M.P.H. (Uniformed Services University of the Health Sciences); James A. Naifeh, Ph.D. (Uniformed Services University of the Health Sciences); Tsz Hin Hinz Ng, M.P.H. (Uniformed Services University of the Health Sciences); Matthew K. Nock, Ph.D. (Harvard University); Rema Raman, Ph.D. (University of California San Diego); Holly J. Ramsawh, Ph.D. (Uniformed Services University of the Health Sciences); Anthony Joseph Rosellini, Ph.D. (Harvard Medical School); Nancy A. Sampson, B.A. (Harvard Medical School); LCDR Patcho Santiago, M.D., M.P.H. (Uniformed Services University of the Health Sciences); Michaelle Scanlon, M.B.A. (NIMH); Jordan W. Smoller, M.D., Sc.D. (Harvard Medical School); Amy Street, Ph.D. (Boston University School of Medicine); Michael L. Thomas, Ph.D. (University of California San Diego); Patti L. Vegella, M.S., M.A. (Uniformed Services University of the Health Sciences); Leming Wang, M.S. (Uniformed Services University of the Health Sciences); Christina L. Wassel, Ph.D. (University of Pittsburgh); Simon Wessely, F.Med.Sci. (King’s College London); Hongyan Wu, M.P.H. (Uniformed Services University of the Health Sciences); LTC Gary H. Wynn, M.D. (Uniformed Services University of the Health Sciences); Alan M. Zaslavsky, Ph.D. (Harvard Medical School); and Bailey G. Zhang, M.S. (Uniformed Services University of the Health Sciences).