The pervasive developmental disorders (autistic disorder, pervasive developmental disorder not otherwise specified, and Asperger’s syndrome) defined in DSM-IV (
1) have been subsumed under the single diagnostic category of autism spectrum disorder (ASD) in DSM-5 (
2). A recent detailed review of epidemiological studies estimates an ASD prevalence of 6.2 per 1,000 children worldwide (
3). Of these, 30%−40% are intellectually disabled (
3).
In addition to essential diagnostic characteristics, children with ASD may exhibit serious behavioral problems such as tantrums, aggression and self-injury (
4), and anxiety (
5), as well as hyperactivity, impulsiveness, and distractibility (
6–
8). Although DSM-IV advised against giving a diagnosis of attention deficit hyperactivity disorder (ADHD) to children with ASD (
1), DSM-5 discarded this convention (
2). When present, hyperactivity, impulsiveness, and distractibility add to the overall impairment in children with ASD (
9). Not surprisingly, stimulants and alpha
2 agonists are commonly used to treat ADHD symptoms in children with ASD (
10).
Few studies have rigorously tested treatments of ADHD symptoms in children with ASD. The alpha
2 agonists clonidine and guanfacine have been evaluated in open and small randomized trials among children with ASD, with inconclusive results on efficacy and recurring problems with sedation and irritability (
11). Using a double-blind crossover design, our research group previously tested three dose levels of immediate-release methylphenidate in 72 children with ASD (
12). All three dose levels of methylphenidate were superior to placebo, with score reductions of small to medium effect sizes on the Aberrant Behavior Checklist-hyperactivity subscale. The overall positive response rate on the Clinical Global Impression–Improvement (CGI-I) scale of 49% was lower than the 65%−70% positive response rate in children with ADHD uncomplicated by ASD (
13,
14). Furthermore, adverse effects occurred at higher than expected rates in children with ASD compared with children with ADHD uncomplicated by ASD (
12,
14). Harfterkamp et al. (
15) reported equivocal results in an 8-week placebo-controlled trial of atomoxetine in 97 children with ASD and ADHD symptoms. Collectively, these results suggest that additional pharmacological strategies are needed for children with ASD and ADHD symptoms for whom stimulants are not effective or intolerable. We previously conducted an open-label trial of immediate-release guanfacine in 25 subjects with a recent history of failed treatment with methylphenidate. In that study, we observed a 39% reduction on the Aberrant Behavior Checklist hyperactivity subscale and a 48% (12 of 25) positive response rate on the improvement item of the CGI (
16,
17). The purpose of the present study was to test whether extended-release guanfacine would be superior to placebo in children with an ASD accompanied by moderate to severe hyperactivity.
Method
Design
This was a five-site randomized, double-blind placebo-controlled, fixed-flexible dose clinical trial conducted by the Research Units on Pediatric Psychopharmacology Autism Network. Using permuted blocks to conceal allocation, eligible subjects were randomly assigned within site without stratification in a 1:1 ratio to extended-release guanfacine or placebo for 8 weeks. At week 8, subjects who met predetermined criteria for positive response (see below) in the double-blind phase continued with their randomized treatment (extended-release guanfacine or placebo) for 8 more weeks without breaking the treatment mask. The treatment blind was broken for subjects who did not show a positive response. Subjects who were randomly assigned to placebo and did not show a positive response were offered open-label treatment with extended-release guanfacine for 8 weeks. Subjects who showed insufficient response to guanfacine in the double-blind phase were tapered off the medication and managed outside of the study. This report focuses on the results of the acute double-blind phase.
Setting and Subjects
The study was approved by the institutional review board at each site (University of California at Los Angeles, Emory University, Massachusetts General Hospital, University of Washington at Seattle, and Yale University) and registered with Clinicaltrials.gov (NCT01238575). Study subjects were recruited from clinic registries, current referrals to the active clinical programs at each site, local website announcements, and outreach to parent support groups. No study data were collected until a parent (or guardian) signed the informed consent. Protocol adherence was monitored through weekly teleconferences with the principal investigators and coordinators. The coordinating centers (Yale University and Emory University) conducted semiannual site visits and managed study data. An external data, safety, and monitoring board reviewed safety, enrollment, and attrition three times a year.
An experienced multidisciplinary team at each site conducted the screening, baseline, and follow-up assessments. To be eligible, subjects had to be between 5 and 14 years of age with a DSM-IV diagnosis of autistic disorder, Asperger’s syndrome, or pervasive developmental disorder not otherwise specified, based on clinical assessment and corroborated by the Autism Diagnostic Observation Schedule (
18) and the Social Communication Questionnaire (
19). The Autism Diagnostic Observation Schedule is a clinician-administered procedure that places the child in naturalistic social situations designed to elicit social and communication responses. The Social Communication Questionnaire is a 40-item parent-completed survey that evaluates the child’s communication and social functioning. The lifetime version of the questionnaire provides a total score that can be compared against normative data as further support for an ASD diagnosis. The pretreatment assessment also included routine laboratory tests (blood counts, electrolytes, liver function tests, blood urea nitrogen, creatinine, and urinalysis), medical and psychiatric histories, a physical examination, and vital sign evaluation. The screening and week-8 ECG were reviewed by a pediatric cardiologist at each site.
The primary targets of the treatment were hyperactivity, impulsiveness, and distractibility. Therefore, we set a minimum score of 24 on the parent-rated Aberrant Behavior Checklist-hyperactivity subscale for study eligibility (see below). In addition, a Clinical Global Impression-Severity (CGI-S) score of moderate or greater was required for entry. The CGI is a 7-item scale, which ranges from 1 (normal) through 4 (moderate) to 7 (extreme), designed to rate overall symptom severity (
17). In addition to hyperactivity, impulsiveness, and distractibility, raters considered all aspects of the child’s clinical picture to assign the CGI-S score.
Based on the Abbreviated Stanford-Binet Intelligence Scales (
20) or the Mullen Scales of Early Learning (
21), subjects had to have an IQ of 35 (or mental age of 18 months) or greater. Anticonvulsant medication for seizures was allowed if the dose was stable (at least 4 weeks) and the subject was seizure-free for at least 6 months. Otherwise, subjects had to be medication-free prior to baseline. Subjects taking a psychotropic treatment deemed ineffective were required to be withdrawn from the medication for at least 1 week for stimulants or clonidine, 2 weeks for atomoxetine and most antidepressants, and 3 weeks for fluoxetine, citalopram, and antipsychotics. Children with a significant medical condition by history, physical examination, or laboratory testing were excluded. Girls with a positive pregnancy test were also excluded.
To screen for other DSM-IV disorders, we relied on clinical evaluation supplemented by the parent-completed Child and Adolescent Symptom Inventory (
22). This 132-item DSM-IV-based checklist asks parents to rate symptoms in the major psychiatric disorders of childhood on a 4-point scale (0=never; 1=sometimes; 2=often; and 3=very often). Scores of 2 or 3 are regarded as a positive symptom for the given disorder. Children with a lifetime diagnosis of psychosis or bipolar disorder or current diagnosis of major depression, obsessive-compulsive disorder, or substance abuse were excluded. To assess adaptive functioning at baseline, we used the parent-rated Vineland Adaptive Behavior Scales II (Vineland II) (
23). The Vineland II provides standard scores in three domains: communication, socialization, and daily living skills. Prior to administration, parents were instructed to consider adaptive skills that the child is unable to perform (score of 0); skills that the child performs sometimes (score of 1); and skills that the child regularly performs (score of 2).
Outcome Measures
The primary outcome measure was the parent-rated Aberrant Behavior Checklist-hyperactivity subscale (
9,
24,
25). The full Aberrant Behavior Checklist is a 58-item parent rating with five factors: irritability, social withdrawal, stereotypy, hyperactivity, and inappropriate speech. The 16-item hyperactivity subscale (collected at baseline, weeks 4, 6, and 8) covers over-activity (seven items), impulsiveness (two items), inattention (three items), and noncompliance (four items). It has been used as a primary outcome measure in several trials of children with developmental disabilities (
12,
16).
Two blinded clinicians followed each subject: a treating clinician and an independent evaluator. The treating clinician adjusted the dose of the medication and monitored adverse events. The independent evaluator assessed key secondary outcomes, including scores for the improvement item of the CGI (
17) and the ADHD Rating Scale (
26). To protect the blind, the independent evaluator did not discuss adverse effects or dosing. The ADHD Rating Scale is an 18-item scale directly derived from DSM-IV criteria for ADHD with established reliability, validity, and sensitivity to change (
26–
28). The CGI-I is a 7-point scale designed to measure overall symptomatic change compared with baseline. Scores range from 1 (very much improved) through 4 (unchanged) to 7 (very much worse). A rating of much improved or very much improved on the CGI-I at week 8 was used to define positive response. As noted, the treatment mask was broken for subjects who did not show a positive response. The blind was broken by the treating clinician, and treatment status was not disclosed to independent evaluators.
Experienced investigators (L.S., B.K.) trained study independent evaluators on the CGI (severity and improvement) using case vignettes for illustration and discussion. To be considered reliable, raters had to be in full agreement on the CGI (severity and improvement) with the gold standard score on at least one vignette. In addition, independent evaluators had to be within one unit of the gold standard without disagreement on study eligibility or treatment response on two other vignettes. For example, if the gold standard baseline CGI-S was moderate (4) and the new rater gave a score of mild (3), this one unit difference would affect eligibility and was considered unreliable. Similarly, on the CGI-I, if the gold standard score was 2 (much improved) and the new rater gave a score of 3 (minimally improved), this was unacceptable because of the disagreement on classification. Independent evaluators also received training on the administration of the ADHD Rating Scale and had to be within 4 points on two video recordings compared with the expert rater. Independent evaluators participated in monthly conference calls to review cases and to promote a common approach to conducting assessments across sites.
Four cognitive tests were administered at baseline and week 8 by psychologists who were trained to reliability and blind to treatment assignment. The tests included the Recognition of Pictures and Digit Recall subtests from the Differential Ability Scales II (
29) and the Imitating Hand Positions and Manual Motor Sequences from the sensorimotor domain of the NEPSY II (
30). To assess working memory, the Recognition of Pictures presents pictures of objects for 5–10 seconds to the child. The examiner then presents a new page with the same objects mixed with distracter pictures and asks the child to point to the original objects. The Recall of Digits is also a working memory task in which the child is asked to repeat a sequence of digits presented orally by the examiner. Sequences start with two digits and increase progressively up to nine digits or until the child meets the discontinuation rule. The Imitating Hand Positions test assesses motor planning by asking the child to imitate the examiner’s hand and finger positions with the dominant hand, nondominant hand, and both hands. The Manual Motor Sequences task measures the ability of the child to imitate a series of rhythmic movements by the examiner using one or both hands.
Medication Schedule
The extended-release guanfacine formulation is undermined if the tablets are crushed or broken. Thus, we confirmed that each subject was able to swallow the whole tablet. The starting morning dose for all children was 1 mg per day. Children weighing less than 25 kg remained on the 1-mg dose until day 14. If the medication was well-tolerated, the dose could be raised to 2 mg until day 28 and increased to 3 mg for the remaining 4 weeks in the trial. Children weighing 25 kg or more were eligible for an increase to 2 mg at day 7, 3 mg at day 14, and 4 mg at day 21 or day 28. The dose schedule was not fixed; the treating clinician could delay a planned increase or lower the dose to manage adverse effects. The treating clinician could also switch to an evening dose to manage daytime drowsiness.
Safety Monitoring
Subjects were seen weekly for the first 4 weeks, then at weeks 6 and 8. Blood pressure and pulse sitting at rest and height and weight were measured at each visit. Routine laboratory tests were not repeated at week 8 in the absence of evidence that guanfacine affects these indices (
31,
32). An ECG was obtained at week 8 (or early termination) to assess the impact of guanfacine on cardiac conduction.
Adverse events were also systematically reviewed and documented at each visit. At baseline, the treating clinician conducted the 34-item Pretreatment Health and Behavior Review, developed by the Research Units on Pediatric Psychopharmacology Autism Network (
4,
12), to collect pretreatment data on mild, moderate, or severe health complaints, as well as activity level, appetite, bowel function, sleep, and dermatological problems. Following a similar format, the treating clinician reviewed the 34-item Adverse Event Review to identify new adverse effects after random assignment. New adverse events, whether presumed related to treatment or not, were rated as mild (no impairment), moderate (some impairment or need for intervention to prevent impairment), severe (evidence of impairment and need for intervention), serious (need for hospitalization or major threat to health and well-being). A decrease of 10 mm of Hg in diastolic blood pressure or a shift into the abnormal range (i.e., >2 standard deviations below the normal range for age and gender) was documented as an adverse event. For these subjects, blood pressure was repeated after a 5- to 10-minute resting period. If the 10-mm drop in the diastolic blood pressure persisted on repeat measurement during the same visit, the dose was reduced.
Analytic Plan
The population mean score on the Aberrant Behavior Checklist-hyperactivity subscale for developmentally disabled boys in this age group was 13 (SD=11.3) (slightly lower for girls). Study eligibility required a medication-free Aberrant Behavior Checklist-hyperactivity subscale score >24. To estimate sample size, we predicted a mean hyperactivity subscale score at baseline of 30 (SD=10) (approximately 1.5 standard deviations above the population mean). Based on previous studies, we predicted incremental, linear improvement for extended-release guanfacine over time. We estimated the power to detect a clinically meaningful effect size of 0.55 across a range of sample sizes in a series of simulations using a random regression model. To estimate the correlation of repeated parent-rated Aberrant Behavior Checklist-hyperactivity subscale scores, we used data from subjects randomly assigned to placebo in our previous trial comparing risperidone with placebo (
4). The correlations ranged from 0.63–0.85 over that 8-week trial. For the linear trend hypothesis, a sample size of 60 provided 85.5% power assuming a test-retest correlation of 0.7 on the Aberrant Behavior Checklist-hyperactivity subscale. Power would be slightly reduced if the correlation were 0.63 and greater if the correlation were 0.8.
All randomly assigned subjects were included in the intent-to-treat analyses. Preliminary analyses included descriptive statistics for baseline measures in each treatment group, as well as examination of scores within each group at weeks 4 and 8. To evaluate the effect of treatment over time, we used a mixed-effect linear model on the primary outcome measure (parent-rated Aberrant Behavior Checklist-hyperactivity subscale). Study group and site were the fixed effects; time and outcome were the random effects (
33). Using the baseline Aberrant Behavior Checklist-hyperactivity subscale score as a fixed effect in the model, each subject’s response was modeled by regressing the score against time. The intercept and slope of the regression were allowed to vary randomly between subjects. A linear contrast of group differences at 8 weeks (i.e., clinical response) was performed and tested for statistical significance. We used a similar approach for the key secondary outcome, the ADHD Rating Scale score collected at baseline, week 4, and week 8. To evaluate overall improvement, we compared the proportion of subjects rated as much improved or very much improved on the CGI-I by the independent evaluator in each treatment group using chi-square analysis.
All analyses were conducted using SAS/STAT software, version 9.3. In addition, p values ≤0.05 were accepted as statistically significant for the Aberrant Behavior Checklist-hyperactivity subscale, the ADHD Rating Scale, and the CGI-I, with Bonferroni correction for other Aberrant Behavior Checklist subscales. The analysis proceeded on the assumption that missing data were missing at random. Although there is no proven method for verifying this assumption, we compared selected demographic and clinical characteristics of subjects who dropped out with these characteristics in the remaining sample (
34). The rate of adverse effects greater than 5% was compared across treatment groups by chi-square analysis; p values ≤0.10 were considered statistically significant for adverse events.
Results
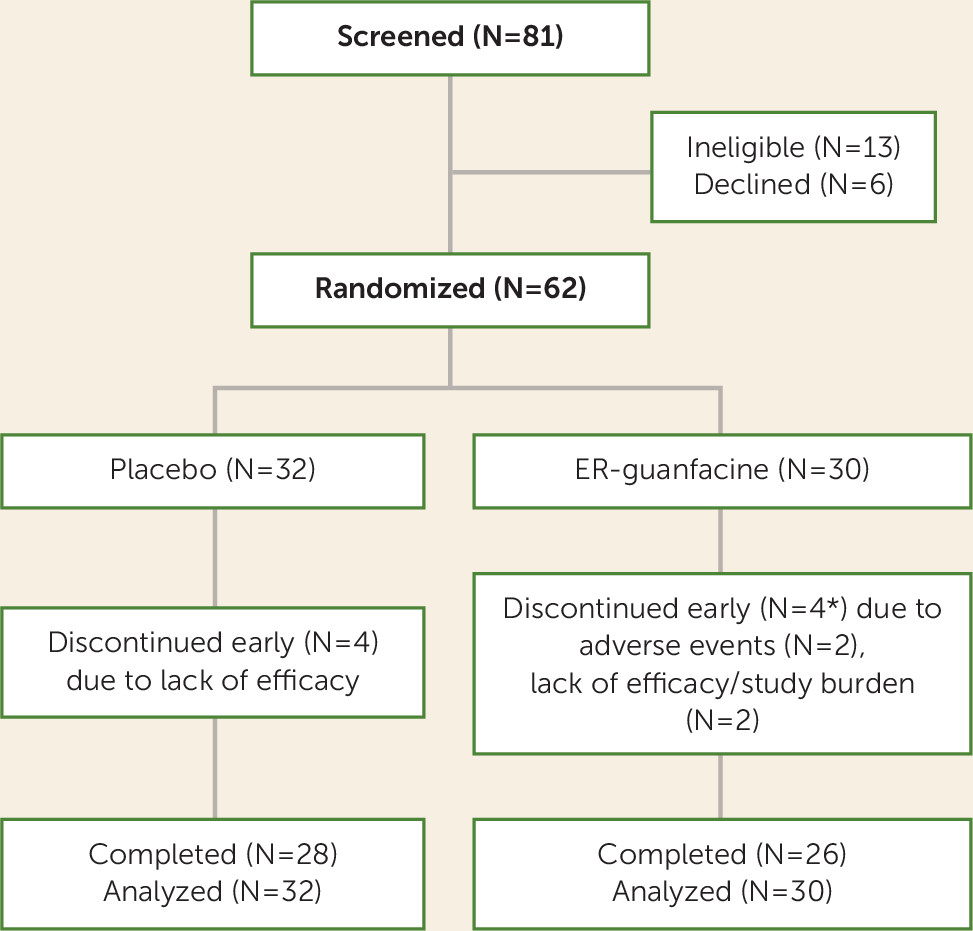
Eighty-one children were screened; 62 (boys, N=53; girls, N=9) eligible subjects were randomly assigned to extended-release guanfacine (N=30) or placebo (N=32) (
Figure 1). Subjects ranged in age from 5 to 14 years (mean=8.5 years [SD=2.25]). There were no differences in demographic and clinical characteristics between treatment groups (see
Table 1). Eight subjects (12.9%) dropped out before week 8 (four from each group). The demographic and baseline clinical characteristics for these eight subjects were not different than these characteristics for the 54 subjects who completed the trial. Thirty-four subjects (54.8%) were drug naive. Twenty-six children (41.9%) were medication-free at screening but had been treated with various medications in the past. In collaboration with the child’s primary clinician, parents decided to discontinue a current medication for two subjects (3.2%). One subject entered following a 3-week washout of fluoxetine, and one entered following a 4-week washout of aripiprazole.
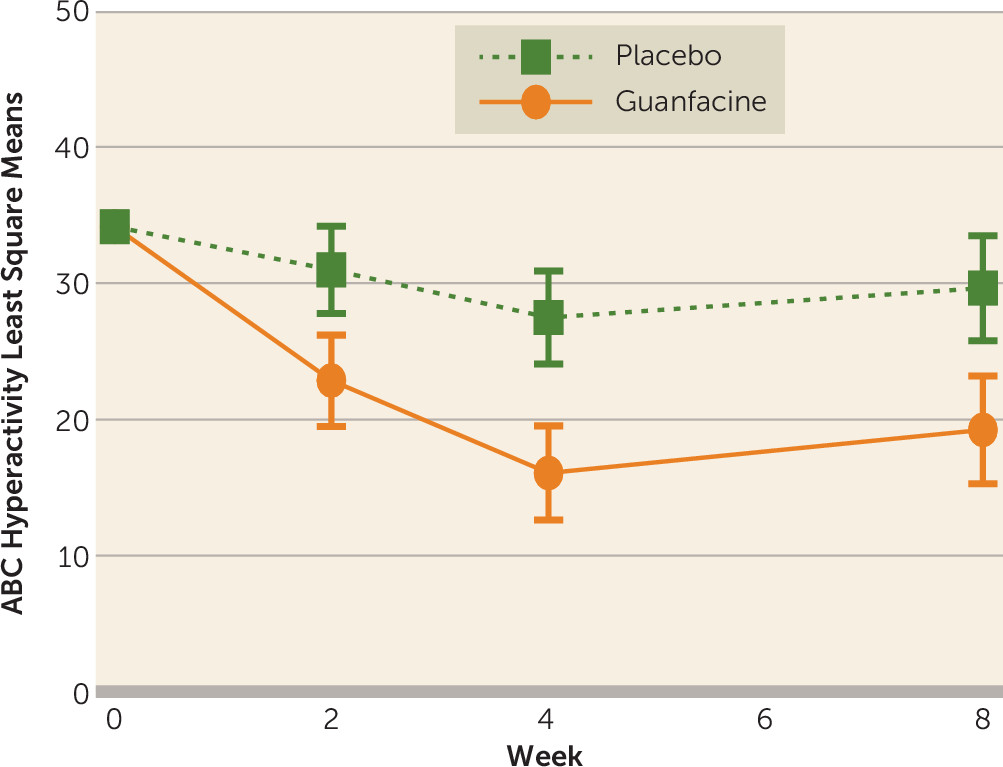
Table 2 shows that guanfacine was superior to placebo on the parent-rated Aberrant Behavior Checklist-hyperactivity subscale (p<0.001, effect size=1.67) and the clinician-rated ADHD Rating Scale (p<0.001 for all three measures). The change in the least-squares means on the Aberrant Behavior Checklist-hyperactivity subscale over the 8-week trial is presented in
Figure 2. The guanfacine group showed a 43.6% decline in the Aberrant Behavior Checklist-hyperactivity subscale score (least-squares mean values were 34.2 at baseline to 19.3 at week 8) compared with a 13.2% decrease for placebo (34.2 at baseline to 29.7 at week 8, p<0.001). The rate of positive response (much improved or very much improved on the CGI-I) was 50% (N=15/30) for guanfacine compared with 9.4% (N=3/32) for placebo (p=0.0001; number needed to treat=2). Baseline and week 8 scores on all Aberrant Behavior Checklist subscales are presented in
Table 2. The extended-release guanfacine group showed modest benefit on the Aberrant Behavior Checklist-stereotypy and inappropriate speech subscales (the latter remained significant after Bonferroni correction).
Cognitive Testing
Fifty-nine of 62 subjects had some cognitive testing results. Among those 59, complete data were available for 51 children, with no difference in missing data across treatment groups. Performance scores at baseline and week 8 on the 17 subtests analyzed are presented in
Table 3. There were no group differences at baseline, and analysis of covariance models (adjusted for IQ ≥70 and<70) showed no group differences from baseline to endpoint on any subtests. The interactions between cognitive test scores at baseline and treatment were not significant. Examination on whether performance on any cognitive subtest predicted positive outcome in either treatment group was uninformative.
Medication Dose
The modal daily dose at week 8 was 3 mg/day (range: 1 mg/day–4 mg/day) for the extended-release guanfacine group and 3 mg/day (range: 2 mg/day–4 mg/day) for the placebo group.
Safety Results
The numbers and percentages of subjects with parent-reported mild, moderate, and severe adverse events are shown in
Table 4. The adverse event labels in this table were derived from a list of preferred terms established before launching the study. The items on the Adverse Event Review and verbatim complaints were matched to the preferred terms. There was one serious adverse event in the guanfacine treatment group. Six days after the scheduled increase to 2 mg per day, the child (a 6 year-9-month-old boy) became verbally and physically aggressive toward his mother. The police were summoned, and the boy was taken to the emergency room. Upon evaluation, he was agitated and threatened hospital personnel, and his speech was pressured. The medication was discontinued, and he remained on the child psychiatric inpatient service for 3 days. Upon discharge, he was hyperactive and impulsive (similar to baseline). He was not agitated or aggressive, and his speech was normal in tone and tempo. During the entire episode, there was no change in his sleep. The study medication was discontinued for this subject, but assessments were continued. One other subject in the guanfacine group also stopped treatment with the study drug because of adverse events and remained in the study for assessment. As shown in
Figure 1, two subjects in the guanfacine group dropped out of the study completely because of multiple adverse events (drowsiness, fatigue, mid-sleep awakening, and emotional lability), and two dropped out because of lack of efficacy.
Nine subjects on active medication had a dose reduction because of suspected treatment-related adverse events (e.g., drowsiness, emotional/tearful presentation, irritability, and/or lowered blood pressure). Five placebo-treated subjects had dose adjustments in response to similar complaints. The term irritability reflects the combination of anger outbursts and low frustration tolerance, with disruptive behavior. By contrast, emotional/tearful captures what parents called “emotionally fragile” or “tearful and cranky.” Although less common, sleep disturbance (trouble falling asleep or mid-sleep awakening) also prompted dose reduction.
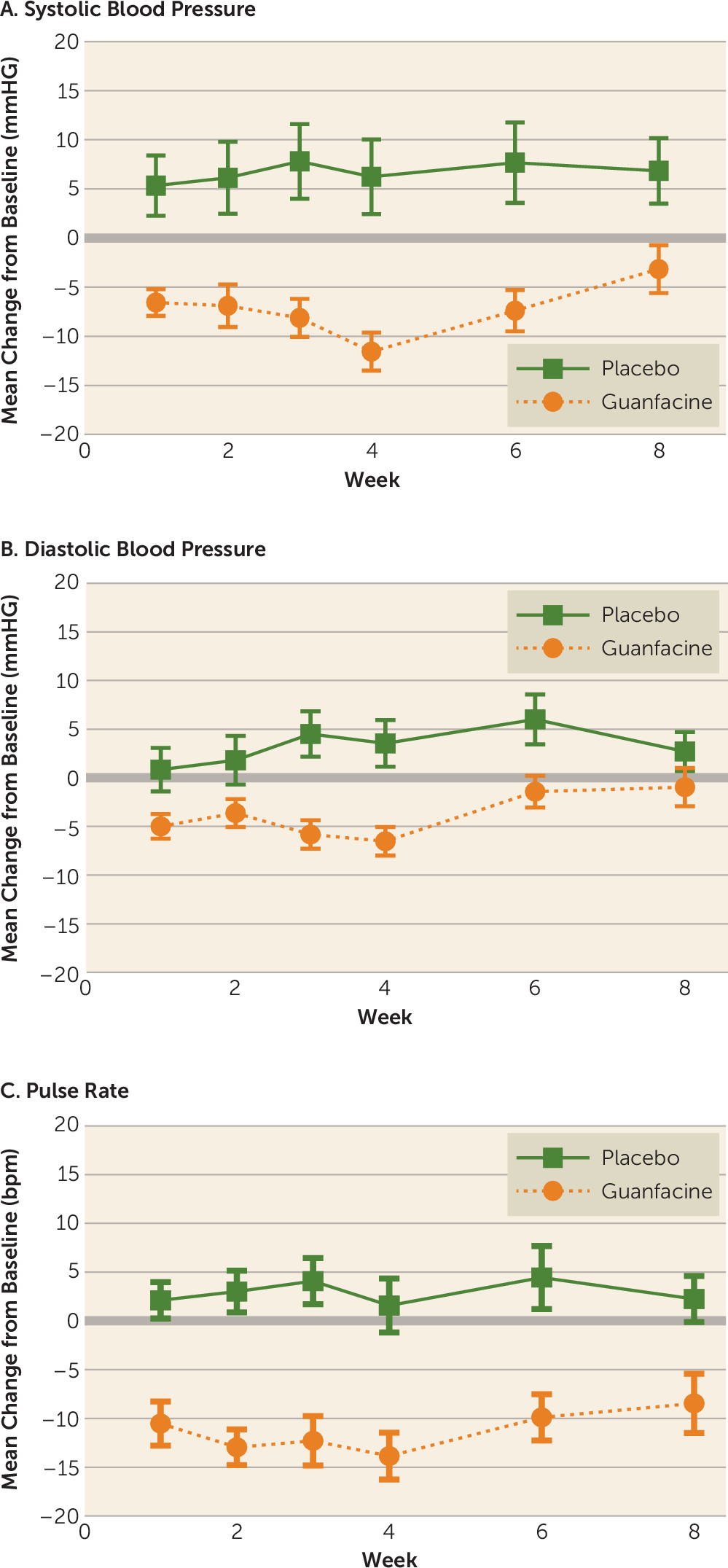
ECG data collected at screening and week 8 were reviewed by a board-certified pediatric cardiologist at each site. Mild, not clinically significant, ECG abnormalities were detected in 12 subjects at baseline and eight subjects at week 8 (active treatment, N=5; placebo, N=3). In guanfacine-treated subjects, sinus bradycardia was the most commonly reported finding. One subject had a borderline QTc prolongation of 461 ms at screening that was considered not clinically significant. At week 8, this subject had a QTc of 465, also considered not clinically significant. No subject had a QRS interval greater than 120 ms, and no other subject had a QTc greater than 450 ms. Systolic and diastolic blood pressure, as well as pulse, for 53 subjects with complete data across the 8-week trial are shown in
Figure 3A,
Figure 3B, and
Figure 3C. Sixteen subjects had a ≥10-point drop in diastolic blood pressure in the guanfacine group compared with nine in the placebo group (p=0.04).
Discussion
Extended-release guanfacine is approved by the U.S. Food and Drug Administration for the treatment of children with ADHD (
28,
30). The results of this trial indicate that extended-release guanfacine is safe and effective for short-term treatment of hyperactivity, impulsiveness, and distractibility in children with ASD. The rate of positive response on the CGI-I is similar to what has been reported in previous trials of extended-release guanfacine in children with ADHD (
28,
30). The results of the present study extend pilot study findings of immediate-release guanfacine in this population (
16,
35). The primary outcome measure (Aberrant Behavior Checklist-hyperactivity subscale) includes items on hyperactivity, impulsiveness, inattention, and noncompliance that do not map directly on an ADHD diagnosis. On the DSM-IV-referenced ADHD Rating Scale (a key secondary measure), however, we also observed significant effects on hyperactivity, impulsiveness, and inattention.
The 43.6% decline in scores (effect size=1.67) on the parent-rated Aberrant Behavior Checklist-hyperactivity subscale from baseline to week 8 in this trial is greater than the 31%–38% reduction (effect sizes ranged from 0.29 to 0.54) across the three fixed-dose levels of methylphenidate in the crossover trial (
12). However, on the predetermined algorithm used to define the optimal dose of methylphenidate, there was a 48% reduction (effect size=0.89) from baseline on the parent-rated Aberrant Behavior Checklist-hyperactivity subscale. The smaller effect size for the optimal dose in the methylphenidate study is due in part to the 22% decline in the placebo group in the prior study compared with a 13% decline in the guanfacine trial. Treatment for four of 30 guanfacine-treated subjects (13.3%) in the present study was discontinued because of adverse events (two remained in the study; two exited the study). By contrast, 18% (13 of 72) subjects discontinued the methylphenidate trial. On the CGI-I, the 50% positive response rate for guanfacine was nearly identical to the rate observed in the methylphenidate trial. Although it is difficult to compare the results of this 8-week parallel trial to the 4-week fixed-dose methylphenidate crossover trial, the magnitude of effect and tolerability appears slightly better for extended-release guanfacine for reducing ADHD symptoms in children with ASD. There are no identified predictors of positive response to either drug. Both drugs require careful monitoring to balance tolerability and benefits.
In the total score of the clinician-administered ADHD Rating Scale, we observed a 34% improvement from baseline to week 8 and a 50% positive response rate on the CGI-I. In an 8-week double-blind placebo-controlled trial of atomoxetine in 97 children with ASD and ADHD symptoms, Harfterkamp et al. (
15) reported a 22% improvement on the ADHD Rating Scale and a 21% positive response rate on the CGI-I. These contrasting results support the selection of extended-release guanfacine over atomoxetine in this clinical population.
The most common adverse events leading to dose reduction with extended-release guanfacine were drowsiness, fatigue, emotional fragility, tearfulness, and irritability. In a 5-week fixed-dose trial (placebo 2, 3, or 4 mg/day) of extended-release guanfacine, Biederman et al. (
28) reported a similar pattern of adverse effects but at lower rates. Similarly, systolic and diastolic blood pressures and pulse declined during the dose escalation phase in the present study, which is consistent with findings in studies of extended-release guanfacine in children with ADHD (
28). Blood pressure readings returned nearly to baseline measurements by week 8 in the present study. Heart rate remained about 10 points below baseline at week 8 in the guanfacine-treated group. There were no clinically significant changes from baseline on the ECG. These results suggest that monitoring blood pressure and pulse is warranted, especially early in treatment.
The alpha
2 agonists guanfacine and clonidine were developed as antihypertensives. The stimulation of presynaptic alpha
2 receptors reduces tonic firing of locus coeruleus neurons, resulting in slower heart rate and decreased blood pressure (
36). A rich body of preclinical evidence indicates that norepinephrine neurons in the locus coeruleus also regulate arousal and play an essential role in interpretation of sensory stimuli and behavioral response (
37). These multiple functions are managed by the balance of tonic and phasic firing of locus coeruleus neurons in concert with reciprocal cortical connections. Accumulated evidence over the past 25 years also demonstrates that guanfacine stimulates alpha
2A receptors in the prefrontal cortex, with potential benefits in working memory, attention, and impulse control (
38). In the present study, we did not detect differences between guanfacine and placebo on tests of working memory or motor planning. It appears that guanfacine did not enhance or hinder cognitive functioning in this sample. Both mechanisms (reduced tonic firing of locus coeruleus neurons and stimulation of prefrontal alpha
2A receptors) may have contributed to the clinical results of this study.
Although symptoms of ADHD and ASD often co-occur and may reflect shared underlying genetic risk (
39,
40), the ADHD syndrome in ASD may differ from ADHD in children without ASD. Children with ASD may be internally focused on topics of special interest, find little reward in matters outside of their circumscribed interest, and, consequently, pay little attention to other environmental stimuli. Hyperactivity and impulsiveness in children with ASD appear similar to the hyperactivity and impulsiveness in ADHD and are more amenable to measurement.
The significant improvement in ADHD symptoms in the guanfacine-treated group compared with placebo notwithstanding, the trial has several limitations. This study provides only acute efficacy and safety results. Furthermore, wide variability in school settings and enrollment during summer months precluded collection of teacher ratings. Finally, the sample size limits the ability to identify clinical characteristics that moderate treatment response.
Acknowledgments
The authors thank Yale Allison Gavaletz, B.A., and Caitlin Tillberg, B.A., for study coordination; Laura Simone for data management; Lily Katsovich, M.S., M.B.A, Gerald Golden, M.D, Christopher Young, M.D., and William Mahle, M.D., for serving on the data and safety monitoring board; and Nichole Evans for assistance with manuscript preparation.