The onset of severe psychiatric illness immediately after childbirth has been described extensively. In the 19th century, case reports described women with severe mania or psychosis after every delivery, including some with as many as 13 pregnancies (
1). Interestingly, these women had isolated episodes of postpartum psychosis or mania without psychiatric episodes outside the postpartum period. Later studies confirmed the vulnerability to psychosis and mania specifically in the postpartum period, including a high postpartum relapse risk after subsequent pregnancies (
2,
3). Accordingly, a history of isolated postpartum psychosis is widely considered a strong risk factor for future severe postpartum episodes.
A second group at high risk for relapse in the postpartum period comprises women with a previous diagnosis of bipolar disorder. Patients with bipolar disorder are more likely to experience a puerperal psychiatric admission compared with patients with any other psychiatric diagnosis. Kendell et al. (
4) were the first to quantify this risk in a population-based cohort. They described a relapse risk of 16% for puerperal admission in patients with bipolar disorder, compared with 3% for patients with schizophrenia and 2% for patients with depression. More recently, Munk-Olsen et al. (
5) replicated this finding in a birth register study by comparing the relative risk for puerperal admissions during the first month postpartum with admissions 11–12 months postpartum. They found a higher relative risk for relapse during the early postpartum period for patients with bipolar disorder (relative risk=37.2, 95% CI=13.6, 102.0) compared with patients with schizophrenia (relative risk=4.6, 95% CI=2.5, 8.5) or other psychiatric disorders (relative risk=3.0, 95% CI=1.9, 4.7).
Women diagnosed with bipolar disorder are at high risk for postpartum episodes, including psychosis and mania. Moreover, first-onset psychosis or mania occurring in the postpartum period is sometimes found in retrospect to be the incipient episode of a lifelong diagnosis of bipolar disorder (
6,
7). Importantly, however, retrospective long-term follow-up studies have shown that a substantial proportion of women with first-onset postpartum psychosis or mania do not have a bipolar illness course with manic and depressive episodes outside the postpartum period (
6). Instead, these women have isolated postpartum psychosis: their risk of mania and psychosis appears to be limited to the postpartum period. Accordingly, increasing evidence suggests that isolated postpartum psychosis may represent a unique diagnostic entity, distinct from bipolar disorder (
8). Previous studies have demonstrated important differences between isolated postpartum psychosis and bipolar disorder, in both acute treatment and medication prophylaxis (
3,
8,
9). From a neurobiological perspective, it is likely that women with isolated postpartum psychosis have a selective vulnerability to the endocrine and immunological changes that follow childbirth, in contrast to women with bipolar disorder, for whom neurobiological triggers are also present outside the postpartum period (
10,
11).
Estimation of relapse risks for women with isolated postpartum psychosis or bipolar disorder have been described in prospective, retrospective, and birth cohort studies. However, the high variability of reported relapse rates across different studies has hampered efforts to obtain a precise quantification. For example, a Swedish birth register study described a postpartum relapse rate of 8.5% in patients with bipolar disorder, whereas an Italian retrospective cohort study found a prevalence rate of 75% in medication-free patients with bipolar disorder (
12,
13). Similar difficulties in the interpretation of studies have arisen for patients with a history of postpartum episodes. For example, a 2012 prospective cohort study from the Netherlands reported a relapse rate of 14% in women with isolated postpartum psychosis, whereas a 2013 retrospective cohort study from the United Kingdom reported a relapse rate of 58% in patients with a history of postpartum psychosis (
2,
3).
A weighted estimation of relapse risk is essential for clinicians and patients to perform a risk-benefit analysis and should ideally include an estimate of the duration of the high-risk period. On the basis of these evidence-based prognoses, patients can be empowered to develop an individualized peripartum plan with their clinicians, covering the period from conception to 1 year postpartum. Before conception, the magnitude of the estimated relapse risk often directly influences family planning. Previous studies have shown that women with first-onset postpartum mania or psychosis are less likely to have additional children. Moreover, women with bipolar disorder are known to have lower fecundity rates compared with the general population (
14). The estimated risk of relapse is particularly relevant during pregnancy, in balancing the benefits of prophylactic medication with the risks of fetal medication exposure. In the postpartum period, decisions regarding pharmacotherapy and breastfeeding are strongly influenced by the estimated risk of relapse.
Clearly, the accuracy and reliability of the weighted estimation of relapse risk is a major determining factor underlying the benefit of this approach. Unfortunately, however, researchers and clinicians have limited knowledge about the relapse risk. An overestimation of relapse risk might lead to overly distressed future parents, excessive medication use, reduced rates of breastfeeding, or unnecessarily altered family planning. Underestimation of relapse risk might lead to ineffective relapse prevention strategies and delay referral for specialized perinatal care in which optimal coordination between obstetric and mental health care providers could otherwise be arranged (
3). With even more severe consequences, underestimation of relapse risk would undoubtedly result in higher rates of quality of life impairment, acute inpatient hospitalization, and suicide (
15).
In this study, we performed a systematic review and meta-analysis to examine the risk of postpartum relapse in women with a history of bipolar disorder, postpartum psychosis or mania, or both diagnoses. We compared the severity of episodes and the duration of postpartum follow-up and examined the association between relapse and prophylactic medication. We also identified methodological factors that account for heterogeneity across studies.
Method
Literature Search
The initial systematic literature search was performed on Aug. 26, 2013, in all large electronic medical databases, using the search terms “bipolar,” “postpartum,” “psychosis,” and “relapse” and “risk.” The search was updated on Jan. 6 and Nov. 11, 2014 (see the data supplement that accompanies the online edition of this article).
Selection of Studies
The selection procedure was conducted according to the PRISMA and MOOSE guidelines (
16,
17). Studies were eligible for inclusion if they were written in English and if patients were diagnosed with bipolar disorder and/or a history of a psychotic or manic episode following childbirth according to DSM criteria, ICD criteria, or the Research Diagnostic Criteria (RDC) (
18). Information about psychiatric relapse within 12 months postpartum was obtained (proportion of patients and/or deliveries). We defined relapse as psychosis, mania or hypomania, depression (or a mixed episode), and/or psychiatric hospitalization. All longitudinal study designs (cohort studies, randomized controlled trials, and birth register studies) were suitable for inclusion.
Data Extraction
Data were extracted by two independent observers (R.W. and A.M.K.) using a data extraction form. Observers were not blind to authors, institutions, or journals. In case of difference in assessment between the two observers, a decision was made with help from a third independent observer (V.B.). Relapse rates were extracted both for patients with a history of bipolar disorder and for those with a history of postpartum psychosis. Studies reporting incidence or prevalence rates were considered eligible for inclusion. As the numerator, relapse events, including psychosis, mania or hypomania, depression (or a mixed episode), and/or psychiatric hospitalization were counted. An event was defined as a severe relapse when an affective psychosis, mania, mixed episode, or relapse required hospitalization. As the denominator, we used the total number of deliveries (study outcome incidence rate) or patients (study outcome prevalence rate). For studies that included more than one delivery per patient, deliveries were considered independent events. In longitudinal studies of patients with a history of postpartum psychosis, only participants with subsequent deliveries were included. Studies that examined various diagnostic entities (e.g., bipolar disorder and schizophrenia) were included only if relapse outcomes were described for each diagnostic category. We screened all included studies for postpartum relapse rates with regard to prophylactic pharmacotherapy. We compared postpartum relapse rates between women with and without prophylactic medication use during pregnancy, the postpartum period, or both.
If a study reported relapse rates at more than one time point during the postpartum period, the data were pooled to calculate an overall relapse rate. All included studies were part of the qualitative synthesis. In those sets of articles for which overlapping cohorts were used, only the most complete or most recent data set was included in the meta-analysis (quantitative synthesis).
Quality Assessment
The reviewers independently assessed the quality of the included studies, according to the GRADE guidelines (
19). Potential bias was assessed with regard to the following quality criteria (
20): definition of inclusion (DSM, ICD, RDC), definition of relapse (DSM/RDC/ICD, hospitalization, clinical interview, or unknown), handling of missing data, and year of publication.
Procedure for Meta-Analyses
We used random-effects estimation and a 95% confidence interval to calculate an overall relapse rate. This provided the opportunity to compare relapse rates between patients with bipolar disorder and those with a history of postpartum psychosis and to assess the influence of pharmacotherapy on relapse. Random-effects analysis was used because it produces a more reliable estimate of the overall relapse rate than fixed-effects analysis in case of substantial heterogeneity (
21). Univariate analyses were performed to assess the association of independent variables with the overall relapse rate. The association with categorical characteristics was assessed using random-effects estimation to calculate and compare the overall outcome per category. Q statistics and significance levels are reported. The association of continuous characteristics with outcome was assessed by performing mixed-effects meta-regression analyses using unrestricted maximum-likelihood estimation, with log relapse rate as the response variable. We added 0.0001 in case of zero cell observations. Beta values with 95% confidence intervals and significance levels are reported. Statistical analyses were performed using the Comprehensive Meta-Analysis program, version 2.2.034 (
22).
Publication Bias
Publication bias was visually assessed with a funnel plot and formally with the Egger test, to assess whether the relapse rate decreased with increasing sample size. Plots with a funnel shape are considered to occur only when publication bias is low or absent. Since nonsignificant studies are less likely to be published, studies in the bottom left-hand corner of the plot are often omitted (
23).
Heterogeneity and Sensitivity Analyses
Cochran’s Q test and I2 statistics were used to quantify heterogeneity across studies. Heterogeneity was further explored by conducting sensitivity analyses. For this aim, we calculated the overall relapse rate using both fixed- and random-effects modeling and evaluated the impact of the modeling procedure on the overall relapse rate of all studies. We compared relapse rates based on the study quality criteria described in the Quality Assessment section above. In addition, we compared retrospective cohort, prospective cohort, and birth register studies; incidence rates and prevalence rates; one delivery per patient versus multiple deliveries per patient; qualitative versus quantitative synthesis; and duration of follow-up. For the analyses regarding the duration of follow-up, we categorized studies by the following thresholds: relapse within <4 weeks, <3 months, <6 months, and <12 months postpartum. Finally, we assessed the influence of the duration of follow-up as a continuous variable on relapse rate.
Results
Selection of Studies
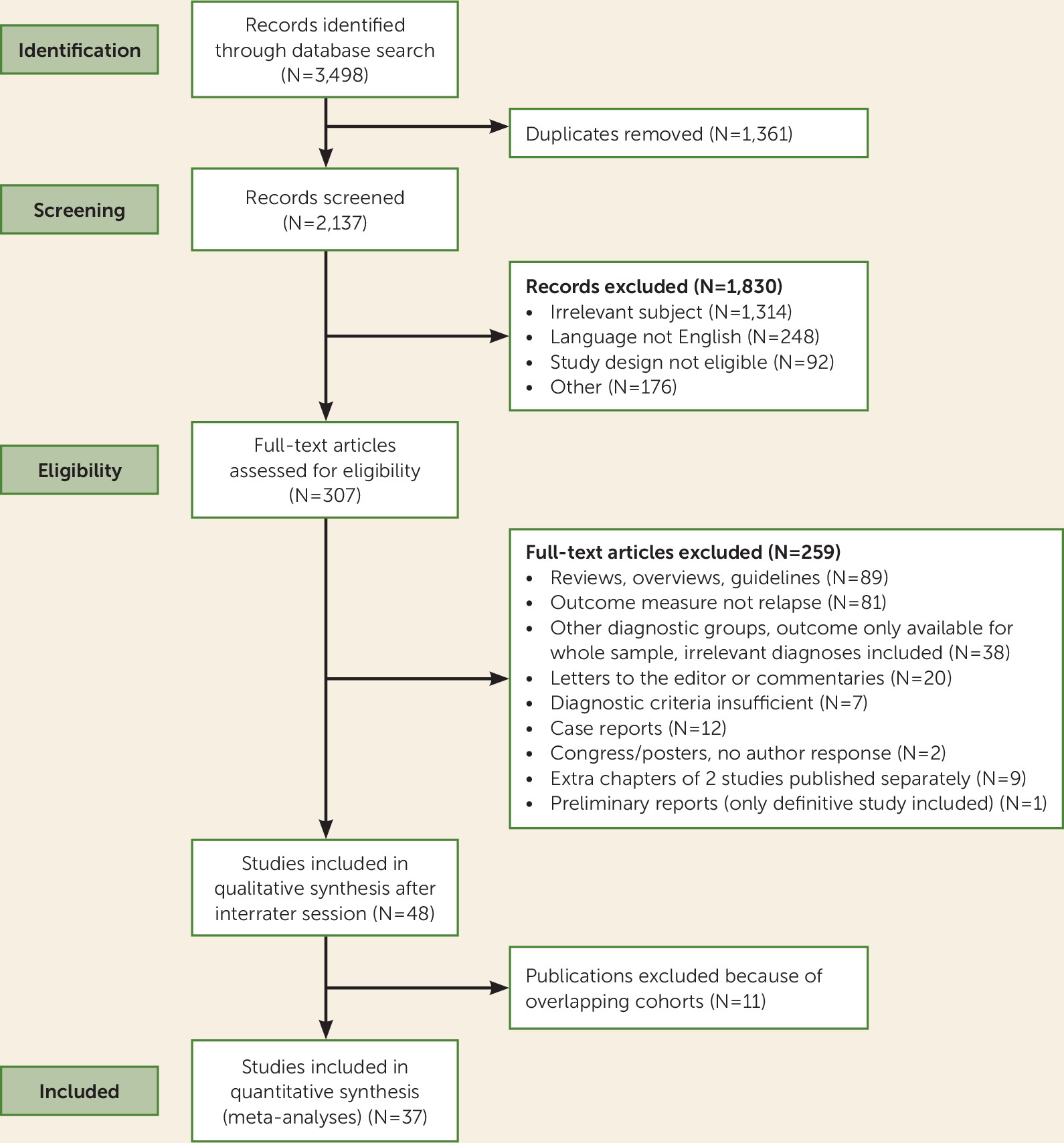
The literature search produced a set of 3,498 articles. After de-duplication, the set was narrowed to 2,137 articles, which were then reviewed in an interrater session (R.W. and A.M.K.) based on title and abstract, resulting in an initial selection of 307 articles. After full-text assessment of the 307 articles, 48 were included in the qualitative synthesis. Screening for overlap in the investigated cohorts resulted in the exclusion of 11 studies. Therefore, 37 articles were included in the quantitative synthesis; publication dates were between March 1986 and October 2014 (articles published before March 1986 did not use DSM, ICD, or RDC criteria and were therefore not considered) (
Figures 1 and
2). Interrater reliability was high (raw interrater agreement=94.7%, kappa=0.88, 95% CI=0.80, 0.96).
Study Characteristics
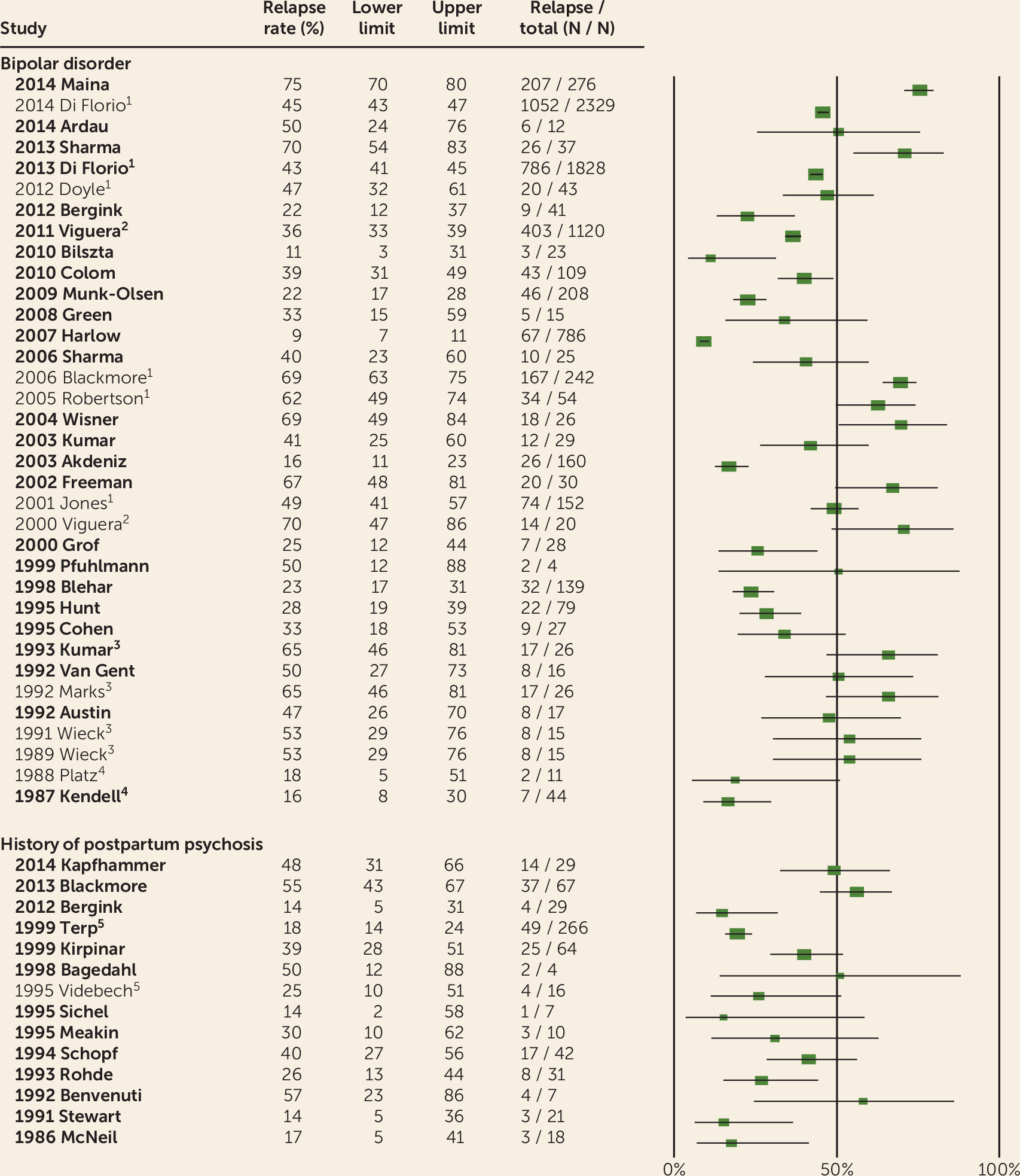
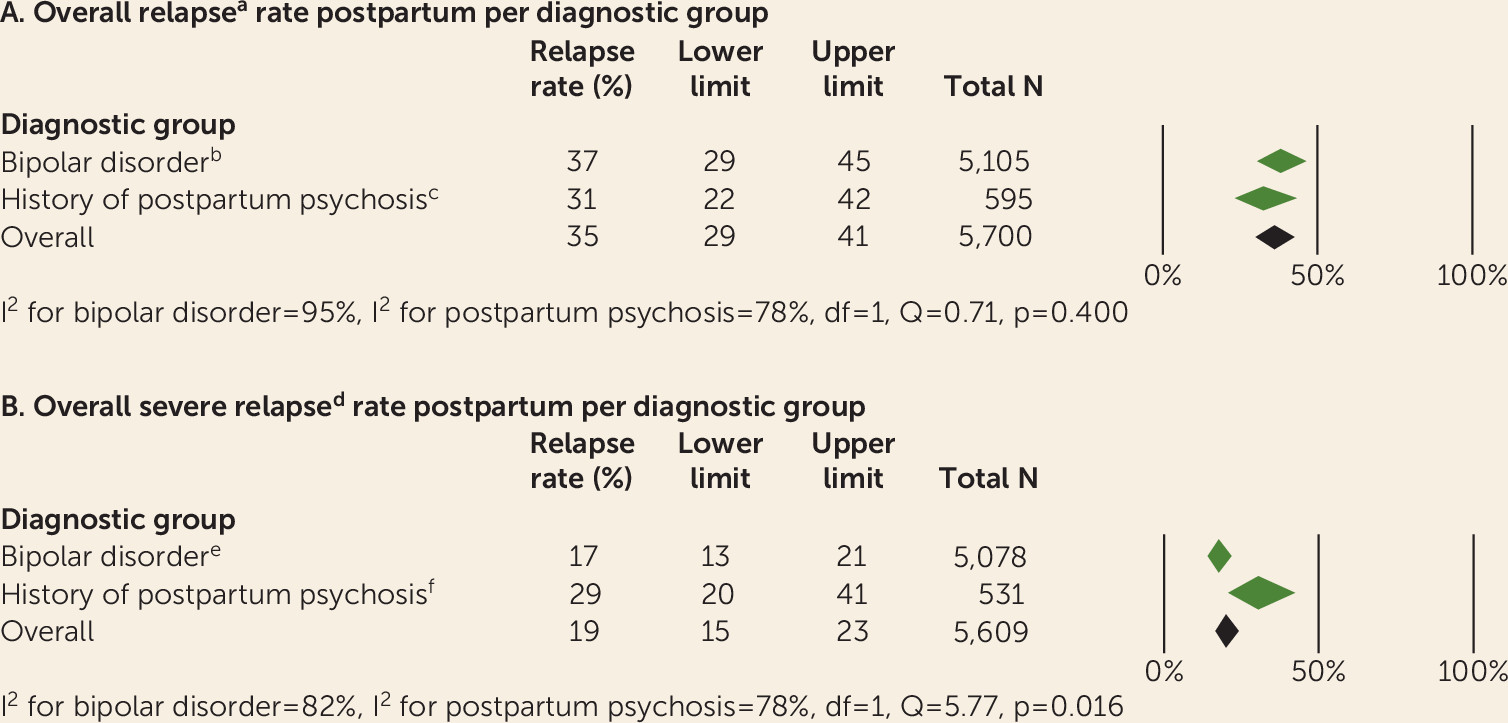
In the quantitative selection (N=37 studies), the outcome of 5,700 deliveries in 4,023 patients was provided. We found an overall postpartum relapse risk of 35% (95% CI=29, 41). Twenty-four studies focused on patients with bipolar disorder, 12 studies focused on patients with a history of postpartum psychosis, and one study described independent groups of patients with bipolar disorder and a history of postpartum psychosis (
Figures 2 and
3A). The largest study described the outcome of 1,828 deliveries in the United Kingdom (
24). Other large studies were conducted at centers in the United States (1,120 deliveries) (
25), Sweden (786 deliveries) (
12), Italy (276 women) (
13), and Denmark (208 deliveries) (
5). Detailed characteristics of all studies are provided in Table S1 in the online
data supplement.
Postpartum Relapse Rates in Patients With Bipolar Disorder
As shown in
Figure 3A, patients with bipolar disorder had an overall relapse risk of 37% (95% CI=29, 45) (25 studies, 5,105 deliveries, 3,495 patients). Three large studies and one small study made a distinction between patients with bipolar I and II disorders (
13,
25–
27). Two studies included only patients with bipolar I disorder (
28,
29) and one study enrolled only patients with bipolar II disorder (
30). No significant difference in relapse rates was found between patients with bipolar I and II disorders (bipolar I disorder: N=2,190, 45% [95% CI=32, 58]; bipolar II disorder: N=1,249, 50% [95% CI=35, 65]; Q=0.25, df=1, p=0.62).
Postpartum Relapse Rates in Patients With a History of Postpartum Psychosis or Mania
Patients with a history of postpartum psychosis had an overall relapse risk of 31% (95% CI=22, 42) (13 studies, 595 deliveries, 528 patients) (
Figure 3A). Eleven of the 13 studies included only patients with first-onset psychosis, and the other two studies provided no information regarding psychiatric history prior to the onset of their postpartum psychosis. Of the 11 studies that included only patients with first-onset postpartum psychosis, the longitudinal illness course was reported in seven studies.
In three of these seven longitudinal follow-up studies, patients with isolated postpartum psychosis were described (54 deliveries, 54 patients) (
3,
31,
32). The remaining four studies (144 deliveries, 144 patients) reported that a proportion of patients had nonpuerperal episodes during follow-up. There was no significant difference in postpartum relapse rate between patients with bipolar disorder and patients with a history of postpartum psychosis (Q=0.71, df=1, p=0.40). Heterogeneity was substantial in both diagnostic groups.
Postpartum Relapse Rates in Patients With Bipolar Disorder and Previous Postpartum Episodes
Nine studies provided information on the prior history of postpartum episodes (9/25, 36%). Two birth register studies included only primiparous patients, who by definition did not have a history of postpartum episodes (
5,
11). Three studies provided detailed information on patients with bipolar disorder and a prior history of postpartum episodes. The relapse rate was 87% in one study (45/52 patients) (
13) and 50% in each of the other two studies (2/4 patients [
33], 4/8 patients [
3]). In the remaining four studies, 41%−73% of patients with bipolar disorder had a history of postpartum episodes (
34–
37). Altogether, there is currently insufficient available information on relapse risk for women with bipolar disorder to permit stratification by their history of previous postpartum episodes.
In a subanalysis, the risk of a severe postpartum episode (affective psychosis, mania, mixed episode, or relapse requiring hospitalization) was significantly higher in patients with a history of postpartum psychosis (29%, 95% CI=20, 41) compared with patients with bipolar disorder (17%, 95% CI=13, 21; Q=5.77, df=1, p=0.016) (
Figure 3B). Two studies were excluded because of insufficient information regarding the clinical severity of the postpartum episodes (
34,
38).
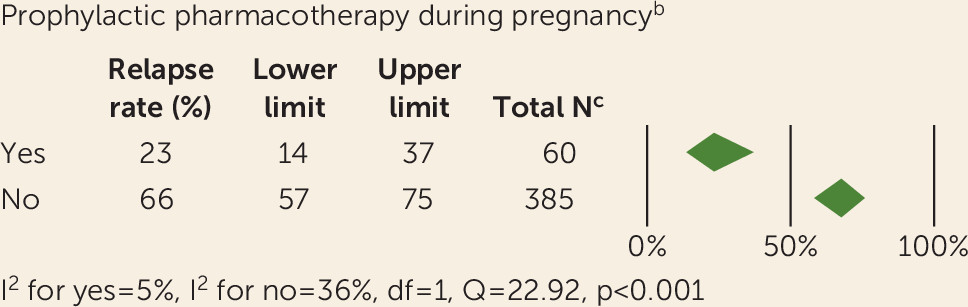
Prophylactic Pharmacotherapy During the Peripartum Period in Bipolar Disorder
In the quantitative synthesis, a total of five studies provided sufficient information to assess the association between postpartum relapse and prophylactic pharmacotherapy during both pregnancy and the postpartum period (
3,
36,
37,
39,
40). In addition, three studies provided information on pharmacotherapy during pregnancy (
13,
27,
41), and three studies described pharmacotherapy during the postpartum period (
34,
35,
42). Overall, patients with bipolar disorder using prophylactic pharmacotherapy during pregnancy had a significantly lower relapse rate (N=60; 23%, 95% CI=14, 37) compared with medication-free patients (N=385; 66%, 95% CI=57, 75; Q=22.92, p<0.001) (
Figure 4). Moreover, patients with bipolar disorder using prophylactic pharmacotherapy during the postpartum period had a lower relapse rate (N=98; 29%, 95% CI=16, 47) compared with those who remained medication free (N=107; 65%, 95% CI=55, 73; Q=10.91, p=0.001). Of all 98 women reported as having used medication postpartum, 38 women initiated prophylactic medication during pregnancy (
3,
37). Twenty-two patients were medication free during pregnancy and initiated prophylaxis immediately postpartum (
3,
36,
37) (see Table S1 in the online
data supplement). Information regarding the timing of medication initiation was unavailable for 38 women.
Prophylactic Pharmacotherapy During the Peripartum Period in Patients With a History of Postpartum Psychosis
Five studies (5/13, 39%) provided information on pharmacotherapy during the peripartum period. During pregnancy, all patients in these five studies were medication free. Of these studies, three provided information on prophylactic medication use during the postpartum period. One study reported a relapse rate of 30% in 10 medication-free patients (3/10) (
43). The second study reported a relapse rate of 14% in 21 patients with lithium prophylaxis (3/21) (
44). In the third study, none of the patients using lithium prophylaxis relapsed (0/20), compared with a relapse rate of 44% (4/9) for medication-free patients (
3).
Publication Bias
There was no association between year of publication and relapse rates (β=0.02, 95% CI=−0.01, 0.05; Q=1.55, p=0.21). The studies reporting the lowest (9%) and highest (75%) relapse rates (
12,
13) were both published relatively recently (2007 and 2014, respectively). A visual inspection of the funnel plot revealed that the plot was asymmetric, with a slightly larger proportion of the medium-sized trials clustering to the left of the mean, but no indication of decreasing event rates with increasing sample size (see Figure S1 in the online
data supplement). The Egger test did not suggest the presence of publication bias (intercept=−0.57, 95% CI=−2.37, 1.24, p=0.53).
Heterogeneity and Sensitivity Analyses
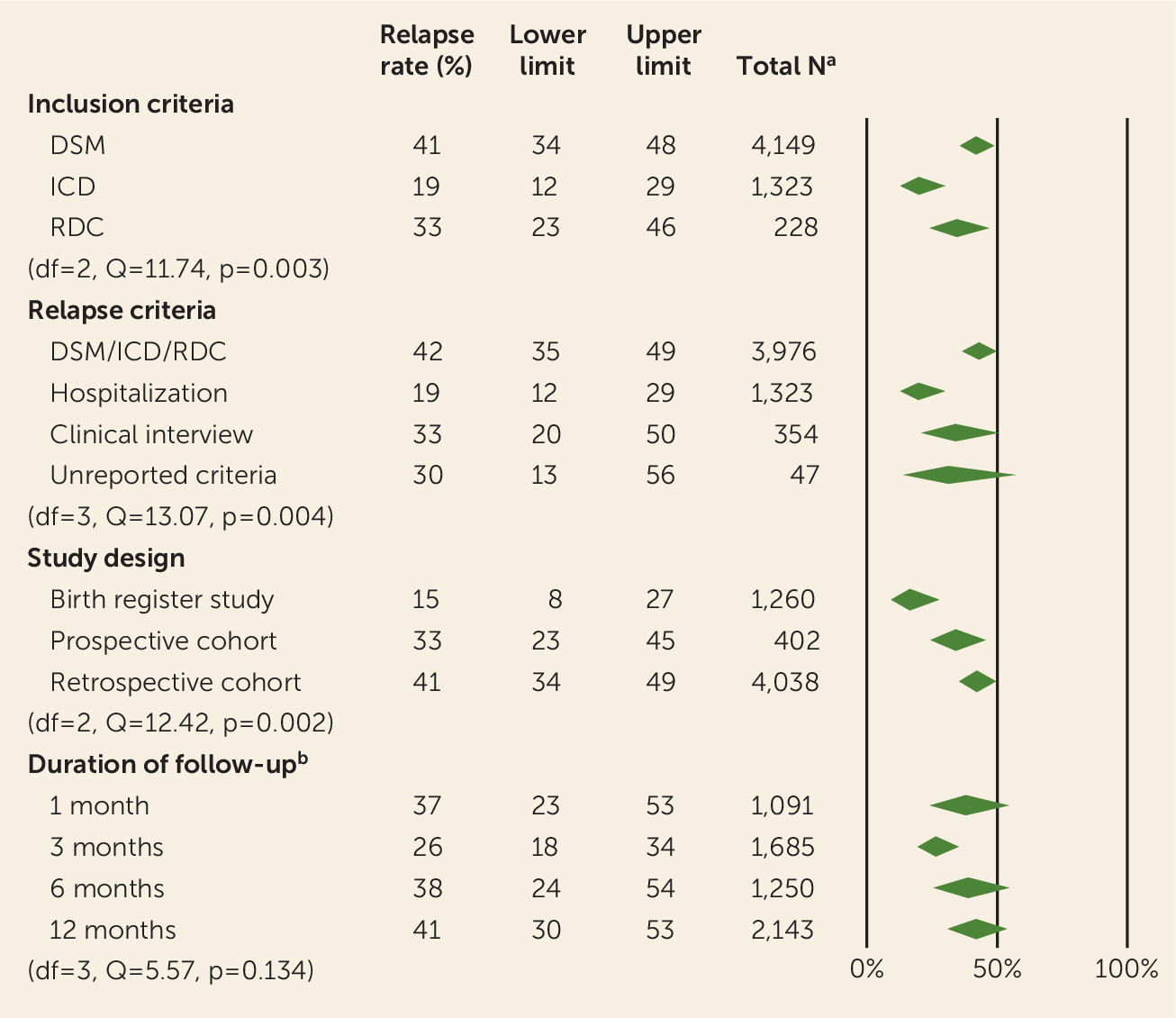
We compared both the inclusion criteria (DSM, ICD, or RDC) and the criteria for relapse (DSM/ICD/RDC, hospitalization, clinical interview, or unreported). Studies that included patients by DSM diagnoses showed higher relapse rates (41%, 95% CI=34, 48) compared with those using ICD diagnoses (19%, 95% CI=12, 29) or RDC criteria (33%, 95% CI=23, 46) (Q=11.74, df=2, p=0.003). Studies that defined their relapse criteria on the basis of DSM, ICD, or RDC criteria showed a higher overall relapse rate (42%, 95% CI=35, 49) compared with studies that used distinct criteria (hospitalization: 19%, 95% CI=12, 29; clinical interview: 33%, 95% CI=20, 50; unreported criteria: 30%, 95% CI=13, 56) (Q=13.07, df=3, p=0.004). No significant difference was found in overall relapse rates, depending on whether or not studies reported their procedures for handling missing data (respectively, 35%, 95% CI=27, 45, and 34%, 95% CI=25, 44; Q=0.05, df=1, p=0.82).
Birth register studies reported lower relapse rates (15%, 95% CI=8, 27) compared with prospective and retrospective cohort studies (33%, 95% CI=23, 45 and 41%, 95% CI=34, 49, respectively; Q=12.42, df=1, p=0.002), primarily because of relatively high relapse rates in the retrospective cohort studies. Twenty-eight studies reported incidence rates (3,297 patients), and the remaining nine studies reported prevalence rates (726 patients). No significant difference was found between studies that reported incidence rates (32%, 95% CI=26, 40) and those that reported prevalence rates (43%, 95% CI=28, 60; Q=1.32, df=1, p=0.25).
In 10 studies, there were more deliveries than patients. Together these studies described the outcome of 3,613 deliveries in 1,936 patients. There was no significant difference in relapse rates when comparing these 10 studies (33% 95% CI=26, 41) with the 27 studies that limited inclusion to one delivery per patient (35%, 95% CI=25, 47; Q=0.16, df=1, p=0.69).
No significant difference was found between the qualitative and quantitative synthesis (Q=0.82, df=1, p=0.37). The duration of postpartum follow-up ranged from 1 month to 12 months across studies (see Table S1 in the
data supplement). However, the majority (89%) of studies defined a threshold between 4 weeks and 6 months postpartum. Regression analysis revealed no significant association between relapse risk and duration of follow-up (β=0.02, 95% CI=−0.06, 0.09; Q=0.23, p=0.63). Furthermore, no difference was found between studies that used different thresholds for the duration of follow-up (Q=5.57, p=0.13). Results of the relevant sensitivity analyses are shown in
Figure 5.
Discussion
Our meta-analysis demonstrated that patients with either a history of affective psychosis in the postpartum period or bipolar disorder are at high risk for postpartum relapse. We included 37 articles describing the outcome of 5,700 deliveries in 4,023 patients and found an overall relapse risk of 35% (95% CI=29, 41).
Postpartum Relapse Rates in Patients With Bipolar Disorder
In women with bipolar disorder, we found an overall relapse risk of 37%. In 17% of the cases, patients suffered from affective psychosis, mania, mixed episodes, or relapses requiring hospitalization, defined as severe episodes. Accordingly, the remaining patients had nonpsychotic affective episodes (mostly depressive and a limited number of hypomanic episodes).
In our subanalysis, we were able to include seven studies, describing the outcome of 2,190 deliveries to patients with bipolar I disorder and 1,249 deliveries to patients with bipolar II disorder. Remarkably, we were unable to detect a differential relapse risk between patients with bipolar I and II disorders. A previous study (
24) found a higher relapse risk in patients with bipolar I disorder compared with patients with bipolar II disorder in the United Kingdom. However, as acknowledged by the authors, they observed few hypomanic episodes, possibly because of inherent difficulties in retrospectively documenting hypomanic episodes and therefore biasing the results toward a lower observed relapse risk in patients with bipolar II disorder.
Most studies did not provide information on previous postpartum episodes. The widespread clinical impression is that women with bipolar disorder and previous postpartum episodes might fall within the highest risk category. Unfortunately, we could not estimate the risks for this specific group. Moreover, since we were not able to stratify patients with bipolar disorder by a history of postpartum episodes, it is unclear whether bipolar disorder and a history of postpartum relapse contribute linearly or nonlinearly to the relapse risk for bipolar patients.
Postpartum Relapse Rates in Patients With a History of Postpartum Psychosis or Mania
Few studies have focused on patients with a history of psychosis in the postpartum period, likely because of both the low prevalence and uncertainties regarding its diagnostic status. We included 13 studies (595 deliveries, 528 patients), for which the overall relapse risk was 31%. Notably, only three studies included patients exclusively with isolated postpartum psychosis (54 deliveries, 54 patients). In the remaining 10 studies, a proportion of patients might have had bipolar episodes before the onset of postpartum psychosis (two studies) or after postpartum psychosis (eight studies), although this information was not reported.
The overall relapse rate of patients with a history of postpartum psychosis was not significantly different from the relapse risk observed in patients with bipolar disorder, but patients with a history of postpartum psychosis were more likely to have severe postpartum relapse episodes compared with patients with bipolar disorder. We observed that studies reported few nonsevere postpartum relapse episodes in patients with a history of postpartum psychosis, which could be due to selection and/or information bias. For example, studies in women with a history of postpartum psychosis might have been designed with an inclusion bias favoring patients with severe manic or psychotic relapse but not depression or hypomania. Accordingly, the 31% overall relapse rate we found could be an underestimation.
Prophylactic Pharmacotherapy Is Highly Effective for Relapse Prevention
Most studies of prophylactic pharmacotherapy for bipolar disorder and postpartum psychosis have focused on lithium. In contrast, data regarding the prophylactic efficacy of lamotrigine, olanzapine, quetiapine, and risperidone are scarce (see Table S1 in the
data supplement). In women with bipolar disorder, we were able to stratify postpartum relapse rates by pharmacotherapy during pregnancy in 445 women. Women without prophylactic pharmacotherapy during pregnancy had a postpartum relapse rate of 66%, compared with 23% for women with prophylaxis (
Figure 4). Medication prophylaxis during pregnancy in women with bipolar disorder appears important not only to maintain mood stability during pregnancy (
45) but also for postpartum relapse prevention. However, the benefits of prophylactic pharmacotherapy during pregnancy should be weighed against the potential adverse effects of in utero medication exposure.
Available data were insufficient to allow us to evaluate the efficacy of pharmacotherapy when it is initiated immediately after delivery as a prophylaxis strategy in women with bipolar disorder. Together, our findings suggest a protective effect of lithium throughout pregnancy and the postpartum period.
Two studies (60 patients) described the efficacy of prophylactic pharmacotherapy in women with a history of postpartum psychosis (
3,
44). Both studies reported that initiation of prophylactic lithium immediately postpartum after a medication-free pregnancy—and thus eliminating the risk of in utero medication exposure—is highly effective for relapse prevention.
Clinical Predictors of Relapse
Another possible predictor of relapse is parity. Previous studies showed that primiparity is a risk factor for relapse in the early postpartum period (
26,
46). Di Florio et al. (
26) found that this effect was not due to women with a history of postpartum episodes being less likely to have additional children. In addition, Munk-Olsen et al. (
46) found a higher risk for a first-time psychiatric episode after a second delivery with increasing time between the births of the first and second children. In the present meta-analysis, we were not able to stratify for parity. Therefore, the interpretation of an overall relapse risk requires some caution, especially when comparing patients with bipolar disorder who could be either primiparous or multiparous with patients with a history of postpartum psychosis, who are by definition not primiparous. Notably, as mentioned by Di Florio et al. (
26), it is possible that the association between primiparity and relapse is confounded by the higher proportion of multiparous patients using prophylactic pharmacotherapy.
Several additional predictors for postpartum relapse have been described previously, including relapse during pregnancy (
3,
47), psychiatric history (
13,
48), family history (
49), and obstetric complications (
50,
51). The assessment of the weight of each of these factors enables clinicians to establish individualized prevention plans for the high-risk postpartum period. Unfortunately, these variables have been understudied and therefore could not be included in this meta-analysis as effect modifiers or confounders.
Heterogeneity Across Studies
There was considerable heterogeneity across studies, both in their design and in their inclusion and relapse criteria. In contrast to population-based studies, selection bias may have occurred in both prospective and retrospective cohort studies. Our sensitivity analyses demonstrated that retrospective studies reported significantly higher relapse rates compared with birth register and prospective studies. Notably, an important source of selection bias in retrospective cohort studies is nonsystematic sample recruitment. For example, the largest study we examined involved the retrospective analysis of a U.K. cohort of patients with bipolar disorder from which 74% of the patients were recruited via sources such as public media and patient organizations (
24). As acknowledged by the authors, this may have led to an overestimation of relapse risk. In addition, retrospective studies have considerable potential for information bias because of long intervals between the relapse episode and data collection. Conversely, prospective studies are inherently biased toward underestimation of relapse risk because of selection bias, since patients with a poor prognosis are less likely to visit an outpatient clinic during pregnancy or to participate in a clinical study.
Birth register studies are more likely to provide estimates of relapse rates that are free of selection and information bias. Moreover, they have superior external validity because they are based on nationwide registers. However, a limitation of birth register studies is the precision of the available diagnostic information, in particular, the likely absence of data regarding less severe episodes that do not require contact with mental health care specialists, since available information is only based on women who actively sought care. Given that relapse was defined in all birth register studies using the criteria of an inpatient psychiatric admission, it is not surprising that the relapse rates were lower in birth register studies compared with cohort studies.
The majority of patients were included based on DSM or ICD criteria. The substantial difference in relapse rates between patients diagnosed using DSM versus ICD criteria is most likely the result of underlying study designs rather than the criteria themselves. Almost all studies using ICD criteria were birth register studies (
5,
12), while DSM criteria were used in the largest cohort studies (
24,
25).
Among the studies included in this meta-analysis, the duration of postpartum follow-up was highly variable, ranging from 4 weeks to 1 year, with the majority of studies having a follow-up interval in the range of 3–6 months. We did not find a statistically significant contribution of follow-up duration to relapse rate, which is consistent with the uniquely high relapse risk in the early postpartum period. In particular, the highest risk period for patients with bipolar disorder and/or a history of postpartum psychosis occurs within the first 3 months postpartum (
5,
24).
Research Implications
Over the past three decades, postpartum relapse rates in women with a history of bipolar disorder or postpartum psychosis have remained consistently high. Ongoing efforts to elucidate the risk and protective factors for these severe postpartum episodes hold considerable potential for substantially lowering the risk of postpartum relapse. Based on our data, we were not able to quantify the risk of relapse for women with both bipolar disorder and a history of postpartum episodes. Whether these risk factors combine linearly or interact nonlinearly remains to be determined. Future studies should be designed to quantify the relapse risk for potentially distinct subgroups of women with a history of isolated postpartum psychosis or mania, bipolar disorder, and both bipolar disorder and (severe) postpartum episodes. This classification should be based on information on parity and all previous postpartum and nonpostpartum episodes. Notably, birth register studies might be of substantial importance in obtaining these outcomes, given their population-wide and naturalistic implementation without selection or information bias.
In addition, there is an urgent need for more detailed data on the efficacy of prophylactic pharmacotherapy, including type, dosing, timing, and duration of medication use. Randomized controlled trials are likely to be very difficult to implement. Therefore, large-scale naturalistic prospective cohort studies may be the most practical approach to obtaining these data. Ideally, both maternal and neonatal outcomes should be included, given that postpartum psychiatric episodes are likely to influence the long-term outcome not only of the mother but also of her children.
Clinical Implications
In no other situation in psychiatry is it possible to define the moment of illness onset as precisely as in postpartum relapse, which offers the unique possibility of an individualized postpartum relapse prevention plan drafted in collaboration between women and their health care providers. Minimally, relapse prevention planning should include 1) medication prophylaxis during pregnancy and after delivery; 2) an obstetric birth plan, including preference regarding the mode of delivery; 3) progressive intervention strategies beginning from the earliest possible signs of prodromal symptoms for relapse; 4) neonatal medical evaluation for children with in utero medication exposure; 5) preference for baby feeding; and 6) strategies to assist women in obtaining adequate sleep, maintain a stable circadian rhythm, limit their stress, support maternal-newborn bonding, and enjoy their newborn experience.
Conclusions
In this meta-analysis, we found an overall postpartum relapse risk of 37% in women with bipolar disorder and 31% in women with a history of postpartum psychosis. The distinction between women with bipolar disorder and those with a history of postpartum psychosis is of substantial clinical relevance, as patients with bipolar disorder were significantly less likely to experience severe episodes postpartum (17%) compared with patients with a history of postpartum psychosis (29%). Moreover, for women with bipolar disorder, continuation of prophylactic medication during pregnancy appears to be critically important for maintaining mood stability after delivery. In contrast, for women with a history of isolated postpartum psychosis, the initiation of prophylaxis immediately after delivery appears to be highly effective for relapse prevention and eliminates the risk of in utero medication exposure. Women have multiple contacts with health services during pregnancy, which provide a compelling opportunity for prevention of postpartum psychiatric episodes. Postpartum relapse prevention plans should be drafted for all women at high risk.