Interpersonal psychotherapy (IPT) is a structured, time-limited psychological intervention that was developed for the treatment of major depression in the 1970s (
1,
2). Since then, numerous randomized controlled trials have shown that IPT is indeed effective in the treatment of depression (
3), that it may be more effective than other psychotherapies for depression (
4,
5), that it may prevent relapse after successful treatment of depression (
3), that it may prevent the onset of major depressive disorders in those with subthreshold depression (
6), and that it is also effective in specific target groups, such as adolescents (
7,
8), older adults (
9), and patients with a somatic disorder (
10–
12).
IPT focuses on stressful life events of grief, interpersonal disputes, life transitions, or social isolation or deficits that are associated with the onset, exacerbation, or perpetuation of current symptoms, while helping patients to connect with social supports and to improve the quality of their relationships (
13,
14). The beginning phase tasks include the forming of a therapeutic alliance, conducting a psychiatric assessment with an extended social history and interpersonal inventory, providing psychoeducation, instilling hope, and choosing an interpersonal focus. During the middle phase, interpersonal problem-specific therapeutic guidelines are applied. In the concluding phase, gains are consolidated, and adaptive interpersonal strategies and contingency plans in the event of relapse are reviewed.
Few systematic reviews examined the effects of IPT. Some focused on the effects of IPT for depression (
3,
24–
26), but none of these included trials published after 2010 (while 22 new trials have been subsequently published since [see below]); some focused on a small subsample of studies (
24,
25) or on narrow research topics, such as the comparison between IPT and care-as-usual (
24) or direct comparisons between IPT and cognitive-behavioral therapy (CBT) (
25). No meta-analysis has focused on IPT for disorders other than depression.
We conducted a comprehensive systematic review and meta-analysis of all randomized trials examining the effects of IPT for any mental health disorder.
Results
Selection and Inclusion of Studies
Of the 871 examined abstracts (647 after removal of duplicate records from multiple databases), 285 full-text articles were retrieved for further consideration. Of these, 195 were excluded (see the flowchart in Appendix A of the data supplement accompanying the online version of this article). Ninety studies met inclusion criteria (see Appendix B in the online data supplement).
Characteristics of Included Studies
The 90 studies included a total of 11,434 participants (4,422 in the IPT conditions, 2,906 in the control conditions, 1,823 in the comparisons with other psychotherapies, 1,464 in the comparisons with pharmacotherapy, and 819 in the comparisons with combined treatment of IPT plus pharmacotherapy). Selected characteristics of the studies are presented in Appendix C in the online data supplement. The majority of trials (69%) were targeted at depression; eight were aimed at eating disorders, another eight at anxiety disorders, and 12 at other mental health problems.
The risk of bias of the included studies varied. Forty-five of the 90 studies reported adequate sequence generation; 27 reported allocation to conditions by an independent (third) party; 58 studies reported blinding of outcome assessors; and in 60 studies intention-to-treat analyses were conducted. Sixteen studies met all four quality criteria, 41 met two or three criteria, and the remaining 33 studies had a lower quality.
Effects of IPT Compared With Control Groups as Acute-Phase Treatment of Depression
The majority of trials (N=62; 69%) were aimed at depression, including its acute treatment (N=50), maintenance treatment (N=6), and prevention (N=6). One trial compared online unguided IPT with two types of CBT (
37) but found no significant difference between the three (with all effect sizes g<0.10).
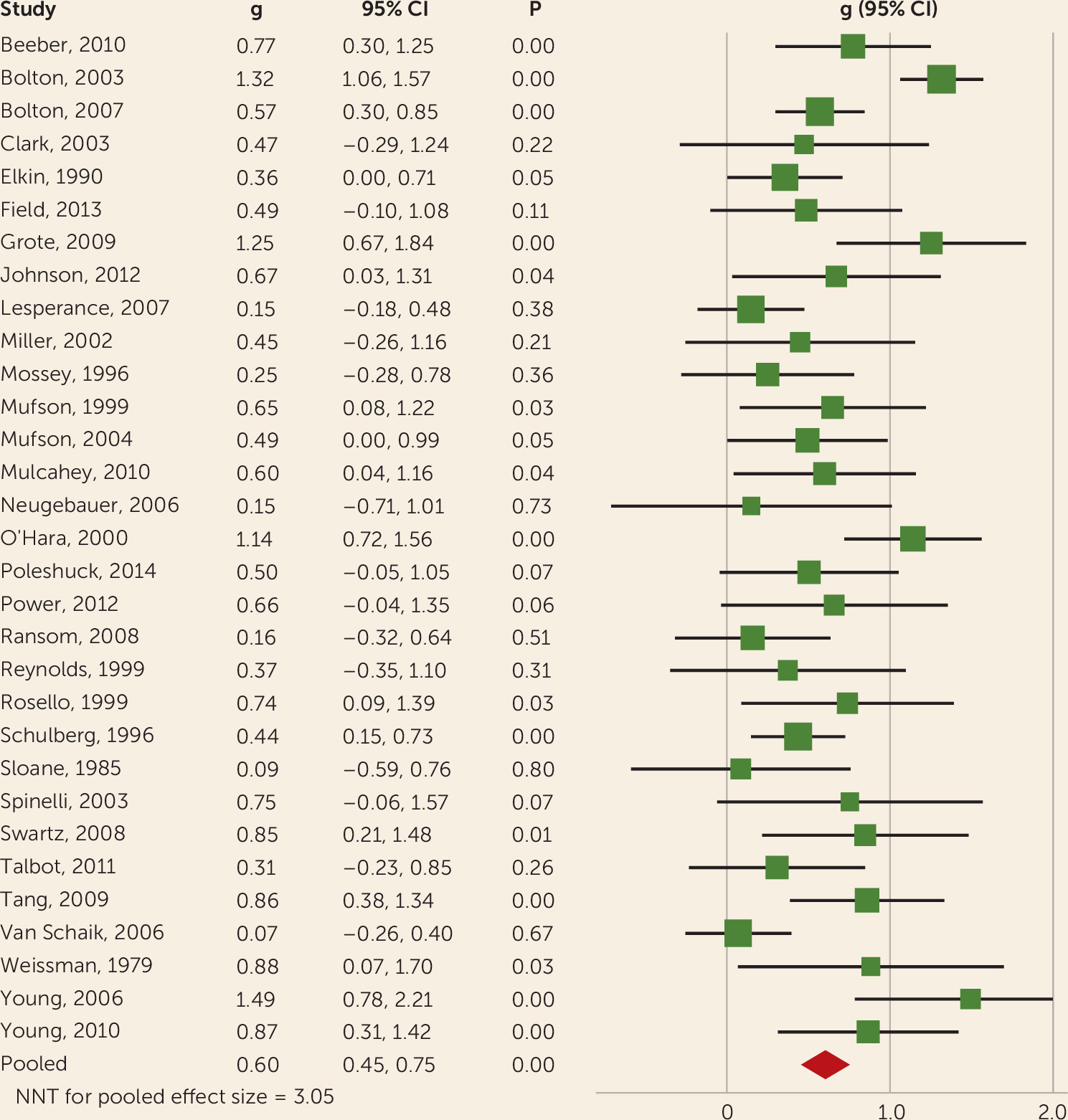
IPT was compared with a control condition in 31 studies (see
Figure 1 and
Table 1, as well as detailed outcomes in Appendix D in the
online data supplement). The effect size indicating the difference between IPT and control conditions at posttest was g=0.60 (95% confidence interval [CI]=0.45–0.75; number needed to treat=3), with moderate-to-high heterogeneity (I
2=63; 95% CI=52–69). The included studies had sufficient power to identify an effect size of g=0.16. We found no indications for publication bias.
A series of subgroup analyses (see Appendix D in the data supplement) indicated that type of recruitment was associated with the effect size (community and clinical recruitment had smaller effect sizes than other recruitment methods, such as screening in medical settings), and studies in which patients were diagnosed with a mood disorder had a smaller effect size than studies with patients scoring above a cut-off point on a self-report scale. Studies in older adults had a nonsignificant effect size that was smaller than in younger adults and adolescents, although the difference between age groups was not significant (p=0.05). Because the number of studies reporting outcomes at follow-up was small and the follow-up periods differed, we did not examine outcomes at follow-up.
Metaregression analyses showed no significant associations between the effect size and risk of bias of the studies. We did find a significant association with the number of sessions (slope=0.02; 95% CI=0.00–0.04; p=0.04).
IPT Versus Other Psychotherapies for Acute-Phase Depression
IPT for acute-phase depression was compared with other psychotherapies in 14 comparisons (see
Table 1, as well as Appendix D in the
data supplement). The difference between IPT and other psychotherapies at posttest was nonsignificant (g=0.06; 95% CI=–0.14 to 0.26; number needed to treat=29), with moderate heterogeneity (I
2=52; 95% CI=0–72). These studies had sufficient power to find an effect size of g=0.25.
The effect size according to the Hamilton Depression Rating Scale (HAM-D) was g=0.12 (0.46 points on the HAM-D; 95% CI=–1.43 to 0.83). There were some indications for publication bias, with results that nearly reached statistical significance (p=0.05) on the Egger’s test and two missing studies in the Duval and Tweedie procedure (adjusted effect size g=–0.00; 95% CI=–0.20 to 0.19). We conducted a limited number of subgroup analyses (because of the small number of comparisons) but found no significant differences between subgroups.
IPT and Antidepressant Medication for Acute-Phase Depression
IPT for acute depression could be directly compared with antidepressant medication in 16 trials (see
Table 1, as well as Appendix E in the
data supplement). The difference between IPT and antidepressant medication at posttest was nonsignificant (g=–0.13; 95% CI=–0.28 to 0.02; number needed to treat=14) in favor of antidepressant medication, with moderate heterogeneity (I
2=51; 95% CI=0–71). These trials had enough power to find an effect size of g=0.18.
Using only the HAM-D as outcome, the effect size was g=–0.24 (number needed to treat=7), corresponding with 1.70 points on the HAM-D (95% CI=0.21–3.19). We found no significant differences between subgroups (Appendix E in online data supplement) and no indication for publication bias.
The combination of IPT and antidepressant medication was compared with antidepressant medication alone in 10 studies (
Table 1) and resulted in a nonsignificant effect (g=0.14; 95% CI=–0.04 to 0.33; number needed to treat=13), with low heterogeneity (I
2=28; 95% CI=0–65). These studies had enough power to find an effect size of g=0.26. Studies with low risk of bias had a significant larger effect size than studies with high risk of bias (p=0.01), and the studies with low risk of bias differed significantly from zero (g=0.48; 95% CI=0.17–0.79; I
2=0; 95% CI=0–64). We found indications for publication bias (Egger’s test: p=0.01; number of imputed studies in the Duval and Tweedie procedure: 4; adjusted effect size: g=0.03; 95% CI=–0.18 to 0.24).
The combination of IPT and antidepressant medication was compared with IPT alone in seven studies (see Appendix E in the data supplement) and resulted in a significant effect in favor of combined IPT and antidepressant medication (g=0.24; 95% CI=0.03–0.46; number needed to treat=7), with low heterogeneity (I2=28; 95% CI=0–69). These studies had enough power to find an effect size of g=0.30. No significant difference between studies with high and low risk of bias was found (see Appendix E in the data supplement). There were some indications of publication bias (Egger’s test was not significant (p>0.1), but the Duvall and Tweedie procedure resulted in two imputed studies; adjusted effect size: g=0.18; 95% CI=–0.06 to 0.41).
Preventing the Onset or Relapse of Depressive Disorders With IPT
Five studies examined the effects of IPT on the incidence of new cases of major depression in people with subthreshold depression but no major depressive disorder (
Table 2). The odds of developing major depression at all time points for IPT compared with the control groups was an odds ratio of 0.30 (95% CI=0.10–0.88), with low heterogeneity (I
2=30; 95% CI=0–74; number needed to treat=7). The follow-up periods ranged from 3 to 18 months. More specific outcomes for the different follow-up periods are summarized in
Table 2. There was no indication of publication bias in these studies (Egger’s test: p>0.1; there were no imputed studies according to the Duval and Tweedie procedure).
Seven studies examined the effects of maintenance IPT after recovery from depression with the aim of preventing relapse and recurrence. Several comparisons could be examined in these trials (
Table 2). The combination of maintenance IPT, once-monthly, plus daily pharmacotherapy was significantly more effective in preventing relapse than pharmacotherapy alone (odds ratio=0.34; 95% CI=0.14–0.84; I
2=61; 95% CI=0–82; number needed to treat=7) and more effective than once-monthly maintenance IPT alone (odds ratio=0.30; 95% CI=0.11–0.71; I
2=50; 95% CI=0–82; number needed to treat=4). After removal of one outlier, the resulting odds ratio was still significant (odds ratio=0.51; number needed to treat=7; I
2=0). No indication was found that once-monthly maintenance IPT (plus placebo) differed significantly from pharmacotherapy, but maintenance once-monthly IPT (plus placebo) was significantly more effective than placebo only (odds ratio=0.47; number needed to treat=6). Unfortunately, none of the seven studies had a low risk of bias.
One study examined the effects of universal prevention in a general population of adolescents at schools (
38). IPT resulted in a significant effect size of g=0.26 (95% CI=0.01–0.51) compared with care as usual and a nonsignificant difference between IPT and CBT (g=–0.18; 95% CI=–0.45 to 0.09).
The Effect of IPT on Eating Disorders
IPT for eating disorders was examined in eight studies (see
Table 1 and Appendix F in the
data supplement). IPT was compared with another type of psychotherapy in six studies with eight comparisons. The effect size of all outcomes showed no statistically significant difference (g=–0.15; 95% CI=–0.32 to 0.03; number needed to treat=12 in favor of the other psychotherapies), and heterogeneity was zero (I
2=0; 95% CI=0–56). These studies had sufficient power to find an effect size of g=0.32.
When we differentiated the outcomes into effects on weight and body mass index (BMI) on the one hand and behavioral outcomes on the other hand, we found no significant difference for weight and BMI, but we did find a significant difference in favor of the alternative therapies for behavioral outcomes (g=–0.22; 95% CI=–0.39 to –0.05; number needed to treat=8; I2=0; 95% CI=0–56). When we further limited the alternative therapies to only CBT (six comparisons), we also found a small but significant difference in favor of CBT (g=–0.20; number needed to treat=9). Unfortunately, only two of the eight studies had low risk of bias, and the effect size for these studies was not significant (g=–0.13; number needed to treat=14). There were not enough studies to conduct subgroup analyses. We found no indication for publication bias. Long-term differences between IPT and other therapies were examined in only three studies and were therefore not examined.
IPT for eating disorders was compared with a control group in only two studies (
Table 1) and resulted in a nonsignificant effect size of g=0.47 (95% CI=–0.17 to 1.12), and one study compared IPT with pharmacotherapy in nonresponders to CBT (g=0.18).
The Effect of IPT on Anxiety Disorders
The effect of IPT on anxiety disorders was examined in eight trials (see
Table 1 and Appendix F in the
data supplement). Anxiety outcomes of IPT were compared with those of another psychotherapy in six studies and resulted in a small, nonsignificant difference (g=–0.16) in favor of the alternative therapy (95% CI=–0.39 to 0.07; number needed to treat=11), with low heterogeneity (I
2=21; 95% CI=0–69). These studies had sufficient power to detect an effect size of g=0.38. In the studies with low risk of bias, we found a significant effect of the alternative therapies over IPT (g=–0.33; 95% CI=–0.59 to –0.06; number needed to treat=5; I
2=13; 95% CI=0–76). Five studies reported follow-up outcomes, but the follow-up periods varied from 3 to 12 months, and therefore long-term effects were not examined.
IPT was compared with control conditions in three studies, and this resulted in large and significant effect sizes for anxiety outcomes (g=0.89; 95% CI=0.22–1.56; number needed to treat=2; I2=58; 95% CI=0–86) and depression outcomes (g=0.82; 95% CI=0.45–1.19; number needed to treat=2; I2=0; 95% CI=0–73). Only one of the three studies had a low risk of bias.
The Effect of IPT on Other Mental Health Disorders
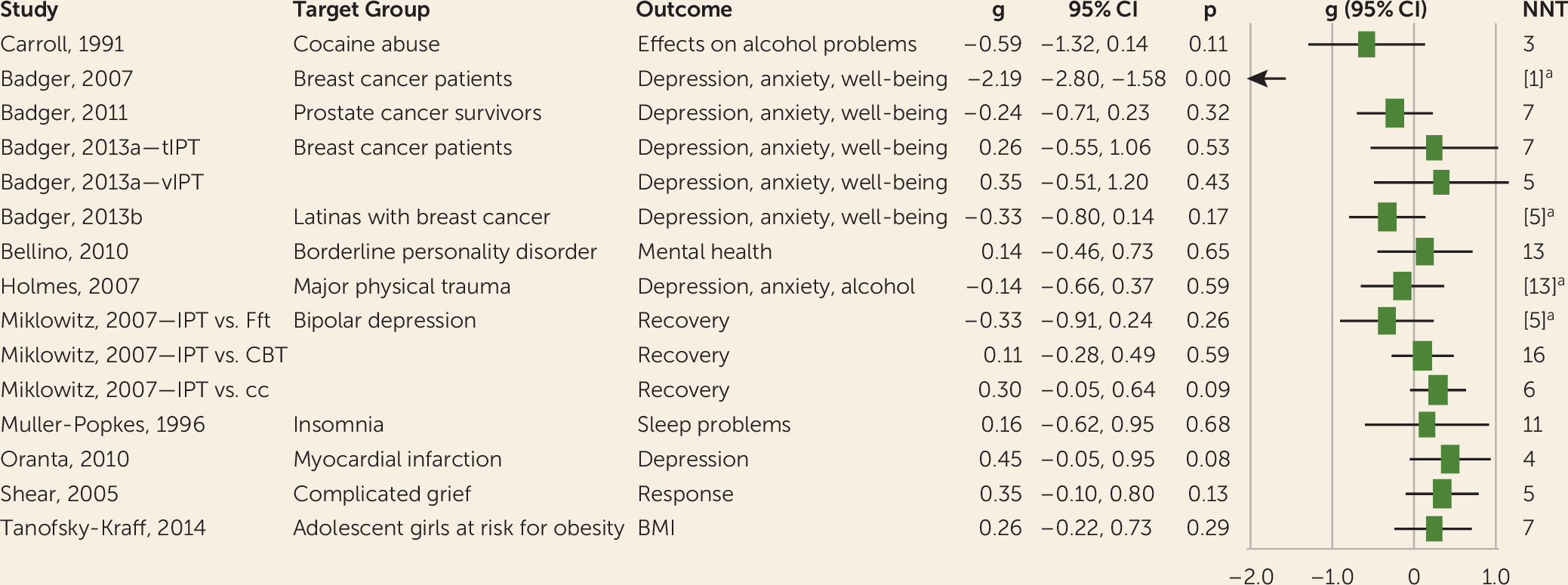
We identified 12 trials in which IPT was used to treat other mental health problems, ranging from other mental disorders to distress in patients with general medical disorders, substance abuse, and obesity risk in girls (
Figure 2). Because these trials were singular studies, the effect sizes were not pooled and no further analyses were conducted.
Discussion
We conducted the most complete meta-analysis, to our knowledge, of trials on IPT to date and identified 90 randomized trials on IPT for mental health disorders. Two-thirds of these studies were aimed at prevention, treatment, and relapse prevention of depression, showing a moderate-to-large effect on depression compared with control groups, with smaller effects in older adults, in clinical samples, and in samples meeting diagnostic criteria for a depressive disorder. IPT was not significantly more or less effective than other psychotherapies for depression. There were some indications that pharmacotherapy may be somewhat more effective than IPT for acute-phase depression; however, this finding was not robust and may have been influenced by the high risk of bias in many of these trials. Combined treatment was significantly more effective than IPT alone but not more effective than pharmacotherapy alone. This should be considered with caution, however, because of the relatively small number of trials. These results are comparable to our earlier meta-analysis of studies on IPT for depression (
3).
We found indications that IPT may prevent the onset of depressive disorders in subthreshold depression, which is in line with meta-analyses of this field (
6,
39). However, the finding that IPT may prevent the onset of depressive disorders has not been established in earlier meta-analyses. These findings should be considered with caution because the number of trials on prevention was small, risk of bias was considerable, and the confidence intervals were broad.
The trials examining the effects of maintenance IPT on recurrence and relapse also revealed significant effects of IPT. But again, these findings were limited by the small number of trials, considerable risk of bias, and broad confidence intervals.
We also found that the outcomes of IPT in depression were associated with the number of sessions, with 10 or more sessions resulting in an increase of the effect size with g=0.2. Although results of such metaregression analyses are not causal evidence, this may indicate that 16-session IPT is more effective than the shorter interpersonal counseling, a finding that needs confirmation in future research.
The applications of IPT to other disorders emerged in response to symptoms and morbidity (e.g., binge eating, social anxiety) being bidirectionally linked with interpersonal stressors and the importance of social supports and relationships to health and resilience (
40–
42).
In the treatment of eating disorders and anxiety disorders, IPT has been used in numerous studies as an active comparison group. No earlier meta-analysis has examined the effects of IPT in these disorders. Overall, these studies showed no convincing evidence that CBT is more effective than IPT in anxiety disorders. In eating disorders, a small but significant effect in favor of CBT was found for behavioral outcomes, but because the number of studies was small and risk of bias was high, this is uncertain, and longer-term effects are not clear.
IPT trials for other mental health problems, including addictions and distress from general medical disorders, showed some promising effects. However, this should be considered with caution because of the high risk of bias in most trials and the insufficient number of trials.
This meta-analysis examined a broad range of mental health problems in a large number of patients using one treatment method, IPT. There are, however, limitations to the conclusions that can be drawn. The number of trials for several comparisons was too small to make reliable estimates of the effects, and heterogeneity was considerable in several analyses. Furthermore, risk of bias was high in the majority of trials, reducing the strength of the evidence considerably. However, when we limited the analyses to studies with low risk of bias, the outcomes were very comparable to those found for all studies. In addition, because only a small number of studies examined long-term follow-up outcomes and these follow-up periods differed, these outcomes could not be examined. Finally, the results of randomized trials may not be generalized to patients who are treated in routine care because of the exclusion criteria used in the trials. Although this problem has not been found to affect the outcome of these trials (
43), these limitations should be kept in mind when interpreting the outcomes of our study.
In conclusion, IPT is one of the best-examined treatments in mental health problems, and it is effective in depression and possibly in other disorders, such as eating and anxiety disorders. It is important to have more than one treatment option for patients, since no treatment works for everyone, and IPT, with its focus on salient relational and interpersonal experiences, provides an important alternative to pharmacotherapy or CBT. IPT has the potential to be used more broadly for endemic mental health problems, as a preventative treatment, and to address the concomitant interpersonal stressors associated with the onset or worsening of disorders.