To enhance the accuracy of diagnosis and facilitate earlier detection in clinical settings, the diagnostic criteria for bipolar disorder in DSM-5 emphasize changes in activity or energy as a core symptom of mania or hypomania (criterion A) in addition to changes in mood. In contrast, DSM-IV criteria included increased goal-directed activity or psychomotor agitation as one of several secondary criteria (criterion B). Other changes from DSM-IV to DSM-5 criteria include the new specifier “with mixed features,” which can be applied to episodes of mania or hypomania when depressive features are present, as well as to episodes of depression when features of mania or hypomania are present.
Elevated activity or energy is a key symptom of mania (
1). Psychomotor pressure and increased motor activity have been described in 85%−95% of mania cases (
1), and previous studies supporting the inclusion of “increased activity or energy” in criterion A noted that it was as important as elevated mood in the clinical picture of mania (
2,
3). In DSM-III-R, elevated motor activity was the most prevalent symptom in subjects diagnosed with a manic episode (
4), and other studies noted that this symptom was more prevalent in individuals with bipolar disorder than in subjects with schizophrenia or healthy comparison subjects (
4). Angst et al. (
3), after evaluating a subsample of 591 subjects with bipolar disorder from a 20-year cohort of 4,547 subjects, proposed that overactivity, which is directly associated with increased activity or energy, should be included as a key criterion of hypomania in addition to euphoria and irritability. In addition, changes in energy and activity are more likely than changes in mood to be noticeable and/or documented by patients and family members.
In diverse studies that have used factor analysis to investigate the phenomenology of mania, hyperactivity and increased energy have been described as key factors across the entire spectrum of mania severity, suggesting that elevated motor activity is not only a key clinical feature of mania but is also more important than mood changes (
5–
9). In patients with bipolar II disorder or major depressive disorder, Benazzi and Akiskal (
8) noted that “energized-activity” and “irritability-racing thoughts”—but not euphoria—were cardinal symptoms for the diagnosis of hypomania. Similarly, Benazzi (
7) reported that hyperactivity was the most common symptom retrospectively identified by patients with bipolar II disorder as well as the one most strongly associated with this diagnosis; in that study, no association between hyperactivity and euphoria or irritability was observed. Moreover, Akiskal et al. (
6) proposed new diagnostic criteria for mania, suggesting that psychomotor activation was the key criterion for mania, while mood changes (elation, depression, anxiety, etc.) were hierarchically less important than psychomotor activation for diagnosis.
It should be noted that mild positive mood changes may be misdiagnosed as hypomania when activity levels are not taken into account. Along these lines, focusing on increased activity rather than just elevated mood or irritability may more successfully identify hypomania in bipolar II disorder (
2,
3). One issue of particular concern is that up to 40% of bipolar II patients may be erroneously diagnosed with major depressive disorder (
10). This underdiagnosis of bipolar disorder, as well as the concomitant changes in diagnostic accuracy in mood disorders, is associated with diverse factors that may result in inadequate treatment (
11). For instance, such individuals have an average delay of 7–10 years before they are diagnosed correctly (
12). This is particularly important because misdiagnosed individuals often receive inappropriate treatments for many years—particularly antidepressant pharmacotherapy without mood stabilizers. A recent analysis from the international, multisite Bipolar Disorder: Improving Diagnosis, Guidance, and Education (BRIDGE) study that evaluated more than 5,000 subjects with major depressive disorder emphasized the benefits of improving the specificity of the hypomania diagnosis by requiring mood plus increased activity or energy for the diagnosis (
13,
14).
In this study, we sought to assess the diagnostic validity of the new DSM-5 criterion of increased activity or energy levels by analyzing point prevalence data from the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD) study at the initial visit. Specifically, we evaluated differences between patients who met the DSM-5 criterion of increased activity or energy levels (in addition to meeting all DSM-IV criteria) and those who did not (that is, individuals who met DSM-IV criteria but not the more stringent DSM-5 criterion of increased activity or energy levels) regarding 1) diagnostic prevalence, 2) clinical and concurrent validators, and 3) longitudinal outcome. We hypothesized that the new DSM-5 criterion would reduce the prevalence of mania and/or hypomania.
Method
Data for this study were drawn from the STEP-BD study, a multicenter observational and effectiveness study with a hybrid design sponsored by the National Institute of Mental Health and conducted at 22 treatment sites (reviewed in reference
15). The main objective of STEP-BD was to determine which treatments were more effective for bipolar disorder across broad inclusion criteria. The study was approved by the institutional review board of each participating institution.
STEP-BD enrolled 4,360 outpatients from academic and nonacademic treatment settings across the United States (
16). To be included in the study, patients were required to be at least 15 years old, to be able to give consent, and to meet criteria for bipolar disorder (type I, type II, or not otherwise specified), cyclothymia, or schizoaffective disorder (bipolar subtype, which incorporates manic symptoms). All participants met DSM-IV criteria for bipolar disorder. The database includes well-characterized subjects who sought outpatient treatment. All participants received a standard assessment, participated in naturalistic or randomized treatment, and provided written informed consent before entering the study.
The present analysis examined the STEP-BD data set to assess the effect of a single DSM-5 primary criterion—that of increased activity or energy levels—on diagnostic prevalence. Specifically, we compared those individuals with bipolar disorder who met the DSM-5 criterion of increased activity or energy levels (as well as meeting all DSM-IV criteria) to those who did not. We evaluated up to 1 year of longitudinal data for subjects with bipolar disorder (types I and II).
Assessments
All patients were systematically evaluated at study entry for medical and psychiatric history, presence of mood or psychotic symptoms, and other illness characteristics using the Mini-International Neuropsychiatric Interview and the Affective Disorders Evaluation adapted from the Structured Clinical Interview for DSM-IV Axis I Disorders (
17,
18). Of the 4,360 patients originally enrolled in the STEP-BD study, 310 met DSM-IV criteria for a manic or hypomanic episode at study entry. This was determined using DSM symptoms assessed via the Clinical Monitoring Form, an assessment tool focused on symptoms and treatment status that was the primary data collection tool for clinical evaluations in the STEP-BD study. The Clinical Monitoring Form is used to record clinician-rated symptoms over the course of the previous week; symptoms were counted as present if the patient had a score ≥1 on that item. Notably, individual symptoms were used instead of categorizations by clinicians in order to facilitate understanding of how change in individual symptom criteria might alter diagnosis. Interrater reliability among the STEP-BD physicians for DSM-IV manic and depressive symptoms was high (intraclass correlation coefficients, 0.83–0.99) (
19).
At follow-up visits, standardized clinical assessments were similarly performed using the Clinical Monitoring Form. Data were examined during a 1-year period (at baseline, 6 months, and 12 months). It should be noted that the present analysis assessed the impact of a single DSM-5 primary criterion A symptom—that of increased activity or energy levels—on diagnostic prevalence, clinical validators, and 12-month outcome; it did not include psychomotor agitation as a primary mania criterion. The specific question from the Clinical Monitoring Form used for this analysis involved the presence of more goal-directed activity than usual over the past week. A secondary analysis using data from the Clinical Monitoring Form examined patients’ current clinical status as an indicator of mood state as assessed by the evaluating clinician. Only patients listed as experiencing a manic, hypomanic, or mixed episode were included, except as otherwise noted.
Statistical Analysis
Demographic characteristics were compared between those who met the DSM-5 criterion and those who did not using chi-square tests for categorical variables and t tests for continuous ones. To examine changes in symptoms over the course of the first year in the study, linear mixed models were used with a first-order autoregressive covariance structure with time and group in a factorial model with restricted maximum-likelihood estimates. Bonferroni post hoc tests were used to examine significant omnibus effects. The significance threshold was set at 0.05, two-tailed. All analyses were performed using IBM SPSS Statistics, version 21.0.0.2 (IBM, Armonk, N.Y.).
Results
Table 1 summarizes the demographic and clinical characteristics of the 310 patients who were experiencing a manic or hypomanic episode at study entry based on symptoms from the Clinical Monitoring Form. All 310 patients met DSM-IV criteria for a manic or hypomanic episode, and 52% also met the stricter DSM-5 criteria (that is, DSM-IV criteria plus the additional DSM-5 criterion of increased activity or energy levels). Patients were evaluated in groups determined by whether they met DSM-5 criteria (N=160) or did not (N=150). The prevalence of mania and hypomania was 8.3% by DSM-IV criteria and 4.3% by DSM-5 criteria. Clinical and demographic comparisons showed that on average, the DSM-5 group had a higher annual income, more comorbidity with obsessive-compulsive disorder, and less DSM-IV-diagnosed major depressive disorder than those who did not meet DSM-5 criteria (
Table 1). Only the difference with major depressive disorder remained significant after Bonferroni correction.
When all patients with available data were included, increased activity was associated with elevated mood (χ
2=526.30, p<0.001; odds ratio=14.56) and irritability (χ
2=112.02, p<0.001; odds ratio=3.82). Elevated mood and irritability were also related (χ
2=409.50, p<0.001; odds ratio=6.12) (
Table 2). The odds ratio was highest for increased activity and elevated mood. In an analysis in which the three symptoms were combined, the association between elevated mood and increased motor activity was significant whether patients had irritability (χ
2=131.66, p<0.001; odds ratio=8.00) or not (χ
2=314.45, p<0.001; odds ratio=18.88). Furthermore, all three of the primary symptoms of mania—changes in mood, increased energy or activity, and irritability—were present in 62% of patients who met DSM-5 criteria for mania or hypomania. Sixty-nine percent of patients who were not experiencing a manic or hypomanic episode displayed none of the three primary manic symptoms (
Table 3).
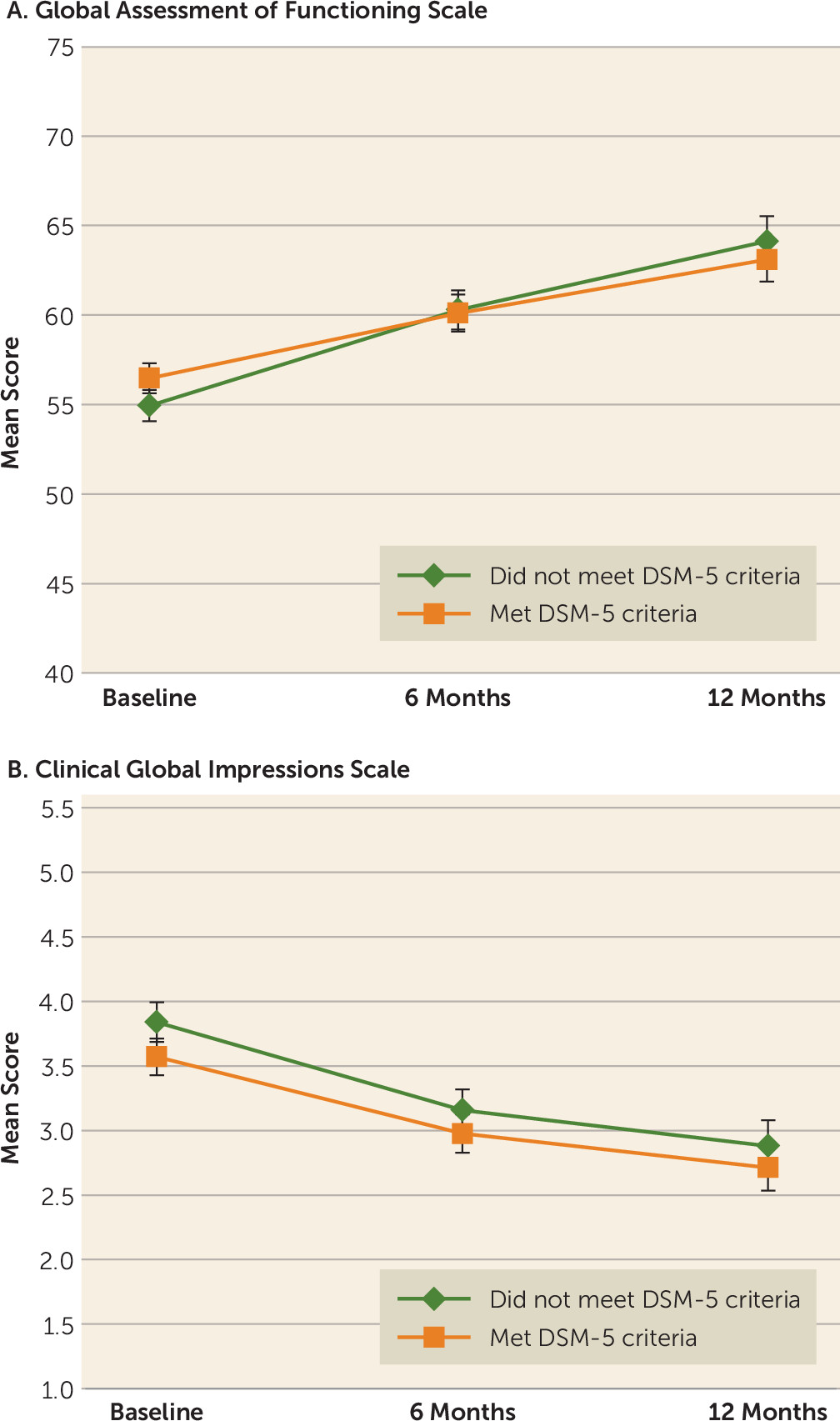
No differences in clinical rating scales were observed at 1-year follow-up between those who met DSM-5 criteria at baseline and those who did not (
Figure 1). Specifically, no between-group differences in Global Assessment of Functioning (GAF) scores were observed at baseline, at 6 months, or at 12 months. For the overall sample, a significant improvement in GAF scores from baseline was observed at 6 months (p<0.001) and at 12 months (p=0.003). Similarly, Clinical Global Impressions scale scores did not differ between groups at any time point, but scores had improved significantly from baseline at 6 months (p<0.001) and at 12 months (p<0.001).
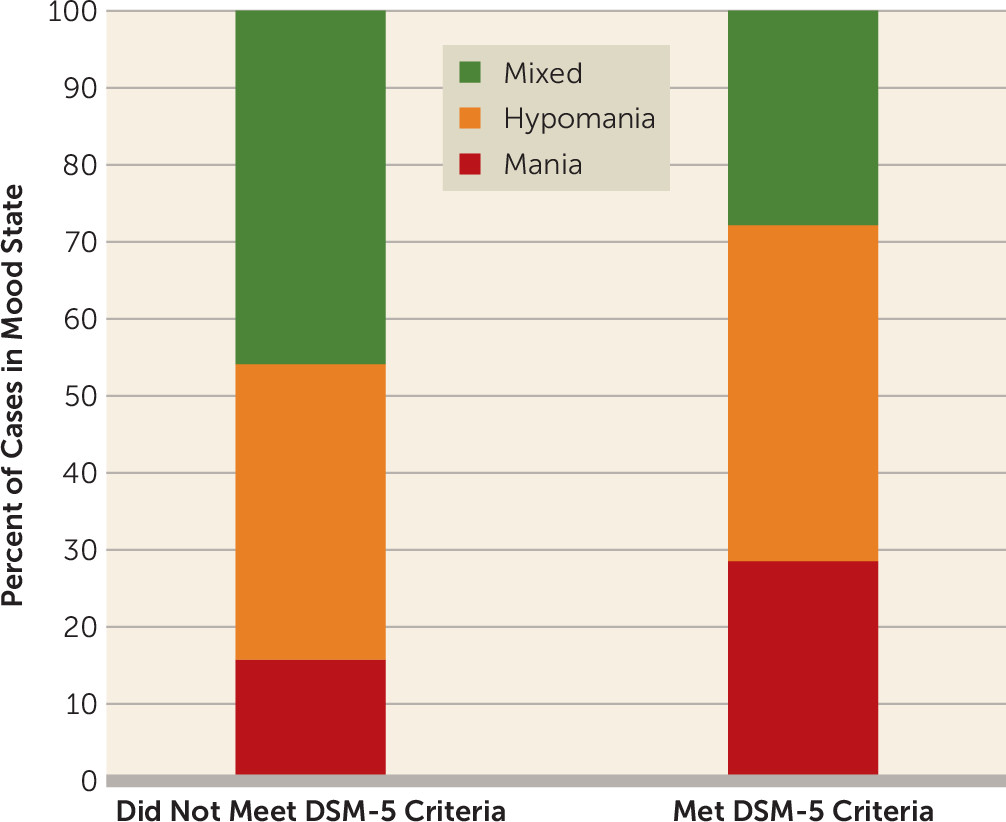
Using the Clinical Monitoring Form to show point prevalence, clinicians categorized the type of episode a patient was currently experiencing at the initial visit.
Figure 2 illustrates the prevalence of DSM-5 diagnosis by episode type. Of the 310 patients who met DSM-IV criteria for a manic or hypomanic episode, 112 (36%) were experiencing a hypomanic episode, 61 (20%) were experiencing a manic episode, and 100 (32%) were experiencing a mixed episode; the remaining 37 (12%) patients were in cyclothymic and other states. For those characterized as hypomanic, 54% met DSM-5 criteria. Sixty-six percent of patients characterized as manic and 39% characterized as being in a mixed episode met DSM-5 criteria. The distribution of DSM-IV criterion A symptoms is summarized in
Table 3.
It should be noted that patients met entry criteria into the STEP-BD study for bipolar disorder through methods other than the Clinical Monitoring Form, but many of these patients would not have met full mania criteria based on the Clinical Monitoring Form questions. Of those patients previously diagnosed as manic using DSM-IV criteria based on the Clinical Monitoring Form, 45% met DSM-5 criteria for “major depressive episode with mixed features.”
Discussion
In this sample from the STEP-BD study, adding “abnormally and persistently increased activity or energy” as part of criterion A for hypomanic and manic episodes in DSM-5 decreased the prevalence of mania and hypomania; this change was assessed using the Clinical Monitoring Form via the additional question on increased goal-directed activity. Changes in cross-sectional diagnosis were more robust for hypomania and mixed episodes than for mania. For hypomania and mixed episodes, only 54% and 39% of patients, respectively, kept the same diagnosis of bipolar disorder using DSM-5 criteria. However, compared with DSM-IV criteria, these expanded criteria affected point prevalence at the baseline visit but did not alter clinical and concurrent validators or 1-year longitudinal outcome when examined in the context of multiple visits for a given patient.
When we examined symptoms at the baseline visit, we found that using the single DSM-5 criterion of increased activity or energy levels reduced the identified number of manic and hypomanic episodes by 48%. Interestingly, the BRIDGE study, which assessed diagnostic criteria for bipolar disorder in a sample of 5,635 patients with DSM-IV major depressive disorder, found that increased activity was a primary symptom of bipolar disorder. In that study, any of the three primary symptoms (changes in mood, increased energy or activity, and irritability) showed diagnostic validity on its own (
14).
These results suggest that the DSM-5 criteria for mania and hypomania may not only affect point prevalence (and potentially prevent overdiagnosis) for both mood states but also, because of their increased ability to differentiate diagnoses, may have an impact on the treatment of mood disorders (
7). Indeed, the change to criterion A was expected to decrease the overall prevalence of bipolar disorder while concomitantly improving diagnostic accuracy. The impact of requiring increased activity or energy as a criterion for the diagnosis of bipolar disorder—and its concomitant effects on treatment selection—is unclear and will require additional study.
Despite the altered point prevalence rates observed in this study when the DSM-5 criteria were used, no impact on outcome was noted in the 1-year follow-up. The magnitude of the odds ratio for the presence of motor activity associated with elevated mood and irritability supports an association among these key manic symptoms.
Nevertheless, the study has some limitations. Specifically, time spent in any mood episode was not evaluated; rapid cycling was not evaluated; there was no diagnostic evaluation of mood disorder (only episode prevalence was analyzed); and the role of comorbidities was not taken into account. In addition, our reliance on a single question on the Clinical Monitoring Form may have limited our ability to evaluate the relationship between diagnostic changes from DSM-IV to DSM-5, although it should be noted that good interrater reliability was present across sites. It is also important to mention that the STEP-BD study only included patients in tertiary care, so the present study was not based on a population-based, random, representative sample. As a result, data comparing the prevalence of DSM-IV-diagnosed versus DSM-5-diagnosed bipolar disorder require further replication in studies with samples drawn from a more generalizable population to confirm potential prevalence changes.
The DSM-5 criteria for mania and hypomania produced a large decrease in point prevalence, with no change in validity or other measures. The impact on point prevalence appears to be particularly remarkable. Specifically, the change in DSM-5 mania criteria reduced the frequency of mania or hypomania by nearly 50%. No difference was observed for most of the available validators when comparing the DSM-5 and DSM-IV criteria sets. Furthermore, and based on available information, a large percentage of those who did not meet DSM-5 criteria for mania now met criteria for major depressive episode with mixed features. Thus, it appears that the decision to include “mixed features” in DSM-5 was a beneficial one, as this is a key and extremely valuable specifier for making diagnoses across the continuum of mood disorders.
Indeed, depressive symptoms as well as full depressive episodes predominate in bipolar disorder; most individuals with bipolar disorder experience chronic depression much more frequently than mania or hypomania (
20,
21). In a longitudinal study, Judd et al. (
20,
21) observed that subjects with bipolar I disorder had depressive symptoms for 30.6% of the weeks observed, while only 9.8% of the weeks observed were spent in hypomanic or manic states. In addition, patients with bipolar II disorder had depressive symptoms for 51.9% of the weeks observed, while only 1.4% of the weeks observed were spent in a hypomanic state. Similar results have been described by the Stanley Foundation Bipolar Network, which found that individuals with bipolar disorder had depressive symptoms three times as often as they did manic or hypomanic symptoms over a 12-month period (
22,
23). The present findings from the STEP-BD data set further support the persistent presence of depressive symptoms over the course of bipolar disorder.
It should be noted that only a relatively small proportion of patients in the total sample experienced a manic or hypomanic episode. Because patients with bipolar disorder spend three times as much time experiencing depressive symptoms as mania or hypomania (
24), we expected to observe only a relatively small proportion of patients with mania or hypomania in a sample with broad entry criteria such as this one, especially considering that patients spent some time well and not ill. In addition, this was a long-term outpatient study, which may explain the small proportion of recruited STEP-BD participants experiencing a manic, hypomanic, or mixed episode.
Despite these limitations, taken together, our results indicate that the new DSM-5 criteria may affect the diagnostic prevalence of manic or hypomanic episodes as well as the overall diagnosis of bipolar I and II disorder. Ultimately, these differences may affect the number of individuals clinically diagnosed with bipolar disorder during initial episodes and their treatment course (i.e., whether they are treated with mood stabilizers, atypical antipsychotics, and/or antidepressants). In addition, these findings suggest that the new DSM-5 criteria may directly affect the diagnostic prevalence of both major depressive disorder and bipolar disorder by potentially increasing the first and lowering the second, while nevertheless potentially supporting their existence along a continuum. Overall, our findings suggest that the inclusion of increased activity or energy levels as a DSM-5 criterion A symptom for manic episodes decreases point prevalence rates of mania and hypomania but does not affect longitudinal clinical outcomes.
Acknowledgments
The authors gratefully acknowledge the support and funding of the Intramural Research Program at NIMH, and they thank the 7SE research unit and staff for their support.