Physicians have described women with acute psychiatric symptoms after childbirth for millennia. In the 19th century, the first case series appeared, of which Esquirol’s was the most detailed (
1). He described 92 women with postpartum psychosis, of which 53% had predominantly manic symptoms, 38% had depressive symptoms, and 9% had nonaffective psychosis. French psychiatrist Louis-Victor Marcé (for whom the international Marcé Society for Perinatal Mental Health is named) published a monograph in 1858 that included detailed clinical descriptions of 79 women with postpartum disorders (
2). Although these cases might include women with infection and delirium, the striking affective and psychotic presentation of women with postpartum psychosis has been consistent over the last centuries. We present two cases—one in the woman’s own words and another as reconstructed from interview by the patient’s treating physician—to demonstrate presentations of postpartum psychosis.
The relationship between birth and psychosis has intrigued investigators who have hypothesized a distinct pathophysiology; however, the fundamental molecular and cellular mechanisms underlying postpartum psychosis remain elusive. This disorder is officially registered as a rare psychiatric disease in
Orphanet (
3), but postpartum psychosis does not have an official DSM code. Much of this literature has been generated in Europe, and severe mood disorders (such as mania without psychosis) have been included in the umbrella term “postpartum psychosis” based on the relationship of the episode with childbirth. In the present review, we provide a summary of the epidemiology, phenomenology, pathophysiology, course, and prognosis of postpartum psychosis, as well as diagnostic recommendations, treatment options, and strategies for prevention.
Presentation and Course
The dramatically increased risk of postbirth affective disorders has been confirmed in large-scale epidemiologic studies (
4–
6). The incidence of first-lifetime onset postpartum psychosis from population-based register studies of psychiatric admissions varies from 0.25 (
4,
7) to 0.6 (
1) per 1,000 births. These studies presented inpatient admission rates and did not include women treated in an outpatient setting or those who remained untreated. Although the absolute prevalence is low, the relative risk for the first onset of affective psychosis is 23 times higher within 4 weeks after delivery compared with any other period during a woman’s life (
4). Moreover, the incidence of new-onset affective psychosis is very low during pregnancy and significantly less frequent than outside the postpartum period.
In addition to first-onset affective psychosis, the postpartum period is also a high-risk period for relapse among women with known psychiatric illness. Women with bipolar disorder are more likely to experience a puerperal psychiatric admission compared with women with other psychiatric diagnoses (
5,
7–
9). Moreover, women with bipolar disorder are also at risk for episodes during pregnancy, especially when they taper off medication.
Multiple studies examining naturalistic cohorts of women with postpartum psychosis have documented the typical time of symptom onset as between 3 and 10 days after birth (
5,
10,
11). The onset of relapse in postpartum women with bipolar disorder has been observed to be earlier, sometimes during or immediately after delivery (
12,
13). Psychiatric admission typically occurs days or weeks after the onset of symptoms.
Early or prodromal symptoms of postpartum psychosis include insomnia, mood fluctuation, and irritability, with emergence of mania, depression, or a mixed state. Although rapid mood fluctuations are a hallmark of the disease, women suffering from postpartum psychosis often have symptoms that are atypical in patients with bipolar disorder. For example, mood-incongruent delusions are common and often related to the theme of childbirth. Disorganized, unusual behavior and obsessive thoughts regarding the newborn frequently occur. Postpartum psychosis is notable for its delirium-like appearance, with cognitive symptoms such as disorientation, confusion, derealization, and depersonalization. Women have a relatively low incidence of symptoms such as thought insertion, withdrawal or broadcasting, passivity experiences, hallucinatory voices giving running commentary, or social withdrawal (
11,
14–
18). Delusions of altruistic homicide (often with associated maternal suicide) to “save them both from a fate worse than death” may occur and are an important exploration within the clinical examination (
19). Postpartum psychosis is associated with an increased risk of both suicide and infanticide (
5).
A Dutch naturalistic cohort study reported an episode duration of 1 month for women with manic features compared with 2.5 months for patients with mixed or depressed features. These times are similar to the median duration of episodes in patients with bipolar disorder (
11,
20). Patients with a shorter duration of the acute episode of postpartum psychosis have a more favorable prognosis compared with patients with longer episodes (
21,
22). The prognosis for patients with first-onset postpartum psychosis is more favorable than that for the first onset of affective psychosis outside the postpartum period (
21–
24).
Following a first episode of postpartum psychosis, some women will experience nonpuerperal mood episodes, for which the postpartum psychosis is the first presentation of a severe, life-long mood disorder (
23,
25–
28). After an incipient postpartum affective psychosis, a woman has a 50%−80% chance of developing another serious psychiatric episode, usually within the bipolar spectrum (
29,
30). For 20%−50% of women, affective psychosis remains limited to the postpartum period (
23,
25–
28). The wide ranges are due to variability in figures from the few studies available. Women with postpartum psychosis usually have one of two disease courses: 1) isolated postpartum psychosis (vulnerability to affective psychosis only after birth) or 2) postpartum psychosis as an expression of bipolar mood disorder with nonperinatal episodes.
Etiology
Postpartum psychosis is among the few psychiatric disorders in which a clear etiological event is definable. Although childbirth is a trigger for postpartum psychosis, many important questions regarding its pathophysiology remain unanswered. A significant predictor is primiparity; therefore, if a woman’s first delivery is not complicated by postpartum psychosis, the likelihood becomes substantially lower after a subsequent delivery (
31). In contrast to postpartum unipolar depression, life events and social stress are not implicated in the etiology of postpartum psychosis (
32,
33). Moreover, investigators have not consistently identified obstetric risk factors for first-lifetime onset of postpartum psychosis (
7,
34). Conducting neurobiological studies of patients with postpartum psychosis is a challenge due to the low incidence of the disorder combined with the acute severity. Presumably, the mechanism of onset is related to specific physiological changes at birth in genetically vulnerable women. Here, we review the related genetic research and potential physiological postpartum triggers (endocrine, immunological, circadian).
Genetic studies in women with first-lifetime onset postpartum psychosis are absent, but the vulnerability for postpartum relapse in women with bipolar disorder has been investigated. Postpartum psychiatric episodes may be a marker of a familial form of bipolar disorder (
35,
36). In a major step toward identifying causative etiological factors, Jones and Craddock (
35) identified the enrichment of specific genetic variants of the serotonin transporter gene (5-HTT) and a genome-wide significant linkage signal at chromosome 16p13 in patients with a history of bipolar disorder and postpartum psychosis (
37,
38). Exploration of estrogen receptor or glucocorticoid receptor gene polymorphisms in relation to postpartum psychosis has not established an association (
39,
40). Encouraging for research potential, a perinatal psychiatry genetic consortium, a large-scale collaborative research effort to disentangle the pathophysiology of postpartum psychiatric disorders including postpartum psychosis, has been established (
35).
Little research has been targeted at understanding the hormonal correlates of postpartum psychosis, and the majority of studies were performed two decades ago. During pregnancy, levels of estrogen and progesterone (among other hormones) rise exponentially. Around 35 weeks gestation, corticotropin-releasing hormone (CRH)-binding protein declines and results in a surge of CRH and ACTH, which precede parturition. After birth, the precipitous drop in estrogen and progesterone levels occurs, and these hormones normalize within 3 weeks (
41). This many-fold concentration change in reproductive hormone levels associated with parturition has been implicated in the etiology of postpartum psychosis (
42). Because estrogen mediates dopaminergic tone in the hypothalamus, the onset of affective psychosis after childbirth was reported to result in an increased sensitivity of dopamine receptors (
42); however, others have not replicated this finding (
43). If the rapid decline in estrogen concentrations is the trigger for postpartum psychosis, immediate postbirth administration might prevent psychosis. However, data from open trials include a small case series suggesting efficacy with a high-dose oral estrogen-tapering regimen after birth (
44) and a randomized trial demonstrating no impact of a regimen of transdermal estradiol on relapse in women at risk for postpartum mood disorders (
45).
An interesting relationship between cortisol and dopamine exists in relation to postpartum psychosis. Animal studies have suggested that glucocorticoid secretion in the postpartum period is regulated, in part, by the dopaminergic system (
46). However, the role of dopamine in glucocorticoid and prolactin secretion in postpartum women must be elucidated within the context of lactation. The release of oxytocin during suckling is associated with feelings of well-being and relaxation and a hypo-responsiveness to stressors. An interesting study conducted in the 1980s showed that one woman with postpartum mania had high levels of oxytocin metabolites (
47).
Evidence is limited regarding the influence of pregnancy hormones in the etiology of postpartum psychosis. In women with and without a history of postpartum depression or premenstrual dysphoric disorder, the role of changes in gonadal steroid levels has been investigated by simulating hormonal conditions related to pregnancy and parturition (
48,
49). Similarly, women at risk for postpartum psychosis may have differential sensitivity to rapid changes in the plasma concentrations of these hormones rather than having altered peripheral levels (
50,
51).
Postpartum activation of the immune system could be an etiologic contributor to the acute onset of mania, psychosis (
52,
53), anxiety, and depression (
52,
54–
56). Bergink et al. (
57,
58) have reported the co-occurrence of postpartum psychosis with thyroiditis and preeclampsia, which have established autoimmune and inflammatory etiologies, respectively. In addition, the investigators reported the identification of CNS auto-antibodies in 4/96 (4%) of patients with postpartum psychosis, which suggests autoimmune encephalitis in a subset of cases (
59). Two of these patients had anti-
N-methyl-
d-aspartate receptor (NMDAR) encephalitis, while for the other two patients the antigen was unknown. Furthermore, they observed abnormalities in monocyte activation, T-cell function, and tryptophan breakdown in patients with postpartum psychosis during the acute phase compared with postpartum control subjects (
52,
60). Specifically, many patients had a monocytosis and did not show the physiological T-cell elevation of the normal postpartum period. These findings support the notion that immunological mechanism(s) contributed to affective instability and psychosis.
Circadian rhythm disruption is common in postpartum psychosis (
61–
65). Investigators have consistently reported that women with psychosis have severe sleep disturbances, which often herald the psychotic symptoms in the postpartum period (
66,
67). Sleep disruption resulting from labor and delivery may initiate the circadian disruption and contribute to the emergence of an episode of mania or mixed state (
63). In first-time mothers, the early postpartum period is characterized by more wakings, a later onset of stage 4 and restorative REM sleep (
62), and sleep loss (
68).
In summary, postpartum psychosis is a psychiatric condition with a mechanism of onset related to specific physiological changes (e.g., hormonal, immunological, circadian rhythm) leading to disease in genetically vulnerable women. Whether these factors lead to a common pathway resulting in psychosis or whether postpartum psychosis is a heterogeneous disorder with multiple etiologic contributors are evolving research questions.
Diagnostic Considerations
Screening for perinatal depression was recommended by the U.S. Preventive Services Task Force (
69). An under-recognized concern is that postpartum women who screen positive for depression may have bipolar rather than unipolar disorder. In a large-scale screening study, 22.6% of screen-positive women had bipolar disorder (
70). Diagnostic clarification of screen-positive women through interview or the Mood Disorders Questionnaire (
71) is an important addition to the postpartum screening process. Additionally, a striking 14% of depressed women who had initial psychiatric contacts during the first postpartum month converted to a bipolar diagnosis within 15 years compared with 4% with a first psychiatric contact unrelated to childbirth (
72).
Women with postpartum psychosis require a high level of care, and inpatient psychiatric hospitalization is recommended for diagnostic assessment and treatment. Clinical symptoms vary widely. Even in an individual woman, rapid fluctuations in symptoms are referred to as “the kaleidoscopic picture of postpartum psychosis” (
73,
74). Assessment of mood and psychotic symptoms (including thoughts of the patient harming herself or her children) at multiple postpartum time points is useful for diagnostic and maternal and infant safety assessments. The diagnostic picture is typically as follows (also see
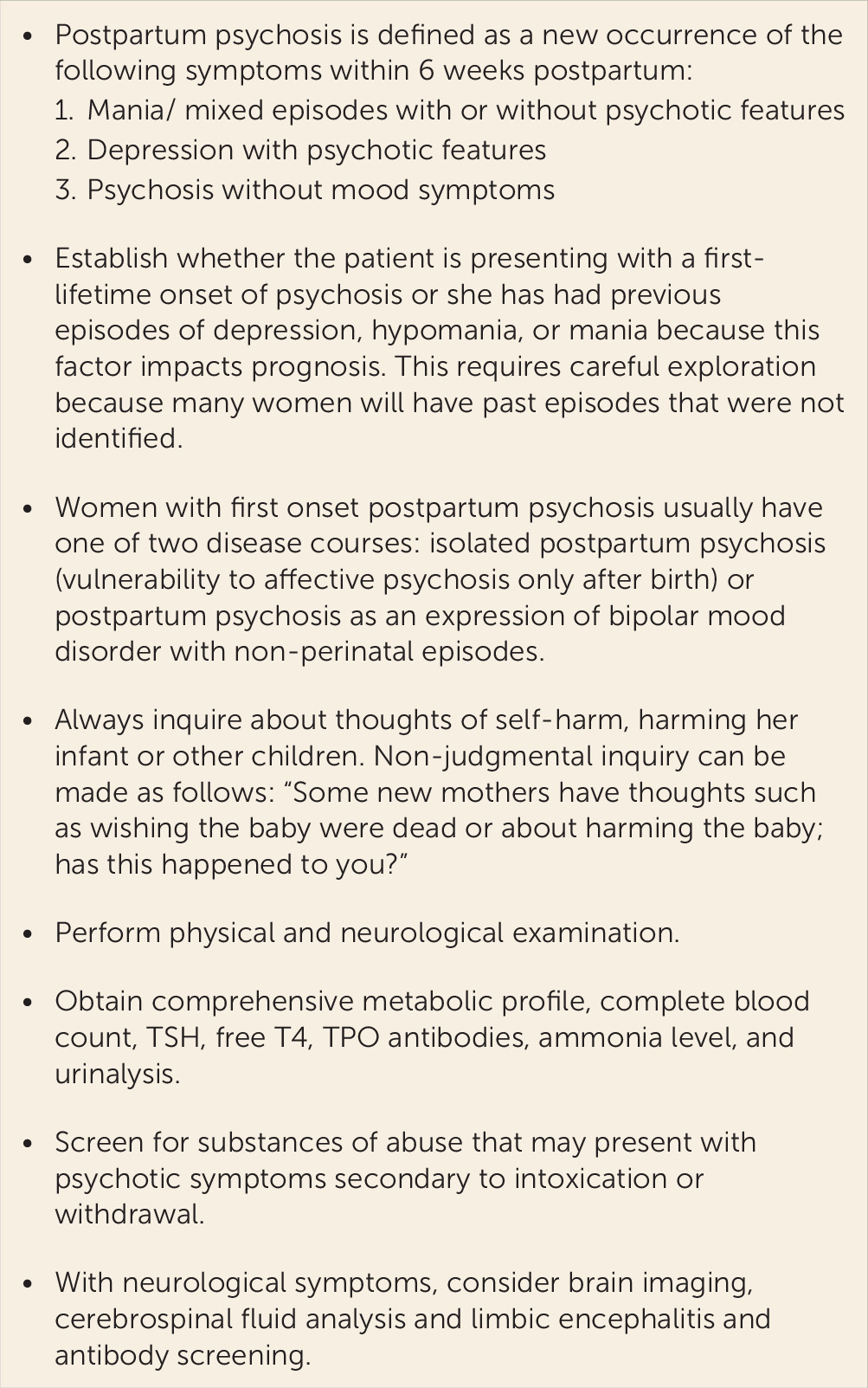
Figure 1):
1.
Mania or mixed episodes (with or without psychotic features);
2.
Depressive episodes with psychotic features; and
3.
Nonaffective psychotic episodes (occurring in <10% of cases).
Some women (variably estimated at 20%−50%) experience episodes only during the postpartum period, without recurrence outside this vulnerable time (
21,
23,
25–
28). Psychotic symptoms can be overlooked because they are either fluctuating or hidden (as in the second case presented in the introduction of this article). It is important to ask both the patient and her family about early symptoms of psychosis, such as paranoid ideas, thoughts others might consider unusual, or strong feelings of guilt. Depressed psychotic symptoms often include suicidal and infanticidal thoughts (e.g., my child is better off without me), and such patients require a higher level of care to ensure safety of the mother and infant. Assessment should include direct questions about suicidal and infanticidal thoughts. Patients may experience perceptual disturbances, both auditory and visual, with direct command for harmful actions. Examinations should include assessment for treatable causes of psychosis, including acute infection, peripartum blood loss and anemia, and exacerbation of predicting endocrine and/or autoimmune diseases. Laboratory testing should include a complete blood count to evaluate for an infectious process (including mastitis and endometritis), urinalysis to assess for cystitis, and a comprehensive metabolic screen. Primary hypoparathyroidism has been reported in a postpartum woman who presented with psychosis, stool incontinence, seizures, and hypocalcemia (
75). Thyroid autoimmune diseases occur in 5%−7% of women during the postpartum period (
76), and the percentage is higher in women with postpartum psychosis (up to 20%) (
57). Monitoring of thyroid function is advisable, especially in patients with thyroid peroxidase antibody positivity because these women are at the highest risk for thyroid dysfunction. We recommend measuring thyroid-stimulating hormone, free T4, and thyroid peroxidase antibodies both at the time of diagnosis and a few months later (
57). There is a well-documented postpartum rebound of thyroid peroxidase antibodies during the first months postpartum, and an initial negative screen immediately postpartum does not rule out thyroid disease.
Neurological symptoms, including seizures, decreased consciousness, dyskinesia, overt motor symptoms, and extrapyramidal symptoms raise the index of suspicion for anti-NMDAR encephalitis. Primary screening for NMDAR encephalitis can be done in serum, but false positivity is common, and CSF analysis is preferable (
59). Neurological symptoms are indication for an MRI to evaluate whether other brain pathology is present.
Lastly, childbearing is a physiological challenge to metabolic pathways that may become stressed by the extreme postbirth catabolic state. Previously unrecognized, late-onset inborn errors of metabolism can present with clinical features similar to postpartum psychosis. Clinical information important in the differential diagnosis is an abnormal neurological examination, seizures, and, in urea cycle disorders, a history of the patient’s avoidance of protein consumption (
77,
78). A serum ammonia concentration will identify the presence of a urea cycle disorder. A positive test can be followed by plasma amino acid analysis and further studies (
77,
78). A review of alcohol and substance use and drug screen should be performed to identify toxic or withdrawal syndromes that may present with psychotic symptoms.
Treatment
Postpartum psychosis is a psychiatric emergency that requires immediate psychiatric evaluation. In many countries, inpatient mother and baby joint admission units are the preferred treatment settings and are associated with improved satisfaction with care and reduced time to recovery (
79,
80). Rare mother-infant psychiatric services have been developed in the United States (
79), but care is usually delivered to postpartum women in standard mental health treatment settings. Involvement of the patient’s family or significant others is an important component of care. They typically bring the new mother for evaluation and are alarmed by the changes in her behavior. They are important allies in medication compliance, maternal and infant safety monitoring, and support of the evolving maternal role. The goals of treatment are not only to reduce psychiatric symptoms, but to support self-esteem, confidence in mothering, social and family function, and infant health and emotional development (
81).
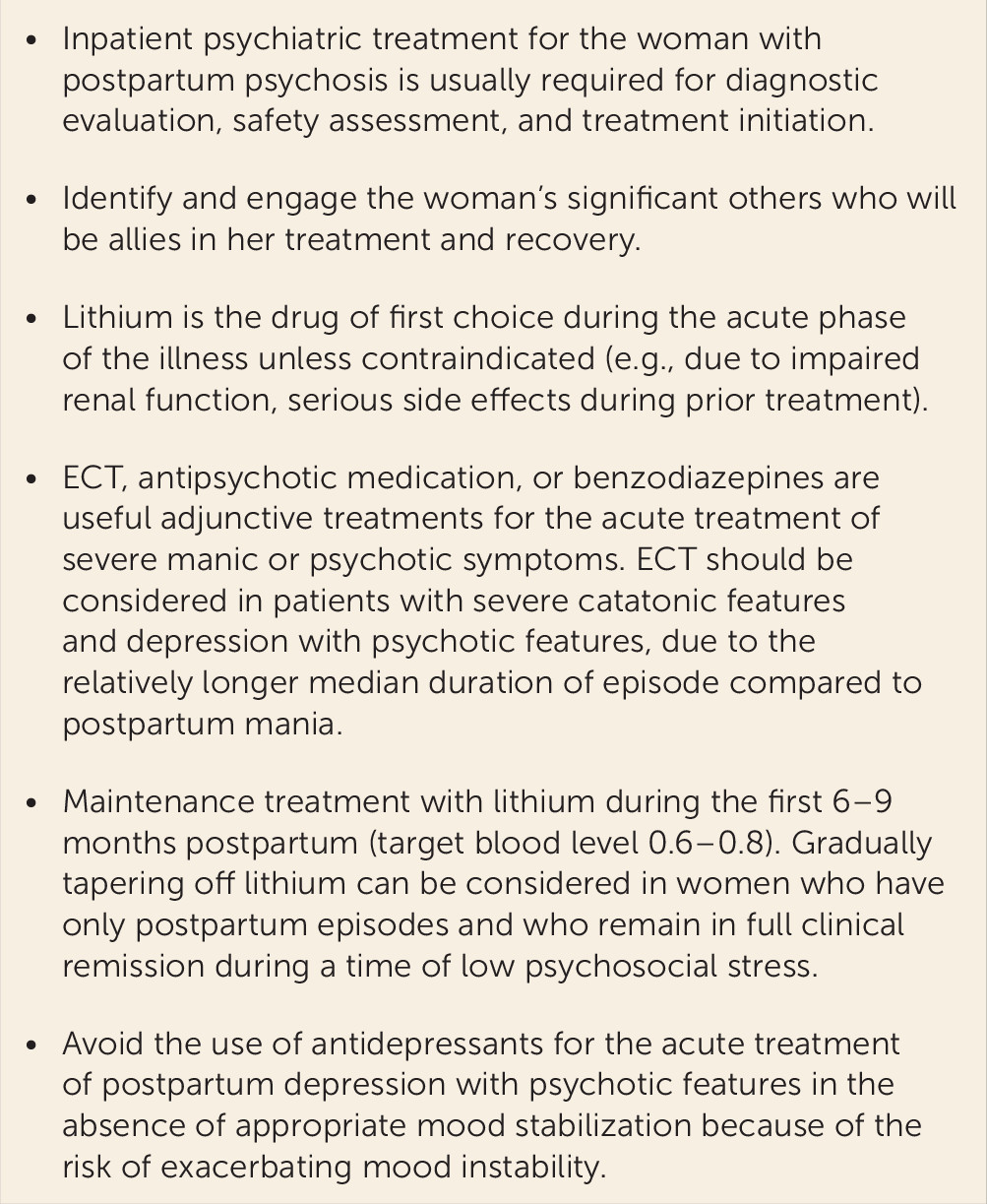
Less than 30 published studies describing the treatment of postpartum psychosis were found in the literature (
82). The majority of these are case reports describing a single patient, and very few studies include more than 10 patients. The largest evidence base exists for treatment with lithium, antipsychotics, and ECT, and we therefore discuss these treatment options. In case studies, lithium was an effective monotherapy (
83), and for adjunctive treatment (
84,
85). A recent naturalistic cohort study in 64 women provided evidence that lithium is highly efficacious for acute treatment of postpartum psychosis, as well as maintenance treatment (
86). The authors observed that nearly all patients (98.4%) achieved complete remission, with a median episode duration of 40 days. The treatment regimen included sequential administration of short-term benzodiazepines, antipsychotics, and lithium, with response monitoring. The drug sequence was designed to promote sleep, target psychosis, and stabilize mood, respectively. Women who remitted on antipsychotic monotherapy continued the drug as maintenance therapy, while the 48 women who required both antipsychotics and lithium to achieve remission were maintained on lithium monotherapy. At 9 months postpartum, sustained remission was observed in 79.7% of patients. Patients treated with lithium monotherapy had a significantly lower rate of relapse compared with those receiving antipsychotic monotherapy (
86). The authors of this study concur that most women with postpartum psychosis have a particularly robust response to lithium. In our opinion, lithium monotherapy is the preferred initial intervention for postpartum psychosis (see
Figure 2).
Antipsychotic treatment has been described in case reports on chlorpromazine, clozapine, pimozide, and quetiapine (
82,
87). The study described above (
86) demonstrated that antipsychotic monotherapy was efficacious in 20% of women within 2 weeks, after which nonremitted women were treated with lithium (
86). The overwhelming majority of patients responded to adjunctive lithium treatment and achieved clinical remission. The authors acknowledged the likelihood that more patients might have had a favorable response to antipsychotic monotherapy if they had been treated longer than 2 weeks; however, antipsychotic monotherapy was not protective for sustained remission, in contrast to lithium monotherapy.
Few studies have explored the efficacy of ECT in the treatment of postpartum psychosis (
88). In one case, treatment with chlorpromazine was ineffective, while ECT resulted in remission (
89). Similarly, a case series of five women with treatment-refractory postpartum psychosis described positive treatment outcomes with ECT (
90). A retrospective study compared the clinical responses to ECT in women with postpartum psychosis compared with nonpostpartum psychosis. The postpartum group was found to have greater clinical improvement following ECT compared with the nonpostpartum group (
91). In a study conducted in India, 34 women received successful ECT treatment, and it was proposed as a first-line treatment option (
92). However, in a cohort study, agitation, mania, and psychotic symptoms responded well to pharmacotherapy in 98% of cases (
86), and none of these patients required ECT. ECT is the primary treatment for patients with catatonia, severe agitation, or refusal to eat or drink. Moreover, ECT should be considered in patients with depression with psychotic features because of the longer median duration of episode (115 days) compared with postpartum mania (34 days) (
9).
Studies on the efficacy of circadian rhythm interventions to treat postpartum psychosis are lacking. Interesting treatment options include add-on treatment with blue-blocking glasses for patients in a postpartum manic state (
93).
The management of a breastfeeding woman with acute onset of psychosis is a challenging clinical situation that must be individualized. The well-established benefits of breastfeeding must be considered in the context of maternal mental health, which is the priority in this situation. Sleep deprivation due to frequent awakenings for breastfeeding may contribute to the onset and maintenance of mania, and re-establishment of regular circadian patterns is critical to recovery. Strategies to preserve sleep (another person to feed the infant at night, pharmacotherapy to support sleep) are critical for maternal well-being.
However, even seriously ill mothers with psychosis may insist on breastfeeding as a condition of treatment acceptance. In these cases, weighing the potential benefits and risks of breastfeeding with pharmacotherapy remains a clinical dilemma. Sparse data from mothers who provided paired mother-infant serum lithium concentrations are available to guide treatment (
94–
97). The range of the infant to maternal concentrations varied from 5% to 65%, with the infant level typically about 25% of the maternal level (
94). One infant became dehydrated during an infection and became toxic (level: 1.4 mEq/L) (
97). Although no serious adverse effects were observed in the majority of these breastfed infants, close observation and monitoring of thyroid and renal function was recommended. Few data are available for antipsychotic drugs; however, the infant doses of olanzapine, risperidone, quetiapine, ziprasidone, and aripiprazole received through breast milk have been estimated to be less than 5% of the maternal dose (
98). Limited use of short half-life benzodiazepine agents to promote sleep is preferred during the postpartum period, while chronic use of benzodiazepines during breastfeeding may result in infant sedation. The exposure of the breastfed infant to maternal medications may be reduced with the use of ECT (
92), which requires short-acting pharmacologic agents during the procedure. If the mother is breastfeeding, the patient and family caregivers should 1) be provided with breastfeeding support, 2) monitor the infant for signs of toxicity (poor suck intensity, decreased feeding, lethargy), 3) be educated about situations that elevate the risk for infant dehydration (reduced feeding/oral intake, excessive fluid loss, or fever), and 4) have access to a pediatric professional willing to monitor the infant under these circumstances.
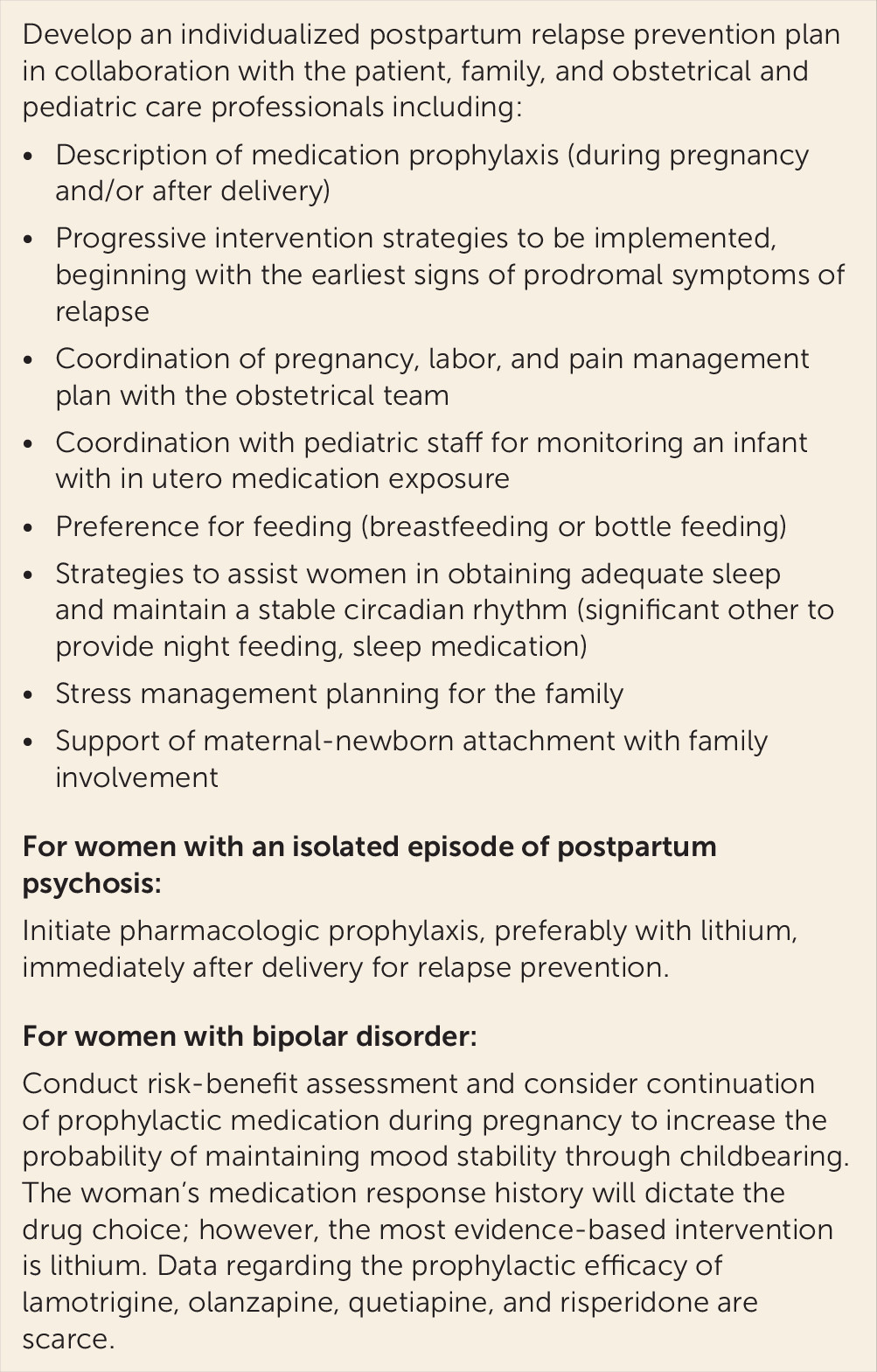
Prevention
Guiding women at high risk for psychosis through pregnancy and the postpartum period is a challenge for health care professionals (
99). The strongest risk factors for postpartum psychosis are a history of bipolar disorder and/or a history of postpartum psychosis (
8,
100). Total postpartum relapse rates for both groups are similar, but there are substantial differences in the approach to prophylaxis.
In a recent meta-analysis, the overall postpartum relapse risk was 37% in women with bipolar disorder (
101). In 17% of the cases, patients suffered from affective psychosis, mania, mixed episodes, or relapses that required hospitalization. The remaining patients had nonpsychotic affective episodes (mostly depressive and a limited number of hypomanic episodes). In women with bipolar disorder, postpartum relapse rates were significantly higher among those who were medication-free during pregnancy (66%, 95% confidence interval [CI]=57–75) compared with those who used prophylactic medication (23%, 95% CI=14–37) (
101). Clearly, the benefits of prophylaxis during pregnancy need to be carefully weighed against the risks to the fetus (also see
Figure 3). Few data are available to evaluate the efficacy of pharmacotherapy when it is initiated immediately after delivery as a prophylactic strategy in women who have not been treated during pregnancy. However, in all studies using prophylactic treatment with lithium, women with bipolar disorder had significantly lower rates of postpartum relapse (
102–
104). In contrast, valproate failed to demonstrate significant prophylactic benefits (
105). Olanzapine prophylaxis was equivocal, and further investigation of second-generation antipsychotics is warranted (
45,
105,
106); however, the established efficacy of lithium makes it the drug of first choice.
The overall relapse risk for women with only postpartum-onset psychoses is 31% (95% CI=22–42) as derived from 13 studies, 595 deliveries, and 528 patients (
107). The risk of a postpartum episode (affective psychosis, mania, mixed episode, or relapse requiring hospitalization) was significantly higher in patients with a history of postpartum psychosis (29%, 95% CI=20–41) compared with women with more chronic forms of bipolar disorder. Furthermore, in stark contrast to the high rates of relapse in women with bipolar disorder during pregnancy, women with a history of psychosis limited to the postpartum period are not at elevated risk of psychiatric episodes during pregnancy (
102). For this subgroup of women, prophylaxis using either lithium or antipsychotics immediately postpartum was highly effective in preventing postpartum relapse (
107).
We recommend different treatment algorithms for women with chronic bipolar disorder and women with a history of psychosis limited to the postpartum period. In women with bipolar disorder, prophylaxis during pregnancy increases the likelihood of maintaining mood stability during pregnancy and preventing postpartum relapse. In contrast, prophylactic treatment immediately after birth in women with a history of psychosis limited to the postpartum period is appropriate (
102).
Future Research
No randomized trials for the treatment of postpartum psychosis (
108) have been published; indeed, such trials would be challenging to conduct due to the low incidence. Fortunately, the majority of women with postpartum-onset psychosis experience remission with currently available interventions. Elucidating the biological determinants of women who are vulnerable to chronic forms of bipolar disorder compared with women who only experience relapse immediately following delivery is of great pathophysiological interest. Follow-up data will provide guidance to determine the duration of treatment following remission and quantification of the risk for conversion to bipolar disorder following a first-onset postpartum psychosis.
The reproductive events that occur throughout women’s lives can be conceptualized as a “longitudinal laboratory” (
109) for research hypothesis generation. Women act as their own controls across time for evaluating changes in state variables (present at the time of the episode) and trait variables (absent during active illness but indicative of risk for the disorder). Research advances result from elaborating our understanding of psychiatric disorders by discovering new relationships between factors that explain aspects of illness and wellness. Postpartum psychosis, although rare, is an example of a psychiatric disorder with rapid progression from wellness to severe disorder in association with the predictable event of birth. Repeated childbirth experiences may result in kindling (increased behavioral responsivity to the same stimulation over time) with progression to spontaneous episodes not associated with the triggering event (birth) (
110). Postpartum psychosis offers an intriguing model to explore etiologic contributions to the neurobiology of affective psychosis as reviewed in this article (genetic, hormonal, immune, circadian), as the boundary between psychiatric and neurological disorders fades and new interventions emerge.
We conclude where we began, with the observations of Louis Victor Marcé (
2), which remain true today: “Where subjects are predisposed to mental illness through either hereditary antecedents, previous illnesses, or through an excessive nervous susceptibility, pregnancy, delivery and lactation can have disastrous repercussions.”