Self-harm is the act of inflicting harm on oneself through the destruction of body tissue, ingestion of toxic substances, or other intentional acts, and it can occur with and without suicidal intent (
1). Self-harm is a leading risk factor for suicide and a major public health problem (
2–
4). In the United Kingdom, where this study is based, self-harm among adolescents is of particular concern. Between 2011 and 2014, the annual incidence of self-harm increased 68% among girls ages 13–16 (
3). The health care cost associated with self-harm is estimated at £162 million yearly, with the highest costs incurred by individuals under age 18 (
5). High self-harm-related costs are likewise observed in the United States (
6).
Some individuals who self-harm also inflict harm on others (
7–
11). There may be important antecedents that increase the risk of violent crime among people who self-harm. Identifying such antecedents could guide early prevention strategies and delivery of targeted interventions to reduce interpersonal violence. However, studies have primarily examined risk factors for self-harm among violent offenders
after they become clients of the criminal justice system (
12,
13). To appropriately target assessments and treatments, clinicians need information to identify who among self-harming adolescents is at greatest risk for violent offending. Our aim in this study was to characterize the risk factors that distinguish young people who engage in both self-harm and violent crime (“dual harmers”) from those who only self-harm, using data from a nationally representative cohort of British children followed across the first two decades of life.
Third, the longitudinal design enabled assessment of risk factors that antedate self-harm and violent crime. Problems in self-regulation are theorized to underlie both self-harm (
14,
17) and violent offending (
15,
18), and they may be important targets for intervention, so we tested whether dual harmers were distinguished by low childhood self-control. In addition, we examined three risk factors identified as salient predictors of self-harm or violent crime and severe psychopathology: maltreatment, childhood self-harm behavior, and family history of psychiatric disorders (
1,
15,
19). In response to external review, we also evaluated three secondary risk factors: low IQ, depression, and anxiety.
Fourth, we assessed participants’ self-harm features, clinical correlates, and life characteristics. This allowed us to draw a comprehensive picture of dual harmers’ psychosocial functioning. We examined self-harm method and frequency, as these are indicators of severity (
4,
14,
20). We characterized dual harmers’ mental health difficulties, experiences of adolescent victimization, and informant-reported personality functioning. Lastly, we evaluated their use of support services.
Methods
Participants
Participants were members of the Environmental Risk (E-Risk) Longitudinal Twin Study, a birth cohort of 2,232 British children drawn from a larger register of twins born in England and Wales in 1994 and 1995 (
21). Details of the E-Risk study have been reported elsewhere (
22). The E-Risk sample was constructed in 1999 and 2000, when 1,116 families (93% of those eligible) with same-sex 5-year-old twins participated in home-visit assessments. In this sample, 56% of twin pairs were monozygotic and 44% were dizygotic; sex was evenly distributed within zygosity (49% male). Families were recruited to represent the U.K. population with newborns in the 1990s on the basis of residential location throughout England and Wales, as well as mother’s age. Teenage mothers with twins were overselected to replace high-risk families selectively lost to the register through nonresponse. Older mothers who had twins via assisted reproduction were underselected to avoid an excess of well-educated older mothers. The study sample represented the full range of socioeconomic conditions in the United Kingdom, as reflected in families’ distribution on a neighborhood-level socioeconomic index (
23): 25.6% of E-Risk families live in “wealthy achiever” neighborhoods, compared with 25.3% nationwide; 5.3% live in “urban prosperity” neighborhoods, compared with 11.6%; 29.6% live in “comfortably off” neighborhoods, compared with 26.9%; 13.4% live in “moderate means” neighborhoods, compared with 13.9%; and 26.1% live in “hard-pressed” neighborhoods, compared with 20.7%. E-Risk underrepresents “urban prosperity” households because they are likely to be childless.
Follow-up home visits took place when study participants were ages 7 (98% participation), 10 (96%), 12 (96%), and 18 (93% participation). Home visits at ages 5–12 assessed twin participants and their mothers; only twins were assessed at age 18. There were no differences between those who took part at age 18 and those who did not on socioeconomic status, as assessed when the cohort was initially defined (χ2=0.86, p=0.65), IQ score at age 5 (t=0.98, p=0.33), or internalizing or externalizing behavior problems at age 5 (t=0.40, p=0.69, and t=0.41, p=0.68, respectively).
Each twin in a twin pair was assessed by a different interviewer. Data were supplemented by searches of official records and questionnaires that are mailed, as developmentally appropriate, to teachers and co-informants nominated by participants. The Joint South London and Maudsley and Institute of Psychiatry Research Ethics Committee approved each study phase. Parents gave informed consent and twins gave assent between ages 5 and 12 and informed consent at age 18.
Self-Harm
At age 18, participants were asked about self-harm behavior since age 12, using a life history calendar to aid recall. Ages 12–18, the years of secondary school in the United Kingdom, represent a meaningful developmental period for self-harm. Participants were asked, “Have you ever tried to hurt yourself, to cope with stress or emotional pain?” Individuals who endorsed self-harm were queried about methods. Ten behaviors were probed (e.g., cutting, burning, overdose), and participants were given the option of describing any other way they had hurt themselves. Of 2,064 participants who provided self-harm data, 280 (13.6%) reported self-harm behaviors. To assess self-harm frequency, we summed participants’ responses concerning the number of times they had performed each behavior (median reported number of self-harm incidents, 6.5).
Violent Crime
Official records of participants’ criminal offending were obtained through U.K. Police National Computer record searches conducted in cooperation with the Ministry of Justice. Records include complete histories of cautions and convictions beginning at age 10, the age of criminal responsibility. Our data are complete through age 22. Violent offending was coded as a binary variable to reflect whether participants had been cautioned or convicted for a violent offense. 2,060 twins consented to record searches of their offending histories, of whom 106 (5.2%) had a record of a violent offense (see Table S1 in the online supplement).
Violent offending was also assessed via a computer questionnaire at age 18, in which participants reported on past-year offending behaviors. Violent offenses were defined to include behaviors that involved the use of force or threat of force upon a victim (e.g., robbery, assault; see Table S2 in the online supplement). Of 2,053 respondents with self-report data, 677 (33.0%) endorsed one or more violent behaviors and 338 (16.5%) endorsed two or more.
Respondents were coded as positive for violent crime if they had an official record of a violent crime or self-reported two or more violent offenses. A total of 398 of 2,051 (19.4%) participants met these criteria (see the online supplement).
Typology of Self-Harm and Other Harm
We categorized participants into three groups for analyses: individuals coded as negative for both self-harm and violent crime (“neither harmers”; N=1,475 [72.0%]), those coded as positive for self-harm and negative for violent crime (“self-only harmers”; N=177 [8.6%]), and those coded as positive for both self-harm and violent crime (“dual harmers”; N=97 [4.7%]).
We aimed to identify which adolescents, among those who self-harm, are most likely to commit violent crime. Therefore, self-only harmers were the comparison group of interest. However, we also conducted comparisons with adolescents who only commit violent crime (“other-only harmers”; N=300 [14.6%]).
Childhood Risk Factors
We analyzed four prespecified and theory-driven childhood risk factors: low self-control, maltreatment by an adult, childhood self-harm behavior, and family history of psychiatric disorder (
1,
15,
19,
24) (see Table S3 in the
online supplement). We also collected information on caregiver- and teacher-reported self-regulation difficulties at age 12 (see Table S3). In response to suggestions from external reviewers, we analyzed three secondary childhood risk factors at age 12: low IQ, depression, and anxiety (see Table S3).
Correlates of Clinical Importance
We collected information on correlates of dual-harm behavior at age 18. We analyzed correlates in three categories with relevance for clinical practice: mental health difficulties (DSM-IV-based symptoms or diagnoses of posttraumatic stress disorder [PTSD], depression, psychosis, and substance dependence); experiences of adolescent victimization (crime victimization, maltreatment, neglect, sexual victimization, family violence, Internet/mobile-telephone victimization, and peer/sibling victimization); and informant-reported personality functioning (see Table S3).
Service Use
At age 18, participants were queried regarding past-year treatment for emotional problems. Participants were asked whether they had used a range of services, including mental health professionals, other supports (e.g., medical doctor, social services), and medication (see Table S3).
Statistical Analysis
We used logistic regression to test for an association between self-harm and violent crime. We included an interaction term to test whether the association differed by sex. We used conditional logistic regression to test whether twins from discordant pairs who self-harmed were at excess risk for violent crime relative to their co-twins who did not self-harm.
We used multinomial and binomial logistic regression to predict group membership from childhood risk factors. The binomial tests were of greatest interest, as we aimed to identify the antecedents that distinguished dual from self-only harmers.
We used chi-square tests to determine whether the dual and self-only harm groups differed in the proportion of individuals reporting a high frequency of self-harm (more than 50 incidents [75th percentile of the distribution]). We used regression to test whether dual harmers were distinguished by mental health difficulties, victimization experiences, and personality functioning and to compare dual and self-only harmers on service use. Groups were included as predictors, first as a set of binary dummy codes (with the neither-harm group specified as the reference category) and then as a two-level nominal variable (to compare risk between the dual harm and self-only harm groups). We analyzed continuously distributed outcomes using ordinary least squares and binary outcomes using logistic regression.
Analyses were conducted using SAS, version 9.4 (SAS Institute, Inc., Cary, N.C.). We used survey analysis procedures to correct all analyses (except the twin-discordance analysis) for the nonindependence of twin observations by clustering standard errors at the family level. Analyses in which male and female participants were combined were adjusted for sex. Analyses were limited to individuals with complete data for self-harm and violent crime (N=2,049); no data were imputed.
Results
Of the 2,232 participants in the original cohort, 2,066 (92.6%) were interviewed at age 18, of whom 2,049 (99.2%) had data for both self-harm and violent crime (970 of them male [47.3%]). Of the 2,049 participants included in analyses, 274 (13.4%) reported self-harm and 397 (19.4%) met criteria for violent crime.
Association of Self-Harm and Violent Crime in Adolescence
Self-harm was more prevalent among females than males (χ2=14.93, df=1, p<0.001), and violent crime was more prevalent among males than females (χ2=78.08, df=1, p<0.001), but the relation between self-harm and violent offending was similar in both sexes: the odds of committing violent crime were more than three times greater for adolescents who self-harmed than for those who did not (males: odds ratio=3.77, 95% CI=2.46–5.78; females: odds ratio=3.27, 95% CI=2.17–4.94) (see Figure S1 in the online supplement). Therefore, male and female participants were combined in analyses (but we controlled for sex; odds ratio=3.50, 95% CI=2.61–4.70). The association remained significant when only police records for violent crime were used (odds ratio=3.26, 95% CI=2.08–5.12) and when only self-reports were used (odds ratio=3.50, 95% CI=2.57–4.76), indicating that the findings do not simply reflect common method variance.
Effect of Familial Risk Factors on the Association Between Self-Harm and Violent Crime
Twins who self-harmed were more likely to commit violent crime than their co-twins who did not self-harm (dizygotic twins: odds ratio=2.57, 95% CI=1.07–6.16; monozygotic twins: odds ratio=4.00, 95% CI=1.34–11.97) (see Figure S2 in the online supplement), indicating that the relation between self-harm and violent offending could not be explained entirely by familial risk factors (genetics or rearing environment).
Childhood Risk Factors Distinguishing Dual from Self-Only Harmers
Analyses of primary risk factors showed that low childhood self-control and maltreatment predicted increased odds of being a dual versus a self-only harmer (self-control: odds ratio=1.82, 95% CI=1.35–2.45; maltreatment: odds ratio=2.46, 95% CI=1.10–5.51) (
Table 1). Together, the four primary risk factors predicted membership in the dual harm relative to the self-only harm group with high accuracy (area under the curve=0.75, 95% CI=0.69–0.82, indicating a large effect [
25] that requires out-of-sample replication; see the
online supplement).
Analyses of secondary risk factors indicated that higher childhood IQ predicted decreased odds of being a dual versus a self-only harmer (odds ratio=0.98, 95% CI=0.96–0.996) (
Table 1). Dual harmers did not differ from self-only harmers in rates of childhood depression or anxiety.
Dual Harmers’ Self-Regulation Difficulties Across Settings
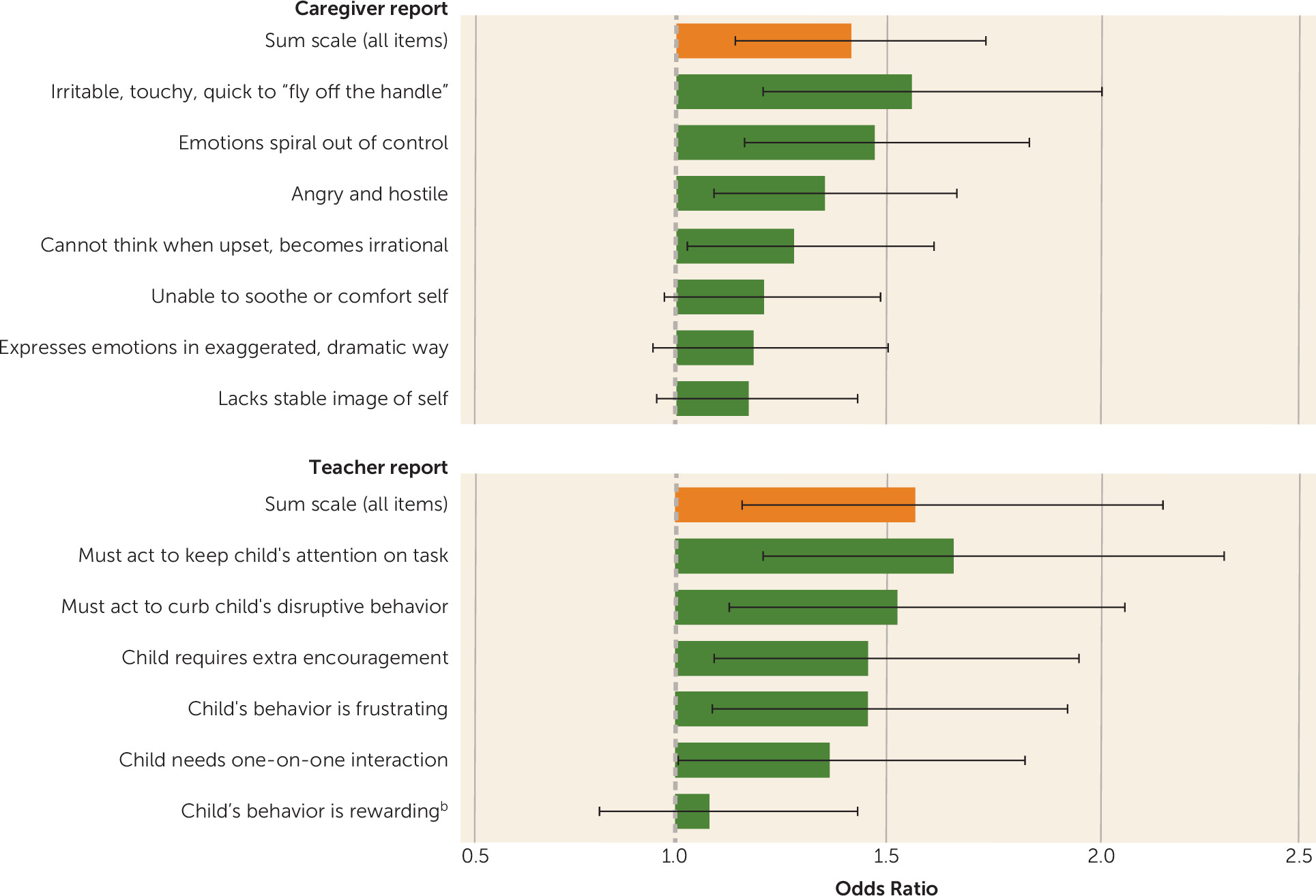
Dual harmers’ self-regulation difficulties were observable across settings. Children rated by caregivers and teachers as having more self-regulation difficulties were more likely to be in the dual harm than the self-only harm group as adolescents (caregivers’ scale score: odds ratio=1.41, 95% CI=1.14–1.74; teachers’ scale score: odds ratio=1.56, 95% CI=1.15–2.13) (
Figure 1).
Clinical Features and Life Characteristics Distinguishing Dual From Self-Only Harmers
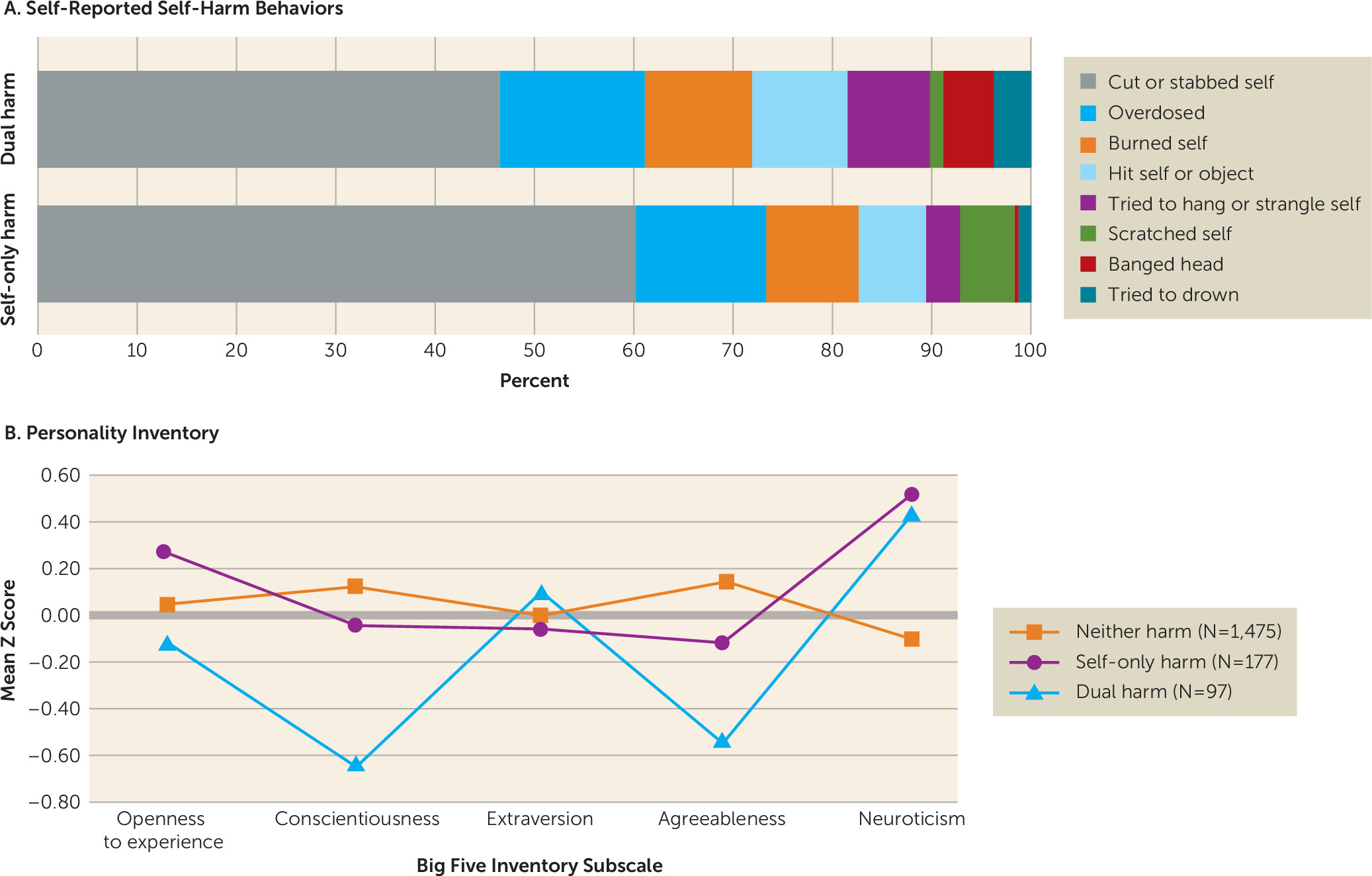
Dual and self-only harmers reported similar rates of high-frequency self-harm (more than 50 incidents; dual harm, 26.6%; self-only harm, 24.6%; χ2=0.13, df=1, p=0.72). Given the small sample sizes for some self-harm methods, we did not conduct tests of group differences for each method. However, inspection of
Figure 2A suggests that dual harmers exhibited higher-lethality behaviors (hanging, drowning) and aggressive acts (hitting oneself or an object, banging one’s head against a wall), while self-only harmers tended to engage in lower-lethality methods (cutting, scratching).
Dual harmers did not differ from self-only harmers in their risk of developing PTSD or depression. However, they were distinguished by a higher prevalence of psychotic symptoms (odds ratio=2.35, 95% CI=1.11–4.95). They were also more likely to meet criteria for alcohol dependence (odds ratio=3.29, 95% CI=1.65–6.57) and cannabis dependence (odds ratio=4.31, 95% CI=1.91–9.76) (
Table 2).
Dual harmers were more likely than self-only harmers to have experienced multiple types of victimization during adolescence (polyvictimization; odds ratio=2.40, 95% CI=1.30–4.42) (see Figure S3 in the
online supplement) as well as crime, maltreatment, neglect, and family violence (
Table 2).
Dual harmers’ personality styles were different from those of self-only harmers. Dual harmers were distinguished by greater resistance to change (lower openness; Cohen’s d=−0.41), poorer impulse control (lower conscientiousness; d=−0.63), and more aggressive/rude behavior (lower agreeableness; d=−0.46). They were more outgoing (higher in extraversion); however, the effect size was modest (d=0.15) (
Figure 2B; see also Table S4 in the
online supplement). Both dual and self-only harmers were more easily distressed (higher in neuroticism) and were lower in conscientiousness and agreeableness than neither harmers.
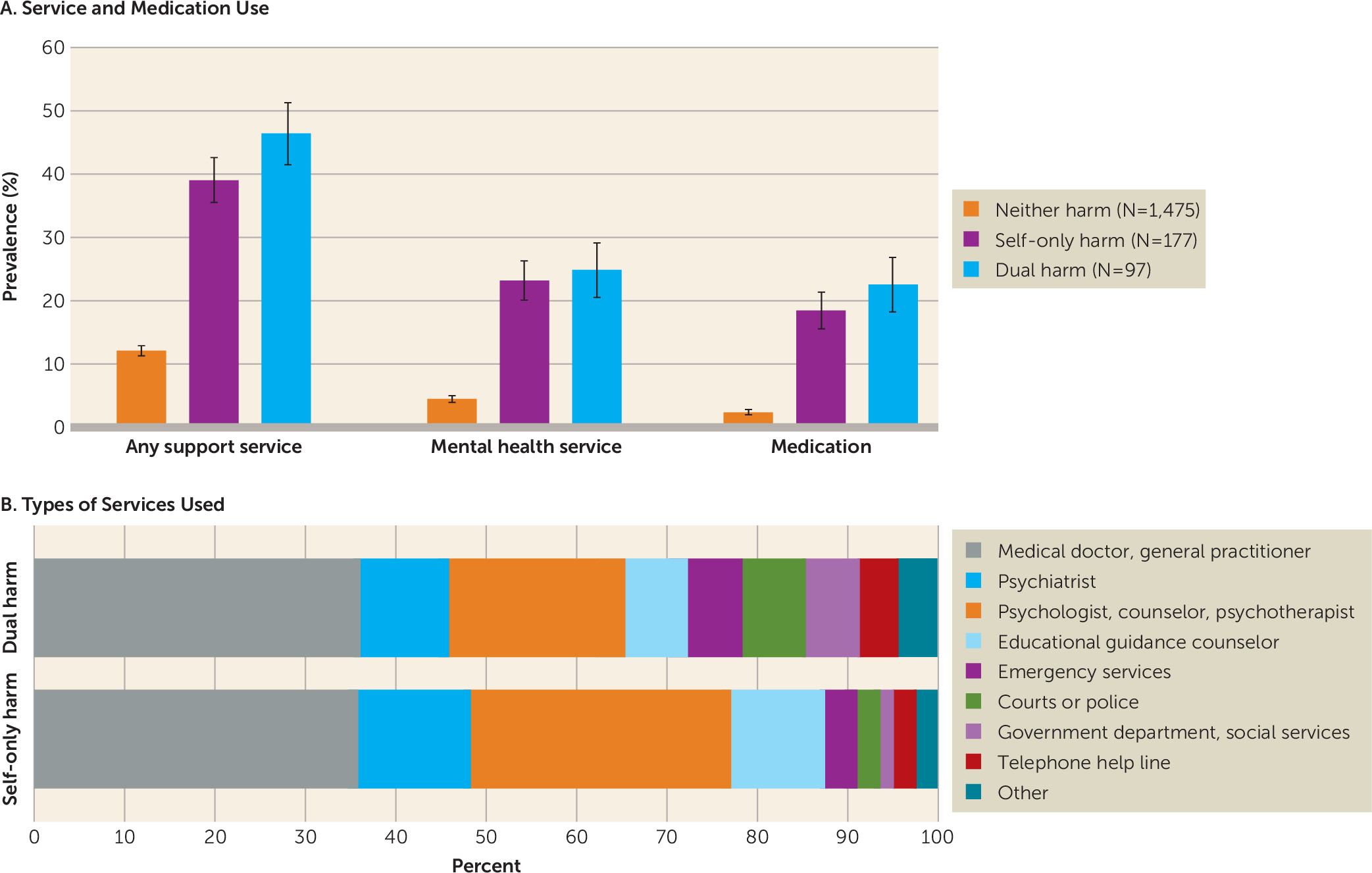
Despite their elevated rates of psychiatric comorbidity and difficult life experiences, dual harmers were not more likely than self-only harmers to be in contact with mental health professionals (psychiatrists, psychologists, counselors, or psychotherapists) or other support services (
Figure 3).
Comparisons With Other-Only Harmers
Compared with participants who committed violent crime only, dual harmers exhibited higher rates of childhood self-harm and childhood depression, had higher rates of all adolescent mental health difficulties, were more likely to have experienced polyvictimization and nearly all types of victimization, and were lower in conscientiousness and higher in neuroticism (see Tables S5–S7 in the online supplement).
Discussion
This study shows that self-harm and violent crime co-occur in a longitudinal population-representative contemporary cohort of British twins. The association is evident in police records and self-reports of offending. This finding is consistent with research employing population-based samples from other countries (
7–
10).
This study advances knowledge in five ways. First, using a co-twin-control design, we showed that the relation between self-harm and violent crime is not solely attributable to shared genetic risk or family background; self-harm itself may be an indicator of violence against others.
Second, we demonstrated that dual harmers are distinguished from self-only harmers by poor childhood self-control, including deficits in executive functioning, as indicated by lower childhood IQ. Prospective assessment enabled measurement of self-control, cognitive ability, and other antecedents prior to the onset of self-harm and criminal offending and ensured that there were no ascertainment or recall biases. Moreover, dual harmers’ self-regulation difficulties were reported by multiple informants, suggesting that this early-emerging risk factor is observable across settings. In addition to their experiences of childhood dysregulation, dual harmers were characterized in adolescence by a triad of personality features that typifies emotional and interpersonal lability: low conscientiousness, low agreeableness, and high neuroticism (
26). (Dual and self-only harmers did not differ on neuroticism, but this trait was elevated in both groups.) Apparently, dual harmers’ self-control difficulties are a stable core feature of their personalities.
Third, we showed that dual harmers are differentiated from self-only harmers by a history of childhood maltreatment. Furthermore, dual harmers were more likely to have been exposed to adolescent victimization. More than 80% of dual harmers had experienced at least one type of victimization, and one-third had experienced polyvictimization. These findings signal a need for primary and secondary preventive strategies to reduce continuity in victimization among individuals at risk for dual-harm behavior.
Fourth, we found that dual harmers are distinguished from self-only harmers by higher rates of psychotic symptoms, alcohol dependence, and cannabis dependence. A previous analysis (
7) did not find differences in risk for cannabis-related problems between dual and self-only harmers. However, that study employed a retrospective survey of adults and DSM-5-based lifetime diagnoses. Ours is the first study, to our knowledge, to test these associations within a prospective sample and to demonstrate the role of psychosis in the self/other harm typology. Dual harmers suffer significant psychiatric comorbidity; comprehensive diagnostic assessment is needed to appropriately target interventions within this population.
Lastly, we found that dual harmers were not more likely than self-only harmers to encounter mental health services. Recent U.K.-based data (
3,
27) suggest long waiting lists and high thresholds in accessing treatment, and similar challenges exist in the United States (
28). Research on hospital- and community-based youth violence prevention services identifies mistrust of authorities as a barrier to treatment engagement (
29). Dual harmers’ psychosocial difficulties and prior experiences with the juvenile justice system may impede service use.
This study has limitations. First, the sample comprised twins, and the results may not generalize to singletons. However, the prevalences of antisocial behavior and mental health problems are similar for twins and singletons (
30,
31), and the association between self-harm and violent crime has been documented in non-twin samples (
7–
10). Second, participants were followed only to the beginning of young adulthood. Future research will determine whether the findings pertain to older age groups. Third, results may vary with historical and cross-national differences in crime-control policy. Fourth, findings concerning risk factors require replication. However, primary antecedents were selected on the basis of prior theoretical and empirical evidence, increasing the likelihood of replication. Fifth, our co-twin-control analyses included a rather small number of “informative cases” (pairs discordant for violent offending). The results will need to be replicated in samples with a higher prevalence of discordant pairs. Sixth, we designed our assessments of self-harm and violent offending consistent with recommendations for best practice. However, differences in the types of assessment methods used across constructs may have affected our results. Finally, we are limited in our ability to infer causality. Assessment of self-harm and crime spanned much of the same period. Furthermore, within-twin-pair associations between self-harm and violent offending may be confounded by twin-specific environmental differences. Additionally, our research can only support low childhood self-control, low IQ, and maltreatment as indicators of risk for dual-harm behavior, not necessarily indicators of causation. Establishing whether associations are causal, however, is secondary to this study’s primary aim of informing mental health treatment.
This study has a number of implications. First, given the robust link between self-harm and harm toward others, research on self-harm—even when conducted in community samples, not only in clinical or forensic settings—should collect data on interpersonal violence. Second, theoretical models of self-harm can generate testable hypotheses for research on dual-harm behavior. Many theories propose that self-harm serves an emotion-regulatory function (
14,
17). Recently developed models hold that several proximal risk factors lower perceived barriers to initiating self-harm; however, the affective benefits of self-harm are its primary maintaining factor (
32,
33). These benefits may lower barriers to engagement in other harmful behaviors, including violent crime. Although our study did not directly test this question, our findings support further investigation of self-regulation as a mediating factor. The interpersonal theory of suicide (
34) posits that self-harm increases risk for suicide by habituating individuals to the fear and pain associated with harming oneself. Such habituation may also increase risk for harming others, or it may occur through repeated aggression toward others. Research on the mechanisms underlying dual harm presents opportunities for interdisciplinary collaboration. Self-harm and offending have largely been studied separately within the fields of psychology, psychiatry, and criminology; collaborative cross-talk can inform more effective preventions and treatments.
Third, clinical guidelines recommend evaluation of risk for suicide following self-harm (
35,
36). Our results support a recommendation of assessment of risk for violence toward others as well, particularly when the clinical picture comprises relevant antecedents and correlates. Furthermore, dual-harming prisoners should be closely monitored for suicidal behavior. Fourth, improving self-control among self-harmers could help prevent violent crime. Self-control training has been shown to reduce delinquency (
37) and could be delivered to patients who self-harm. In addition, dual harmers often experience psychiatric comorbidity. Transdiagnostic approaches that target self-regulation (e.g., mindfulness-based approaches for emotion regulation) may reduce harmful behaviors and co-occurring psychopathology (
38). Lastly, our findings support recommending the application of available interventions to prevent childhood maltreatment (
39) as well as implementation of exposure-reduction strategies (e.g., education on self-protective measures) and evidence-based programs (
40,
41) to prevent revictimization in adolescence. Dual harmers have been immersed in violence from a young age; a treatment-oriented rather than a punishment-oriented approach is indicated to meet these individuals’ needs. Such an approach could also yield substantial reductions in violent offending: one in four other-harming adolescents was a dual harmer in this population-representative study.
There is a pressing demand for improvements in adolescent mental health services (
42) and psychological treatment research (
43,
44). Our analysis responds to this demand by identifying several opportunities for early-years prevention and intervention science (
43,
44). Connecting vulnerable adolescents with delinquency-reduction programs that target self-control, prevention of maltreatment and victimization, and improvement in children’s self-regulation abilities could significantly reduce the health and social burdens attributable to internalized and externalized violence.