Most general population risk for schizophrenia is accounted for by common variations in the genome, but each variant explains only a tiny fraction of increased risk. In contrast, approximately 1%−2% of individuals with the diagnosis of schizophrenia have a microstructural chromosomal abnormality resulting in either a deletion or duplication of a segment of the genome, typically involving more than 100,000 nucleotides and many genes. These so-called copy number variations (CNVs) typically arise during meiosis and are found on one parental chromosome. They tend to be much more clinically penetrant than common variants, presumably because they involve a dosage alteration of genes within the CNV region, although they account for much less population risk. Close to a dozen CNVs have been associated with the diagnosis of schizophrenia, and as with common variants, they span the genome and do not converge on a simple common biology. Although the more penetrant schizophrenia associated CNVs are of potential value in genetic counseling, and some involve a high probability of intellectual compromise, none are more likely to result in the diagnosis of schizophrenia than not.
Because common risk-associated variants have little or no value in genetic counseling and limited application in clinical research, a so-called polygenic risk score (PRS) has been developed as a tool for assigning to an individual a measure of his or her overall genomic risk for illness, and PRSs tend to account for severalfold increases in individual liability. Indeed, PRSs near the upper end of the distribution of scores carry risk odds ratios similar to most of the risk-associated CNVs. The PRS is calculated as a weighted sum of risk-associated alleles found in the latest genome-wide association study (GWAS) of a particular trait or diagnosis. Because it is a value given to an individual, it can be used as a predictor variable in clinical studies. Three articles in this issue of the Journal illustrate some applications of the schizophrenia PRS in clinical research, including in the context of risk-associated CNVs.
The article by Bergen and colleagues (
1) addresses the question of whether genomic risks based on single-nucleotide polymorphism (SNP) associations (i.e., the PRS) and CNVs are orthogonal risk trajectories in affected individuals or whether PRS biases CNV carriers to express psychotic features. Rare variants appear to be more penetrant as schizophrenia risk factors than GWAS-associated SNPs, but most carriers of the identified rare variants do not develop schizophrenia. Intellectual disability is the most likely phenotypic association. In a subsample of more than 40,000 participants from the Psychiatric Genomics Consortium data set with available CNV results, Bergen and colleagues evaluated the relationship of PRS and the presence of CNVs previously implicated as risk factors for schizophrenia. In general, they found that carriers of CNVs had lower PRS compared with noncarriers, but this difference was only significant in the context of the most penetrant CNVs. These results thus fit the model of both interacting and divergent risk trajectories, since PRS contributes to risk for the diagnosis of schizophrenia in CNVs with relatively low penetrance but less so, if at all, in CNVs that are more penetrant (e.g., the 22q11 hemideletion associated with the velocardiofacial syndrome). These results and earlier studies with similar findings raise interesting epistemological questions about whether individuals with CNVs and those without actually have different syndromes.
The article by Zhang and colleagues (
2) explores whether PRS could inform about clinical response to antipsychotic drug treatment in patients with first-episode psychosis. Using treatment response data over 12 weeks in four clinical samples, two from the United States and two from Europe, the authors found that PRS calculated from SNPs with p values <0.01, in the European ancestry sample GWAS described above, predicted residual symptoms in three of the four cohorts at 12 weeks, meaning that the higher the score, the poorer the apparent response to treatment. In a meta-analysis of all four groups, a significant relationship was found, but less than 4% of the variance in treatment response could be determined from this PRS relationship. These results echo several earlier studies suggesting that relatively higher schizophrenia PRSs tend to predict a relatively poorer response. The study by Zhang and colleagues raises many questions, including whether this correlation might reveal more meaningful predictions with specific subgroups of study subjects if the authors had not controlled for certain covariates. For example, would the results be stronger among males or among case subjects with an earlier age at onset? It also is of interest that apparently better prediction is found in the non-European samples in this study, even though current schizophrenia PRSs show much poorer prediction of phenotypic risk in non-European samples. Efforts to evaluate the clinical utility of PRS in predicting treatment response will likely be empowered by deeper and more granular approaches to patient characterization.
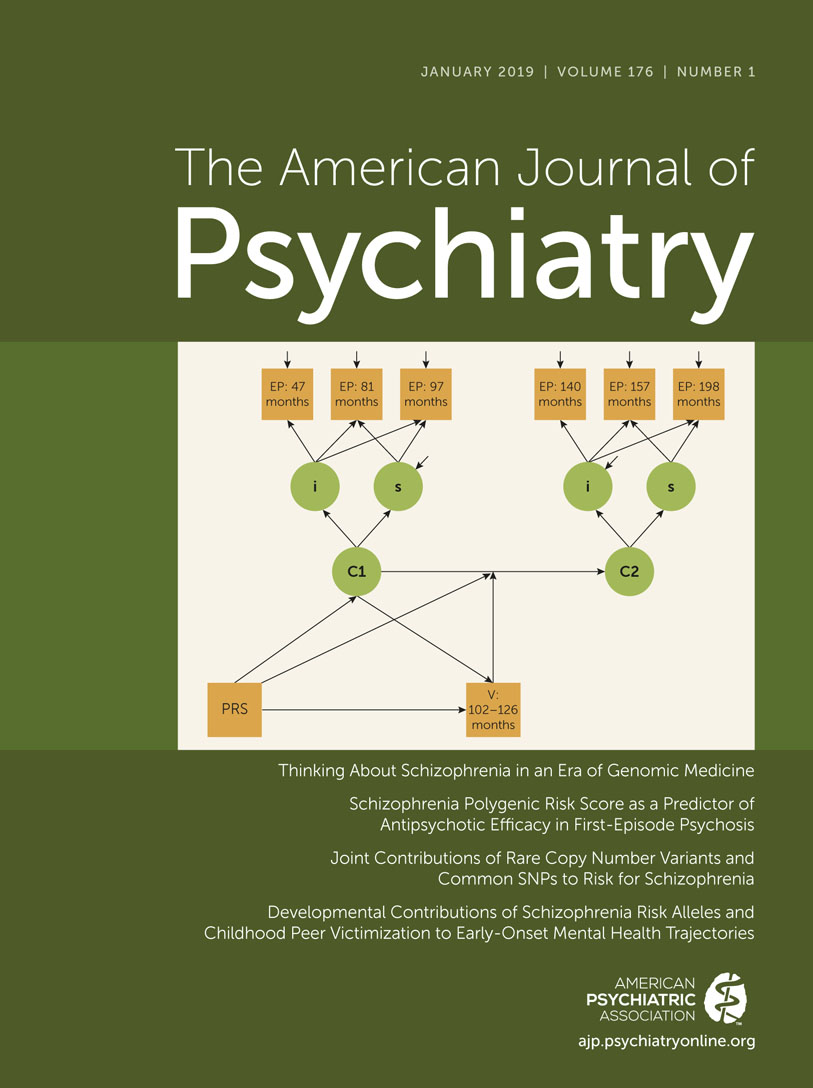
The article by Riglin and colleagues (
3) asks whether PRS can predict anxiety-related characteristics during early childhood and adolescence, their stability within and across these age periods, and whether PRS interacts with social stress in the form of bullying and related aspects of peer victimization in late childhood. The study population of more than 7,000 participants from England is one of several longitudinal birth cohort data sets from studies of child health and development around the world. The authors confirm earlier observations that schizophrenia PRS predicts aspects of emotional and cognitive function relatively early in life. Their longitudinal design allowed them to explore changing trajectories of ratings for anxiety during the age periods studied, and they found that approximately 9% of participants had a trajectory of increasing emotional distress during childhood that predicted increasing emotional distress during adolescence. PRS was significantly associated with the increasing emotional distress trajectory during childhood, although the association was weak (odds ratio, 1.1). PRS did not account for the adolescent trajectories, which seemed to be based on the childhood emotional trajectory, and there was no clear interaction between PRS and peer victimization, which did, however, significantly affect adolescent emotional trajectories. These results fit other models suggesting that schizophrenia genomic risk influences the establishment of an early developmental trajectory related to higher-order brain functions that read out in terms of cognition and emotional reactivity. This study also underscores both the potential complementarity and, to some degree, orthogonality of genetic and environmental risk factors for adolescent emotional distress.