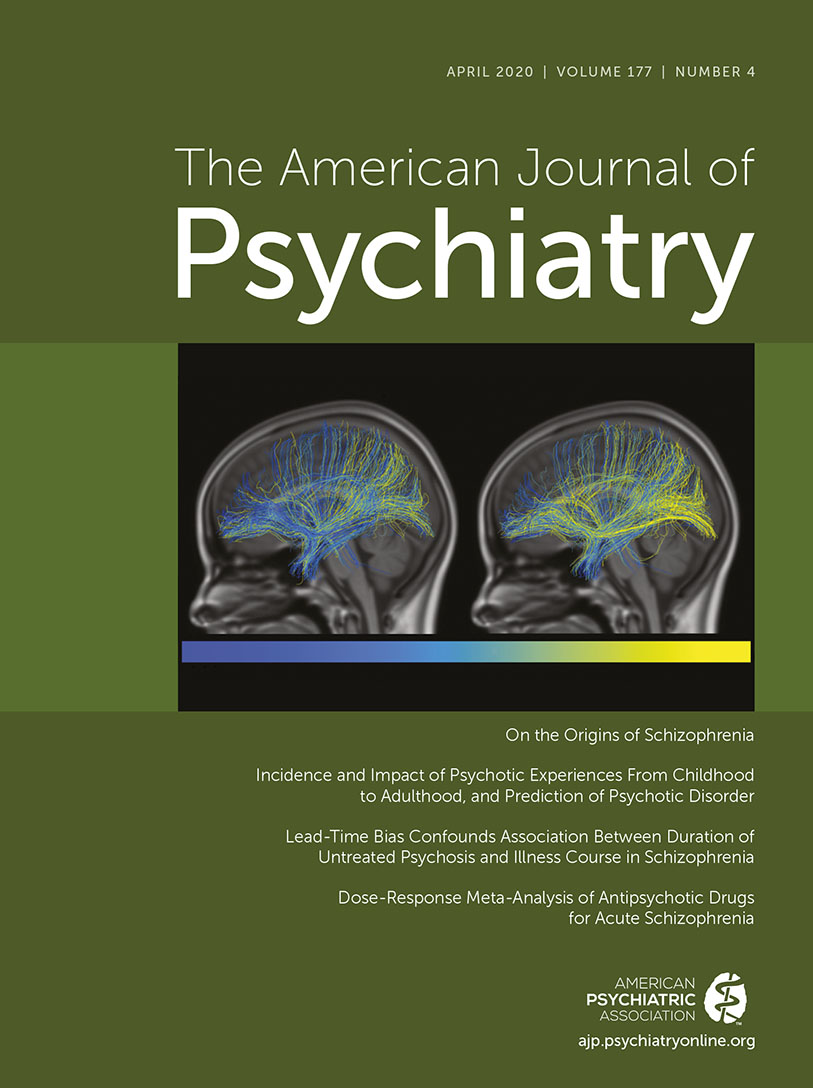
Schizophrenia has been conceptualized as a disorder of brain connectivity since the illness was first defined (
9,
10,
44), and this idea was revived a century later using more modern techniques (
45). Consistent with these hypotheses, we have shown that white matter connectivity is disrupted in schizophrenia, particularly in those areas that form the hubs for the main connections in the brain (
46,
47). In view of their rich interconnectedness, these hubs are sometimes collectively called the “rich club” (
46). These networks, also called the “connectome” of the brain (
48), are under genetic control (
43,
49) and are already being formed in the second trimester of pregnancy (
50). The efficiency of this network—defined as the optimal relationship between functional connectivity and distance between brain areas (
51)—is highly related to intelligence (
52), as are the observed changes in this network’s efficiency during adolescence (
49). Not only are brain networks under considerable genetic control, and not only are the abnormalities related to some of the genes conferring increased risk for schizophrenia, but also important changes in these networks crucially occur during early adolescence. In general, the cortex becomes thinner during adolescence (e.g.,
53), with its connecting white matter fibers increasing in volume (
54). The cortical changes are genetically controlled and are related to cognitive development during adolescence (
55). Crucially, the brain networks become increasingly more efficiently organized during this period (
49), with their efficiency increasing in adolescence between ages 10 and 13 (
56) and the effect leveling off between ages 13 and 18. The connectome’s efficiency itself and the relationship between intelligence and network efficiency are under genetic control (47% and 87%, respectively) (
54). Thus, abnormal development of the brain’s network appears to be a plausible candidate for the neuroanatomical and functional substrate of the cognitive changes that precede the onset of psychosis in schizophrenia. Moreover, in view of the high heritability, abnormalities in the networks’ efficiency could possibly be related to the genetic risk of schizophrenia. Indeed, abnormal network efficiency in the rich club has been found in siblings (
57) and offspring of schizophrenia patients (
58). Interestingly, this effect in the rich club hubs appears to be specific for schizophrenia—it has not been found in patients with bipolar disorder (
59) or their offspring (
58). Since the abnormalities are also observed in medication-naive schizophrenia patients, they cannot be attributed to the use of medication and are most likely present before illness onset (
60). Moreover, connectome organization has been found to be related to functional outcome and decreases in IQ over time in schizophrenia patients (
61). Importantly, the macroscopic hub areas of the brain, as identified with MRI, can also be determined on a cellular, microscopic level, and they are highly related to higher-order cognitive functions, such as IQ (
62,
63). Moreover, when combining transcriptional profiles of schizophrenia risk genes with data on the decreased hub connectivity, we found that the expression profile of risk genes across cortical regions was significantly correlated with the regional dysconnectivity (
64). In addition, effects were found to be potentially specific to schizophrenia, with transcriptional profiles not related to cortical dysconnectivity in patients with bipolar illness. Especially fascinating is the finding that brain connections present in humans but not in chimpanzees—those predominantly involved in semantic comprehension and language processing—are those affected in schizophrenia and not in other psychiatric disorders, such as autism, obsessive-compulsive disorder, and major depression (
65), suggesting that the same areas that have evolved in humans to acquire higher-order cognitive capabilities, such as language, are those that are particularly vulnerable to being affected in the development of schizophrenia. Another line of evidence suggesting that brain development during adolescence is a crucial factor in the path to schizophrenia is derived from genetic studies.