T
o the E
ditor: We appreciated the opportunity to read the thoughtful correspondence from Dr. Iyer and colleagues. They identified a number of factors that could have influenced our finding that the association between duration of untreated psychosis (DUP) and long-term outcome is explained by lead-time bias (
1). We agree with two of the points put forward by Dr. Iyer and colleagues, and we analytically evaluate the effects of potential confounding variables mentioned in their letter.
First, as stated in our publication, the results of our analyses should not be interpreted as evidence that early intervention is ineffective or unnecessary. We wholeheartedly agree with Dr. Iyer and colleagues that early comprehensive intervention can provide meaningful symptom relief and short-term psychosocial benefits and is therefore tremendously valuable to patients, families, and society.
Second, we agree with Dr. Iyer and colleagues that the care received by the Suffolk County Mental Health Project cohort is not comparable to that delivered in early intervention clinical trials. Previous publications have shown that this cohort received inconsistent, primarily pharmacological care (
2,
3). Indeed, Mojtabai’s review (
3) of the Suffolk County and other clinical epidemiological cohorts concluded that only a minority of individuals with schizophrenia receive adequate evidence-based care. Comprehensive treatments, such as those delivered in coordinated specialty care programs, may have durable effects on illness course in schizophrenia. NAVIGATE (
4), OnTrackNY (
https://www.ontrackny.org), and a number of other early intervention programs show promise for greater efficacy. However, this cohort’s treatment is likely reflective of that received by patients in the general population, and our analyses show that such treatment was insufficient to halt psychosocial decline.
Although the Suffolk County cohort differs from clinical trial cohorts in many ways, we have no reason to believe that our findings are not generalizable. In two epidemiological cohorts from Scotland and Israel, both contemporary to the founding of the Suffolk County cohort, more than 90% of individuals with schizophrenia were eventually hospitalized (
5,
6). Furthermore, despite significant declines in the availability of inpatient psychiatric beds in the years since the Suffolk County cohort was recruited, more than 75% of individuals in the Recovery After an Initial Schizophrenia Episode (RAISE) project were hospitalized prior to study entrance. Given these high rates, it is unlikely that our results were significantly affected by ascertainment of subjects during their first admission. Furthermore, the mean DUP in the Suffolk County sample (103 weeks) is within the range reported in a meta-analysis of epidemiological cohorts (10.4–213.2 weeks) (
7), suggesting that this cohort is representative of the range of DUPs observed in the general population.
In contrast, clinical trial cohorts in mental health research generally have fewer comorbidities and less severe illnesses, and they are younger, have better functioning, and are of higher socioeconomic status than epidemiological cohorts (
8). A comprehensive review of longitudinal studies of first-episode psychosis found that outcomes are substantially worse in representative samples (
9). Importantly, the trajectory of participants in the Suffolk County project closely parallels that of population-representative studies, as reported in Menezes et al. (
9). Therefore, although it is true that the Suffolk County cohort differs from clinical trial cohorts, it may reflect the modal course of schizophrenia for patients in the United States, most of whom will not be enrolled in clinical trials.
Dr. Iyer and colleagues cited evidence that the 90 days following first symptom onset may be a critical period during which intervention is effective in altering illness course.
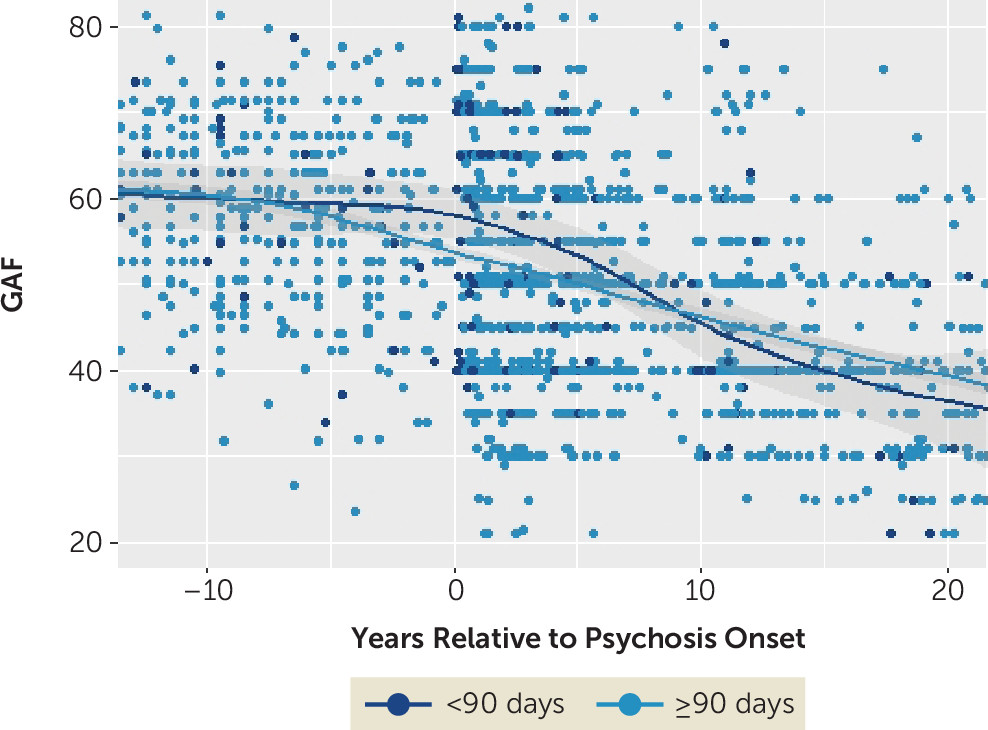
Figure 1 depicts a LOESS plot of trajectories as measured by the Global Assessment of Functioning Scale (GAF) as a function of DUP dichotomized at 90 days. The pattern of overlap between these groups is consistent with lead-time bias.
Finally, it was suggested that attrition over time was a function of psychosocial function (as measured by the GAF) and that attrition may have biased the trajectories of psychosocial function. However, attrition in the present study was low. Excluding data missing because of mortality, only 10% of data points were missing. Furthermore, we estimated a pattern mixture model, the best statistical correction available for correcting nonignorable missing data (
10), on GAF measures from baseline to the 20-year follow-up. After this correction, we found that the 20-year outcome worsened by less than 3 points on the GAF scale. The effect of DUP remained nonsignificant.
In sum, these analyses do not alter our findings that the association between DUP and long-term outcomes in schizophrenia is explained by lead-time bias. This does not mean that more robust treatments, such as those provided in early intervention clinical trials, cannot have lasting effects. However, determining whether this is true requires long-term follow-up of clinical trial cohorts and adjustment for lead time. Ultimately, even if the effect of early intervention is short-lived, we emphatically agree with Dr. Iyer and colleagues that these programs reduce suffering and are therefore valuable.