Clozapine Intoxication in COVID-19
| Year or Day | Clinical | O2 Sat. | Respiratory Rate (min) | Temperature (°C) | CRP (mg/L) | WBC (×109 cells/L) | Neutrophils (×109 cells/L) | Clozapine dosage (mg/day)a | Clozapine level (ng/mL)b | Norclozapine level (ng/mL)b | C/Dc | C/Nd | Treatment Strategy |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Past history (through April 2020) | |||||||||||||
| 2013 | Bronchitis | 36 | 300 | 210 | ? | 0.7 | ? | ||||||
| 2018 | Pneumonia | 37 | 22 | 500 | 1,183 | 490 | 2.4 | 2.4 | |||||
| 2019 | Bronchitis | 37 | 240 | 264 | 170 | 1.1 | 1.5 | ||||||
| 2019 | Pneumonia | 38.1 | 47 | 450 | 817 | 350 | 1.8 | 2.3 | |||||
| 2020 | Upper respiratory tract infection | 37.6 | 39 | 400 | 661 | 380 | 1.7 | 1.7 | |||||
| Current case (April 2020) | |||||||||||||
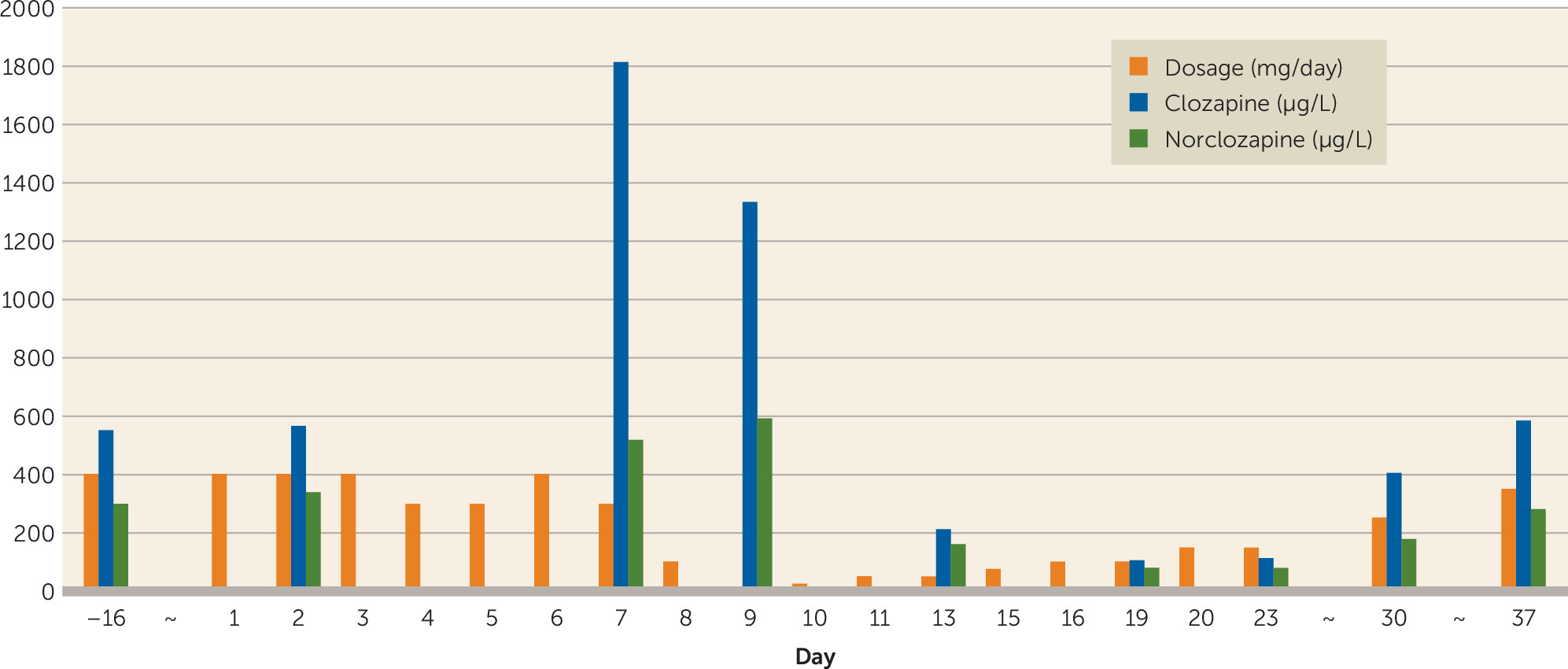
| Baselinee | 9 | 6.4 | 400 | 553 | 300 | 1.4 | 1.8 | ||||||
| 1 | Sonorous wheezes audible without stethoscope. Nasopharyngeal swab, PCR SARS-coronavirus-2 RNA: positive | 95%–96% | 14 | 36.9 | 400 | Home quarantine | |||||||
| 2 | Sedimentation rate, 2 mm/hour | 37.0–37.5 | 9 | 5.3 | 4.2 | 400 | 565 | 340 | 1.4 | 1.7 | |||
| 4 | Tremors in arms and legs, unsteady on feet, sweating, pale face, blue lips | 38.4 | 300 | Halve clozapine dosage per dose at temperatures ≥38°C. Start oxygen 1 liter/minute, start paracetamol 1,000 mg t.i.d. | |||||||||
| 5 | Clinical deterioration, loss of initiative, echolalia | 24 | 38.7 | 13 | 300 | Increase oxygen to 2 liters/minute | |||||||
| 6 | Clinical deterioration, increased fatigue | 93% | 24 | 37.1–38.1 | 400 | Increase oxygen to 3 liters/minute | |||||||
| 7 | Lungs: vesicular breath sounds, dubious basal right crackles. Gross tremors in arms and hands. Clinical deterioration. Working diagnosis: bacterial pneumonia in addition to COVID-19 | 90%–96% | 39.4 | Unknown (test failed) | 6 | 5.2 | 300 | 1,814 | 520 | 5.0 | 3.5 | Increase oxygen to 4 liters/minute. Start amoxicillin/clavulanic acid 500/125 mg t.i.d. for 7 days | |
| 8 | Clinical deterioration, increased fatigue | 98% | 20 | 100 | |||||||||
| 9 | Clinical improvement: more active | 95% | 20 | 38.4 | 2.1 | 1.3 | 0 | 1,335 | 590 | 2.2 | Reduce oxygen to 3 liters/minute | ||
| 10 | Clinical improvement | 95%–98% | 37.6–38.0 | 25 | |||||||||
| 11 | Clinical improvement | 93%–99% | 16 | 36.7–38.1 | 50 | ||||||||
| 12 | Clinical deterioration: fatigue, reduced alertness | 95%–97% | 20 | 37.3 | 50 | ||||||||
| 13 | Clinical deterioration: fatigue, dyspnea, drowsy | 88%–99% | 14 | 35.2 | 3.1 | 1.8 | 50 | 213 | 160 | 1.3 | |||
| 14 | Clinical improvement, but tired | 18 | 37.8 | 50 | Reduce oxygen to 2 liters/minute | ||||||||
| 15 | Clinical improvement | 97% | 16 | 36.3 | 75 | ||||||||
| 16 | Clinical improvement | 98% | 14 | 36.9 | 100 | Reduce oxygen to 1 liter/minute | |||||||
| 17, 18 | Clinical improvement | 100 | |||||||||||
| 19 | Clinical improvement | 95%–98% | 18 | 36.3 | 10 | 7.5 | 100 | 107 | 80 | 1.4 | 1.3 | No extra oxygen | |
| 20 | Clinical improvement | 99% | 36.1 | 150 | Stop extra oxygen. Continue home quarantine in accordance with guidelines. Clozapine titration schedule to usual dose of 400 mg/day, in accordance with Clozapine Plus Werkgroep guideline | ||||||||
| 23 | Clinical improvement | 6.8 | 4.2 | 150 | 112 | 80 | 1.1 | 1.4 | |||||
| 30 | Clinically recovered | 7.4 | 5.2 | 250 | 406 | 180 | 1.6 | 2.7 | |||||
| 37 | Clinically recovered | 6.7 | 4.3 | 350 | 583 | 280 | 1.7 | 2.0 | |||||
References
Information & Authors
Information
Published In
History
Keywords
Authors
Funding Information
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBLogin options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).