Although current treatments are effective for many of our patients, numerous individuals fail to achieve complete remission, only partially respond to treatment, or discontinue treatment because of intolerable side effects. There is no doubt that we are more successful in treating some illness as compared with others. For example, we generally do well with patients suffering from depression but not as well, especially over the long term, with those struggling with schizophrenia. Most of our treatments result in demonstrable symptom reduction; however, when treatment is discontinued, relapse rates tend to be high. Fortunately, exciting recent advances from clinical and translational research hold promise for the development of new and more effective treatments.
A review of the data from some of the larger efficacy studies that focused on the treatment of depression and schizophrenia reminds us of where we were in the early 2000s in relation to today. The large Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study, completed in 2006 (
1), is a good example. This study revealed that only one-third of patients with depression reached remission after their first adequate trial of a selective serotonin reuptake inhibitor (SSRI), and in this study of “real-world” depression, it took four sequential treatments, including cognitive-behavioral therapy, to achieve remission in 67% of the patients (
2). Another large-scale study, from which the results were reported in 2005, was aimed at understanding the efficacy of antipsychotics for schizophrenia treatment. In the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) study (
3), by the end of 18 months, 74% of the patients had discontinued treatment because of side effects or lack of efficacy. While positive symptoms are the most responsive to antipsychotic treatment—and clozapine appears to be the most effective treatment for these symptoms—negative symptoms are particularly difficult to treat, and it is difficult to achieve a prolonged state of full remission. In our everyday practices, we still use SSRIs and atypical neuroleptics as our mainstays of treatment, and we continue to face considerable challenges in helping our patients with treatment-resistant illness. However, it is important to underscore that research over the last 10–15 years has led to the emergence of innovative treatment strategies targeting novel underlying mechanisms. While some of the new treatments are still under development, some have received approval from the U.S. Food and Drug Administration (FDA) and are currently in clinical use.
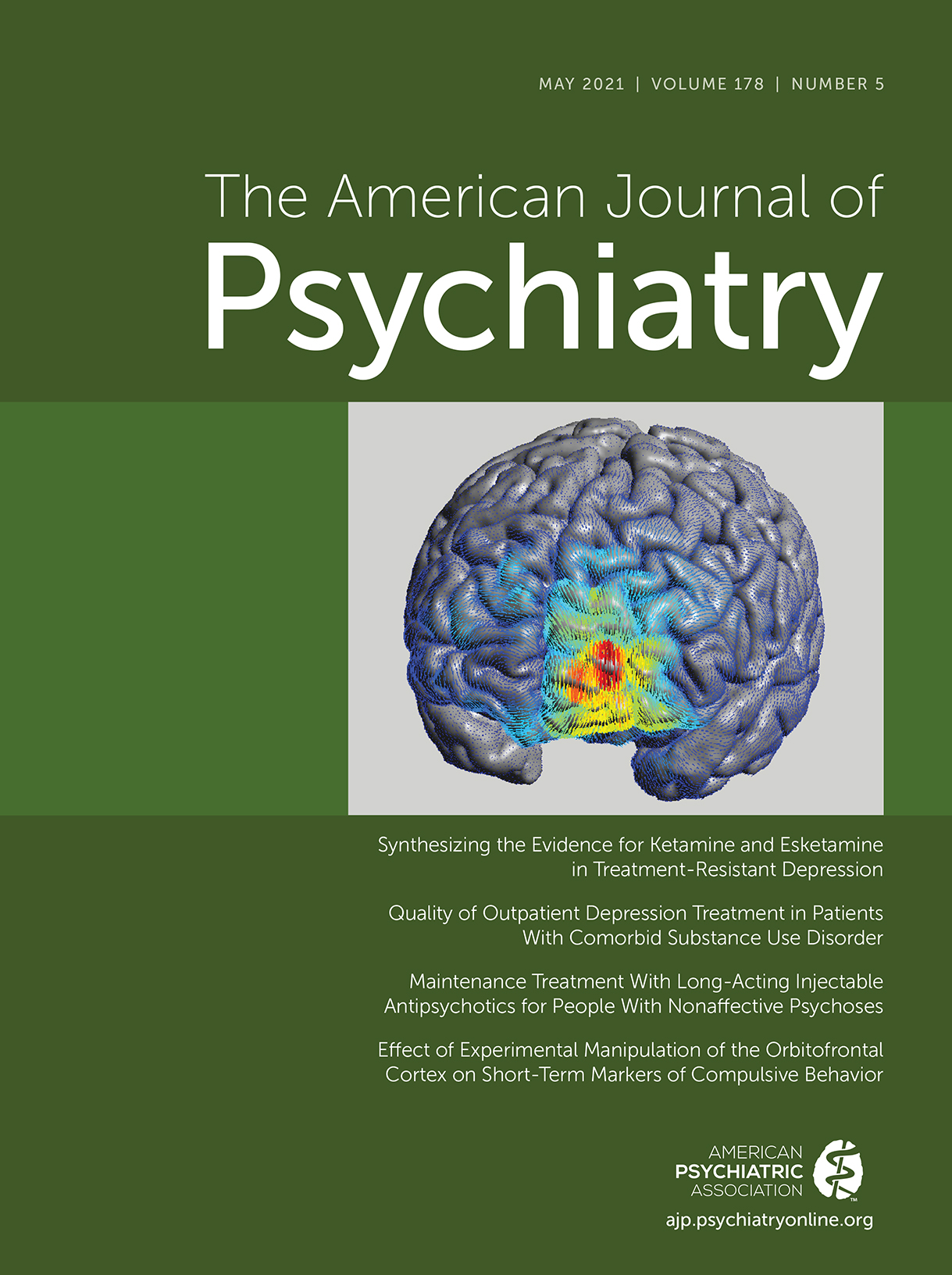
These recent advances have provided additional treatment tools for providers and new hope for our patients. This is especially the case for the treatment of major depression, where considerable progress is occurring. For example, modifications of transcranial magnetic stimulation (TMS) using a method called theta burst appears to hold much potential. Building on more traditional repetitive TMS, intermittent theta burst TMS (iTBS) is a method approved by the FDA that uses magnetic energy to modulate brain activity in ways that are thought to mimic rhythms associated with hippocampal electrical activity. A recent study noted rapid and improved response rates in patients with treatment-resistant depression when modifying the iTBS treatment protocol with more intensive administration over a shorter period of time and by using functional MRI (fMRI) to guide the iTBS targeting (
4). Intravenous ketamine and the FDA-approved intranasal esketamine have been important advances for rapid symptom reduction in some patients with severe depression and suicidal ideation (
5). Ketamine is thought in part to work via antagonism of the
N-methyl-
d-aspartate receptor with downstream effects mediated by AMPA receptors (
6). Other evidence suggests that opiate mechanisms may be partly involved in ketamine’s efficacy (
7). In relation to postpartum depression, efficacy has been established for the neurosteroid progesterone metabolite known as allopregnanolone or brexanolone (
8). Allopregnanolone, which must be administered with an intravenous infusion over 60 hours, modulates the function of GABA
A brain receptors, which is hypothesized to underlie its mechanism of action (
9). Follow-up oral drugs based on these effects are under development. Intriguing work with the use of psychedelics as a therapeutic strategy is ongoing, with clinical trials examining the efficacy of psilocybin for depression and
3,4-methylenedioxymethamphetamine (MDMA) for posttraumatic stress disorder (
10). These drugs are thought to, in part, mediate their potent effects by modulating the serotonin system. It is also important to note that considerable work is being performed to develop personalized medicine strategies. The goal of personalized medicine is to use valid biomarkers (e.g., neuroimaging measures such as EEG or genetic variation) along with machine learning tools to predict treatment efficacy in subsets of patients within or across disorders. An illustrative example is the demonstration that certain patterns of resting-state functional connectivity, as measured with fMRI, can predict which depressed individuals are more likely to respond to TMS (
11).
The examples mentioned above represent some of the exciting new opportunities for therapeutics in the treatment of depression. However, it is important to recognize that additional studies need to address many unanswered questions and issues related to some of the new treatments noted above. These include optimal dosing strategies, the maintenance of acute efficacy over the long term, concerns related to significant side effects in vulnerable individuals, and concerns regarding potential misuse or abuse.
This issue of the
Journal provides insightful reviews and original research articles focused on advances in therapeutics and treatment approaches. The findings reported here are directly relevant to the treatment of patients with major depression, psychotic disorders, obsessive-compulsive disorder (OCD), and alcohol withdrawal. This issue also includes a review of the state of the art for the use of ketamine and esketamine in psychiatry authored by McIntyre et al. (
12), as well as a review authored by Ferrarelli and Phillips on the use of TMS as a tool both for understanding pathophysiology and for treatment (
13). In addition, Maixner and coauthors contribute a commentary on the need to consider ECT as an essential treatment to facilitate the best care for our patients during the COVID-19 pandemic as well as for the future, if we have the misfortune of having to deal with other pandemics (
14).
Likelihood of Receiving Depression Treatment in Patients With Comorbid Depression and Substance Use Disorder
Coughlin et al. (
15) report data that address the important issue of treatment for patients with comorbid depression and substance use disorder. Using a retrospective design from a 2017 data set of 53,034 veterans diagnosed with depression, the authors assessed the extent to which depressed veterans with and without substance use disorders received appropriate outpatient treatment for depression. Of the depressed patients, 14.2% had a comorbid substance use disorder diagnosis within the prior year. Of the total group of depressed patients, only 52.9% received any antidepressant treatment, and of these, 34% received psychotherapy for depression. This finding, especially since the patients were actually diagnosed with depression, is troubling in and of itself. Moreover, the authors found that the depressed patients with comorbid substance use disorder, compared with depressed patients without comorbidity, had 21% lower odds of receiving appropriate acute antidepressant treatment and 13% lower odds of engaging in acute-phase psychotherapy for depression. Similar reductions in longer-term ongoing care were observed for depressed patients with comorbid substance use disorder. The authors discuss the importance of concurrently addressing both depression and substance use disorder issues, the numerous reasons that could account for the reduced quality of care experienced by individuals with depression and comorbid substance use disorder, and the need to address and overcome these barriers.
Relapse Prevention and Acceptability of Long-Acting Injectable (LAI) Antipsychotic Medication
Ostuzzi et al. (
16) performed a network meta-analysis to compare the efficacy and acceptability of LAIs in patients with nonaffective psychotic disorders. A network meta-analysis is a method that allows for the comparison of different treatments, the comparisons of which may or may not be performed within the same study. In this network meta-analysis, the authors analyzed treatment studies that lasted at least 12 weeks and also included studies in which LAIs were compared with oral antipsychotic medication. Outcome data from 11,505 patients were included in the analysis. Not surprisingly, the authors found that most LAIs were significantly better than placebo in preventing relapse. Although the largest effects were seen for the paliperidone 3-month formulation and for aripiprazole, the magnitude of these effects did not significantly differ from that of the other LAIs. In relation to acceptability, aripiprazole outperformed a number of the other LAIs. Because the quality of the evidence for both the relapse and acceptability outcomes was the highest for paliperidone (3-month and 1-month formulations), aripiprazole, and olanzapine, and given the relapse and acceptability findings, the authors suggest that these LAIs should be used as first-line treatments. Dr. William Honer from the University of British Columbia provides an editorial (
17) that places these findings in the context of other studies and more broadly discusses the important implications of relapse prevention in patients with psychotic disorders.
Clinical Trial Targeting a Potassium Channel as Novel Strategy for Treating Depression and Anhedonia
In a small but interesting double-blind randomized clinical trial in patients with major depression, Costi et al. (
18) compared the effects of ezogabine, a positive modulator of specific voltage-gated potassium channels (KCNQ2/3), with placebo. This approach was based on preclinical evidence that linked these specific voltage-gated potassium channels to depression and the function of reward-related circuitry. This study, and its outcome measures, was designed in line with the new drug development strategy from the National Institute of Mental Health (NIMH) that is based on first establishing evidence for target engagement (
19). Therefore, as a means to focus on mechanisms underlying anhedonia, the primary endpoint for this study was a functional neuroimaging marker assessing activation of reward-related circuitry. The secondary endpoints were reductions in depression and anhedonia severity. Based on the primary endpoint, the study failed, as ezogabine was not found to significantly increase reward-related activation of the ventral striatum. However, the secondary endpoints were reached, demonstrating significant reductions in depression and anhedonia ratings. These findings present an interesting conundrum that Dr. Alan Schatzberg from Stanford University addresses in his editorial (
20). In his piece, Schatzberg questions the wisdom of the NIMH “fast-fail trial” strategy with the goal of first demonstrating target engagement before moving forward with further psychopharmacological drug development. This issue is particularly poignant in relation to the ezogabine clinical trial reported here as the potentially important findings revealed by this trial could be discounted because of a lack of evidence of “target engagement,” thus preventing further study.
Prazosin Treatment for Alcohol Dependence in Relation to Alcohol Withdrawal Symptoms
Sinha and coauthors (
21) present data from a 12-week double-blind clinical trial examining the effects of the α
1 adrenergic antagonist prazosin on alcohol intake and associated affective and craving symptoms. The study involved 100 patients with current alcohol dependence and varying degrees of withdrawal symptoms who were randomly assigned to receive either placebo or prazosin (16 mg/day, titrated to this dosage over a 2-week period). Primary outcome measures were self-reported drinking days, and secondary outcomes were mood, anxiety, craving, and sleep symptoms. Interestingly, the authors found that prazosin was helpful in patients who presented with higher levels of withdrawal symptoms but was not effective in the subset of individuals with low levels of these symptoms. For example, in the higher withdrawal symptom group, patients given prazosin reported drinking on 27% of days during the trial compared with 58% for the comparison placebo group. These patients also had significant improvements in anxiety, depression, and craving. Importantly, no significant positive effects of prazosin were found in patients in the low withdrawal symptom group. While preliminary, these findings suggest that prazosin may be particularly helpful for drinking reduction in a subset of patients with substance use disorder who concurrently experience withdrawal symptoms. In her editorial (
22), Dr. Barbara Mason from the Scripps Research Institute comments on the findings and also notes that while the authors of the article referred to the prazosin-responsive patients in their study as having higher levels of withdrawal symptoms, in reality the levels as assessed by rating scales were relatively low. She also provides a helpful overview of the current treatments for alcohol use disorder (AUD) and a more in-depth discussion of prazosin as a possible treatment particularly relevant to the affective and anxiety symptoms associated with AUD.
Using Theta Burst TBS to Causally Link Reduced Orbitofrontal Cortex Function to Reductions in Compulsive Behaviors
Price and coauthors (
23) report findings from a creative study that uses different patterns of theta burst TMS to test the role of the orbitofrontal cortex (OFC) in modulating compulsive behaviors. In this double-blind study, 69 patients with compulsive behavior disorders (OCD, excoriation disorder, trichotillomania, body dysmorphic disorder) received either one session of iTBS or continuous TBS (cTBS) targeted at the left OFC. Immediately after TBS, the patients engaged in a training session that was focused on overriding habit formation. iTBS is thought to acutely increase neural activity, whereas cTBS is thought to have the opposite effect. In findings consistent with these beliefs, the researchers found that iTBS increased, while cTBS decreased, blood flow in the OFC and other surrounding regions. Importantly, cTBS, combined with the post-cTBS training session, resulted in reductions in laboratory-based measures of compulsive behaviors that were observed both acutely and 1 week after the intervention. This was not the case in the patients who received the iTBS intervention. It is important to note that the design of this study did not allow the researchers to parse the effects of cTBS from those of the post-TBS habit override training session. Furthermore, despite the demonstrated improvements in compulsive behaviors in the cTBS group, when challenged in the laboratory, these patients did not experience a significant reduction in their real-world symptoms. This work is meaningful for a number of reasons, including the capacity to target the OFC with TBS, the use of TBS as a causal probe, and the suggestion that it is the combination of modulating brain activity with specific cognitive training that may be most useful in achieving behavioral and psychological effects. In their editorial (
24), Jennifer Lissemore, a Ph.D. student, and Dr. Nolan Williams—both from Stanford University—review the brain modulation strategies used to treat OCD, consider the meaning and transdiagnostic nature of these new findings, and point to studies that will be needed to build on this work.
Conclusions
The findings reported in this issue of the Journal highlight new data and advances in conceptualizing new treatments in psychiatry. While sometimes not obvious in our day-to-day clinical work, it is important to emphasize that we have come a long way since the early 2000s. This issue provides the following insights into improving current treatment approaches and in the development of new treatments: 1) ketamine and esketamine in relation to clinical use; 2) TMS as both a treatment and a neural probe for causal human studies; 3) the critical need to recognize, and concurrently treat, depression and comorbid substance use disorder; 4) evidence supporting the use of specific LAI antipsychotics for psychosis relapse prevention; 5) a potassium channel–modulating drug as a potential new treatment for anhedonia and depression; 6) the efficacy of prazosin for AUD patients with withdrawal symptoms; and 7) the OFC as a cTBS target for treating transdiagnostic compulsive behaviors.
It is important to emphasize that new treatment advances are not only clinically relevant but that they also, based on their novel mechanisms, open new avenues for drug discovery and development. Ultimately, a more complete understanding of the pathophysiology of the illnesses that we treat will provide a neuroscientific blueprint for further novel intervention strategies. As we develop treatments that are more aligned with etiology and pathophysiology, the hope is that our interventions will move beyond symptomatic treatments and toward actually repairing or restoring molecular, cellular, and circuit alterations that sustain the recurrence and chronicity of many psychiatric illnesses. Also, it is likely that interventions early in the onset of illnesses, ideally prior to their full-blown expression, will be more likely to have long-term salutary effects. In this regard, because many psychiatric illnesses have neurodevelopmental origins, a greater emphasis on childhood interventions is in our future.