Mental health outcomes can vary widely following major life stressors like a traumatic event. In fact, the variability in patient outcomes can range from those who are symptom free to those who suffer severe emotional distress (
1–
3). Furthermore, the profile of symptom expression often varies widely from person to person. Although there is some evidence that the nature of stressful events may affect the type, severity, and profile of symptom presentation, the nature of the event itself does not fully account for the entire range of mental health outcomes (
2). This variability presumably relies, at least in part, on interindividual differences in prior life experiences, which affect the cognitive, behavioral, and neurobiological underpinnings of these mental health outcomes (
3). Thus, an important objective of translational neuroscience research is the development of neurobiological models that elucidate the processes that mediate psychiatric disorders.
A better understanding of the complex range of neurobiological consequences associated with trauma exposure is needed to develop neural markers that effectively predict susceptibility and resilience to posttraumatic stress. Although previous research has made important advances to our understanding of the neurobiological basis of psychiatric conditions like posttraumatic stress disorder (PTSD), significant gaps remain in our knowledge of the neural processes that underlie the heterogeneous psychiatric outcomes that are often observed following a trauma (
3,
4). For example, we know relatively little about the manner in which separate dimensions of neurocognitive function interact to influence psychiatric outcomes. This gap in our knowledge highlights an important limitation of previous neuroimaging projects that have largely focused on studies assessing a single dimension of neurocognitive function (e.g., fear processing). Thus, there have only been a few integrative multidimensional neuroimaging studies that have investigated mental health outcomes following trauma exposure (
5,
6). Additional multidimensional neuroimaging studies are needed to build neurobiological models that can effectively predict susceptibility and resilience to psychiatric conditions. Furthermore, there have been relatively few studies that have assessed brain function acutely after a major life stressor (e.g., a traumatic event), then followed participants longitudinally to identify relationships between acutely assessed neurobiological processes and future outcomes (
5,
7,
8). The acute impact that major life stressors have on neural function may have an important influence on the nature of the mental health outcomes that are ultimately displayed. Therefore, determining the relationship between acutely assessed brain function and future symptom profiles may elucidate the neurobehavioral processes that underlie the heterogeneous psychiatric presentations that often develop following trauma.
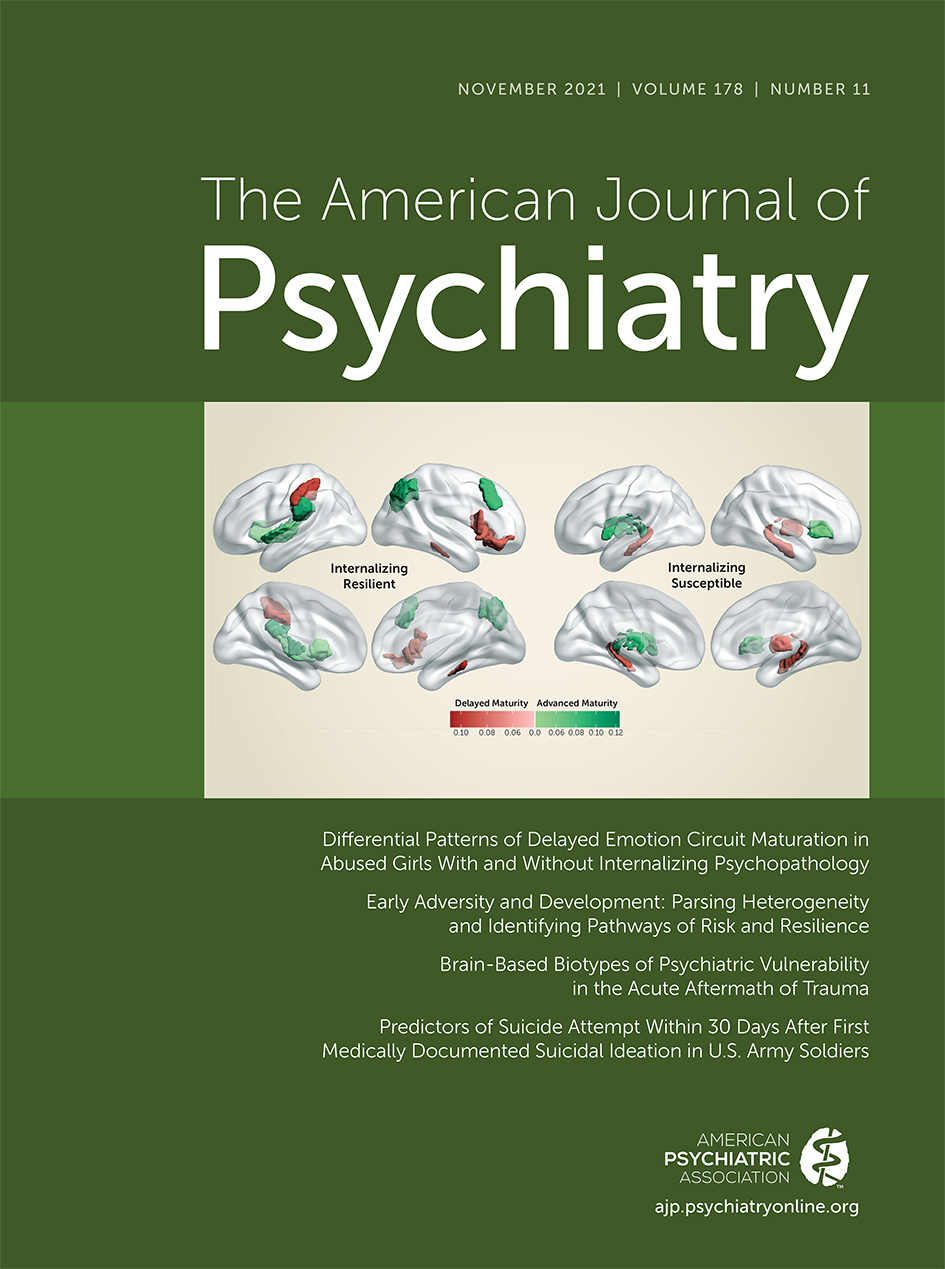
In this issue of the
Journal, Stevens and colleagues (
9) detail the findings of a longitudinal, transdiagnostic study (the Advancing Understanding of Recovery After Trauma study [
6]) that investigated relationships between trauma exposure, neural function, and symptom presentation in an effort to identify neurobiological predictors of risk and resilience to posttraumatic stress. The study included 146 participants, separated into discovery (N=69) and replication (N=77) cohorts, who completed functional MRI (fMRI) during threat, reward, and inhibitory control tasks approximately 2 weeks after a traumatic event. A hierarchical clustering approach, used on data from the discovery cohort, identified four clusters of participants that showed distinct brain response patterns to the fMRI tasks. The participants were grouped as 1) reactive/disinhibited (i.e., those who showed high reactivity within brain regions that support reward and threat-related processes and limited activity within regions that support inhibitory control functions); 2) low reward/high threat (i.e., those who showed high reactivity to threat and low reactivity to reward); 3) high reward (i.e., those who showed limited neural reactivity to threat and inhibitory control tasks and high reactivity to reward); and 4) inhibited (i.e., those who showed limited reactivity to reward, deactivation to threat, and increased activity during inhibitory control). Similar results were obtained from the replication cohort, with the exception of the high reward phenotype, which may have merged with the reactive/disinhibited group due to the higher-acuity traumas that were generally experienced by the replication cohort. Outcomes were assessed 2 weeks, 8 weeks, 3 months, and 6 months posttrauma for each of the three groups that replicated across cohorts (i.e., the reactive/disinhibited, low reward/high threat, and inhibited groups). The reactive/disinhibited group (categorized based on multidimensional neurocognitive data collected 2 weeks posttrauma) showed greater PTSD symptom severity as well as higher anxiety symptoms (assessed 2 weeks to 6 months posttrauma) than other groups. The neurocognitive groupings did not predict symptoms of depression, dissociation, or impulsivity. The findings from this study suggest that patient groupings, based on the neural response to multidimensional cognitive tasks, may predict distinct posttrauma outcomes. Specifically, those who show a reactive and disinhibited pattern of brain function following trauma exposure appear most likely to develop symptoms of anxiety and PTSD.
The study by Stevens and colleagues is innovative in several ways. First, it assessed participants’ neurocognitive function acutely (i.e., ∼2 weeks) following trauma exposure. Aside from a few exceptions (
5,
7,
8,
10), previous posttraumatic stress research has generally studied chronic PTSD patients. Thus, relatively few studies have assessed relationships between posttraumatic stress and brain function acutely following a trauma. Assessing neural markers of posttraumatic stress acutely after trauma exposure may be particularly important given that acute neurobiological processes seem prone to influence the future neurobehavioral presentation of individuals who ultimately develop PTSD. Second, this study advances the field by taking a multidimensional neurocognitive approach to the assessment of threat, reward, and inhibitory processes. Prior work has largely focused on identifying the neural substrates of a single dimension of cognitive or emotional function (e.g., response inhibition, fear processing) in relation to PTSD (
7,
8,
10). As demonstrated by Stevens and colleagues (
9), integrating multiple dimensions of neurocognitive function may elucidate the mosaic of interrelated neurobiological processes that underlie the development of PTSD. A third innovative aspect of this study is that participants were categorized based on neural profiles independent of the traditional diagnostic categories that are often used in this type of research. Previous work has generally studied brain activity related to specific clinical features of interest. In contrast, Stevens and colleagues first used a data-driven approach to identify multidimensional neural profiles, then linked those neural profiles to the subsequent emergence of psychiatric symptoms. An advantage of this approach is that it can identify distinct neurobiological signatures that predict future susceptibility or resilience to posttraumatic stress, without restricting the approach to specific features of a particular diagnosis. In summary, this project acutely assessed a multidimensional set of neurocognitive functions, independent of traditional diagnostic criteria, to identify neural profiles that predict susceptibility and resilience to posttraumatic stress. The findings from this study demonstrate the potential of neuroimaging tools to elucidate some of the heterogeneity of posttrauma outcomes.
In their study, Stevens and colleagues focus on an important but nascent area of psychiatric research. There is increasing interest in multidimensional data-driven approaches for predicting future mental health outcomes in patient populations (
1,
3–
5). Analytic approaches that integrate multiple dimensions of the broader range of neurocognitive function will likely be necessary to advance our understanding of psychiatric disorders. Multidimensional imaging approaches may provide the means to identify interrelated patterns among distinct neurocognitive functions that would otherwise remain concealed. Identifying these latent patterns will likely advance our capability to develop more complete neurocognitive profiles of psychiatric conditions. Developing neurocognitive models of these psychiatric conditions is particularly important given that the current approach to psychiatric diagnosis generally does not integrate neurobiological information. Instead, diagnosis primarily relies upon the identification of cognitive and behavioral symptoms that match the specific features of a diagnostic category. Furthermore, the general analytic approach taken by this study could advance efforts to identify patterns of neurocognitive dysfunction that show commonalities across multiple psychiatric conditions. At the same time, other neurocognitive profiles could be used to distinguish separate disorders. Thus, this type of research direction seems primed to advance our current understanding of important neurobiological processes that underlie psychiatric conditions. The approach used by Stevens and colleagues provides a model for translational research that may pave the way for the future development of neuroimaging-based prediction techniques. These techniques have the potential to enhance our ability to identify those at greatest risk, which could provide the basis upon which to initiate early intervention strategies that may improve patient outcomes. Similarly, these techniques could ultimately lead to improvements in diagnostic precision that may, over time, better target the treatment selection for psychiatric disorders with complex and heterogeneous symptom presentations.