That childhood abuse can lead to significant negative outcomes for the abused is not debatable. What is less clearly understood is how this occurs, especially on a biological level. Many studies, including a recent meta-analysis, have noted that adversity experienced early in life may accelerate maturation (
1). This has been described as the stress acceleration hypothesis, which posits that early stress advances brain development (
2). However, there is also evidence that different adversity types may have differential effects; for example, abuse (i.e., threat-related adversity) and neglect (i.e., deprivation-related adversity) may have opposite maturational effects (
3). Such mixed findings from heterogenous samples have led to some confusion in the field; the study by Keding and colleagues (
4), in this issue of the
Journal, moves this debate forward by separately examining the impact of abuse and neglect on brain maturation and internalizing psychopathology in girls.
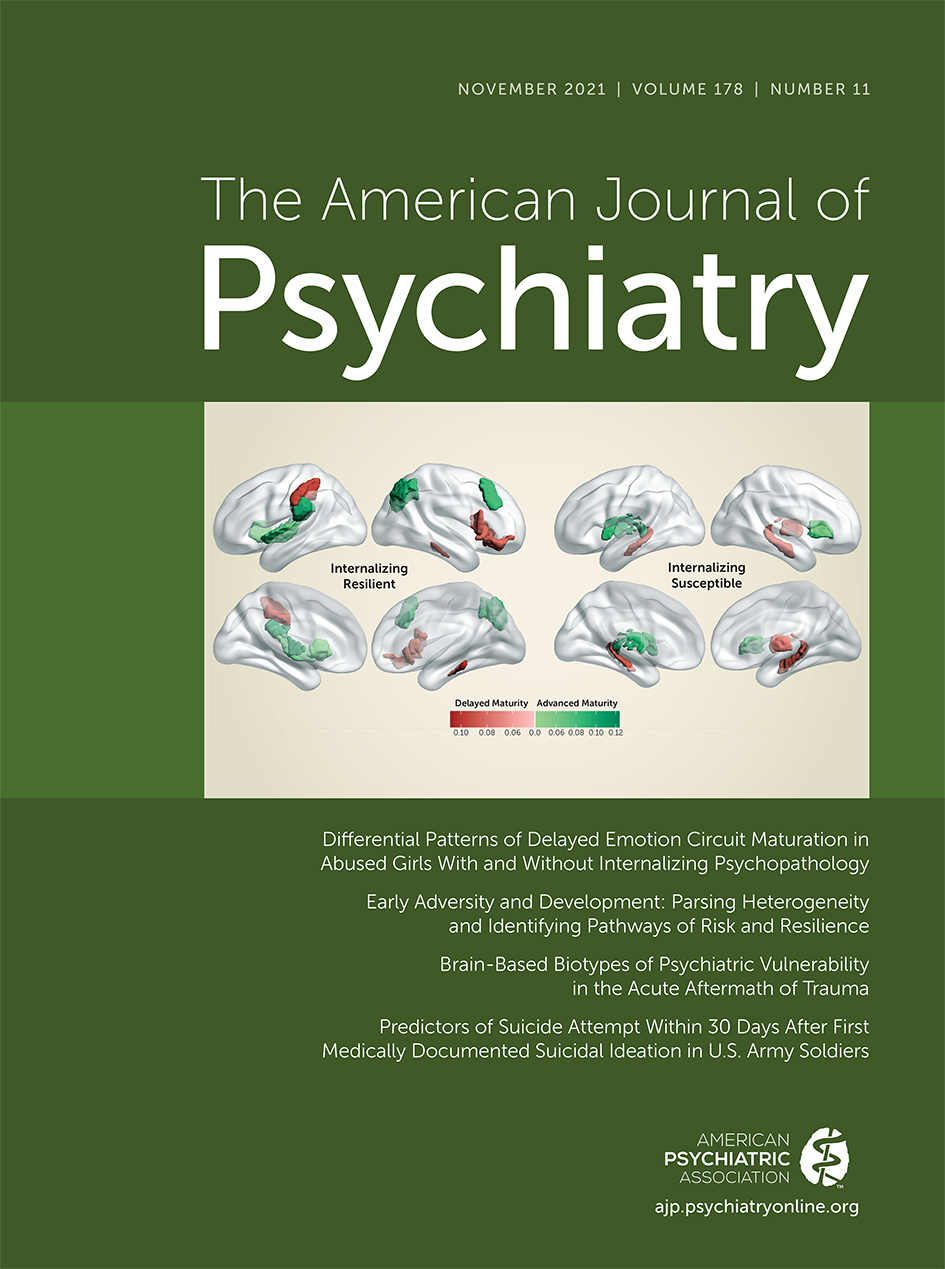
It is important to better understand how abuse may affect maturation but also how such alterations in maturation affect health and disease in the long-term. Moreover, why do some abused girls develop psychopathology while others do not? The study by Keding and colleagues does not answer all of these questions, but it does separately examine resilient girls compared with susceptible girls (i.e., those with either no/low versus high internalizing psychopathology symptoms). Keding and colleagues used structural MRI data and a stacked machine learning algorithm to examine brain maturation in a large sample (N=234) of 8- to 18-year old girls scanned at three study sites. These participants were divided into three groups: no abuse history, abuse without psychopathology, and abuse with internalizing psychopathology. The abuse group included all girls who self-reported any experience of physical, sexual, or emotional abuse. Self-reported neglect score was used as a continuous variable. The brain age gap estimation (BrainAGE) algorithm derives an index of either delayed or accelerated brain development relative to chronological age. The key results indicate that 1) neglect can lead to accelerated brain maturation, while abuse may delay maturation, primarily in emotion circuits; 2) this delayed maturation is associated with higher hyperarousal symptoms in abused girls; and 3) brain maturation patterns differ between resilient and susceptible abused girls. Importantly, these data were cross-sectional, and therefore the results are correlational and not causal.
Keding and colleagues report that abuse and neglect had opposite associations with brain development: abuse delayed, whereas neglect accelerated, maturation. The reported associations differ in specificity as well as direction. Neglect was associated with whole-brain maturation, while abuse was related to maturation of emotion circuitry, including the amygdala, hippocampus, cingulate, and insula. These differential effects have important implications for understanding the impact of adversity on brain development given that according to the 2019 Child Maltreatment report by the U.S. Department of Health and Human Services, 61% of maltreated children report neglect, 23.5% report abuse, and 15.5% experience both neglect and abuse. For those 15% of children exposed to both forms of adversity, the opposing patterns of maturation may mask the impact of each and result in mixed findings in the literature, underscoring the need to assess both in any research of brain development. Keding and colleagues assessed and analyzed abuse and neglect; however, the study was primarily designed to test the impact of abuse, with more girls in their sample having no exposure to neglect than having experienced physical neglect. For this reason, the study does not provide strong insight into the impact of neglect in the absence of abuse, or even for individuals who might experience high levels of both abuse and neglect. Additional studies that examine how abuse and neglect jointly affect brain development are needed.
The specificity of findings pointing to delayed maturation of emotion circuits is highly interesting and clinically significant. Abused girls did not show any delays in whole-brain maturation or language-relevant circuits. This underscores the importance of emotion processing circuits in understanding the link between abuse and subsequent health risks. Previous research has identified emotion-related difficulties in children who were victims of abuse, including problems identifying emotional facial expressions (
5), disengaging attention from angry faces (
6), and regulating emotion (
7). Although it is unclear whether delayed maturation of emotion circuits underlies these problems, these findings lay the groundwork for future studies to make this link more explicitly.
Taken together, these data highlight potential mechanisms underlying risk for posttraumatic stress disorder (PTSD) in abused girls. Critically, susceptible girls showed delayed maturation of the hippocampus, a limbic brain structure that has repeatedly been associated with trauma outcomes. Those with chronic PTSD have smaller hippocampi compared with control subjects (
8), and prospective studies of adults have shown that hippocampus activity after trauma increases resilience and decreases risk for later PTSD (
9). Keding and colleagues suggest that delayed maturation of emotion circuits may lead to increased hyperarousal via increased threat generalization. Increased threat generalization and poor discrimination between threat and safety has been linked both with PTSD symptoms broadly (
10) and hyperarousal specifically (
11). The hippocampus has also been implicated in safety learning (
12) and could be a key link between early abuse, impaired inhibition of fear to safety versus threat signals, and risk for PTSD. Studies have especially supported the association between safety learning and PTSD in women (
13), specifically those with lower estrogen levels (
14). Because the study by Keding and colleagues specifically examined abused girls, their results are consistent with this pathway to risk in female subjects. Further work should test whether the same relationships are also found in male subjects.
Although the analyses did not incorporate information about the specific age(s) when participants experienced abuse or neglect, Keding and colleagues note that brain structure-specific developmental trajectories may affect the relationship between abuse, neglect, and brain development. Studies indicate that age of abuse exposure affects subsequent effects on brain structure (
15). Recent work has highlighted puberty as a sensitive period for fear learning (
16) and for recalibration of the stress response system (
17), suggesting that the effects of abuse may depend on whether it is experienced pre- or postpuberty. Indeed, the positive association between childhood maltreatment and amygdala volume is strongest when maltreatment exposure occurred near the onset of puberty (
18). The study by Keding and colleagues sets the stage for future studies to incorporate age of exposure into analyses of the associations between abuse, neglect, brain structure, and internalizing psychopathology.
Prior studies indicate that both the developmental timing and type of abuse may affect both psychopathology risk (
19) and brain development in nuanced ways (
15). Keding and colleague’s results provide an overarching summary of how abuse and neglect affect girls: regardless of developmental timing or type, abuse is associated with delayed emotion circuit maturation, and neglect is associated with accelerated brain development. These results suggest that abuse and neglect may result in a developmental mismatch between the child’s age and brain maturation, such that the capabilities of the child are not aligned with the demands of her environment. The association between lower BrainAGE values and more hyperarousal symptoms may be one example of how developmental mismatches confer mental health risk. This highlights the need for future work that examines how either acceleration or delay of typical development may modulate health risk and resilience in abused and neglected girls.