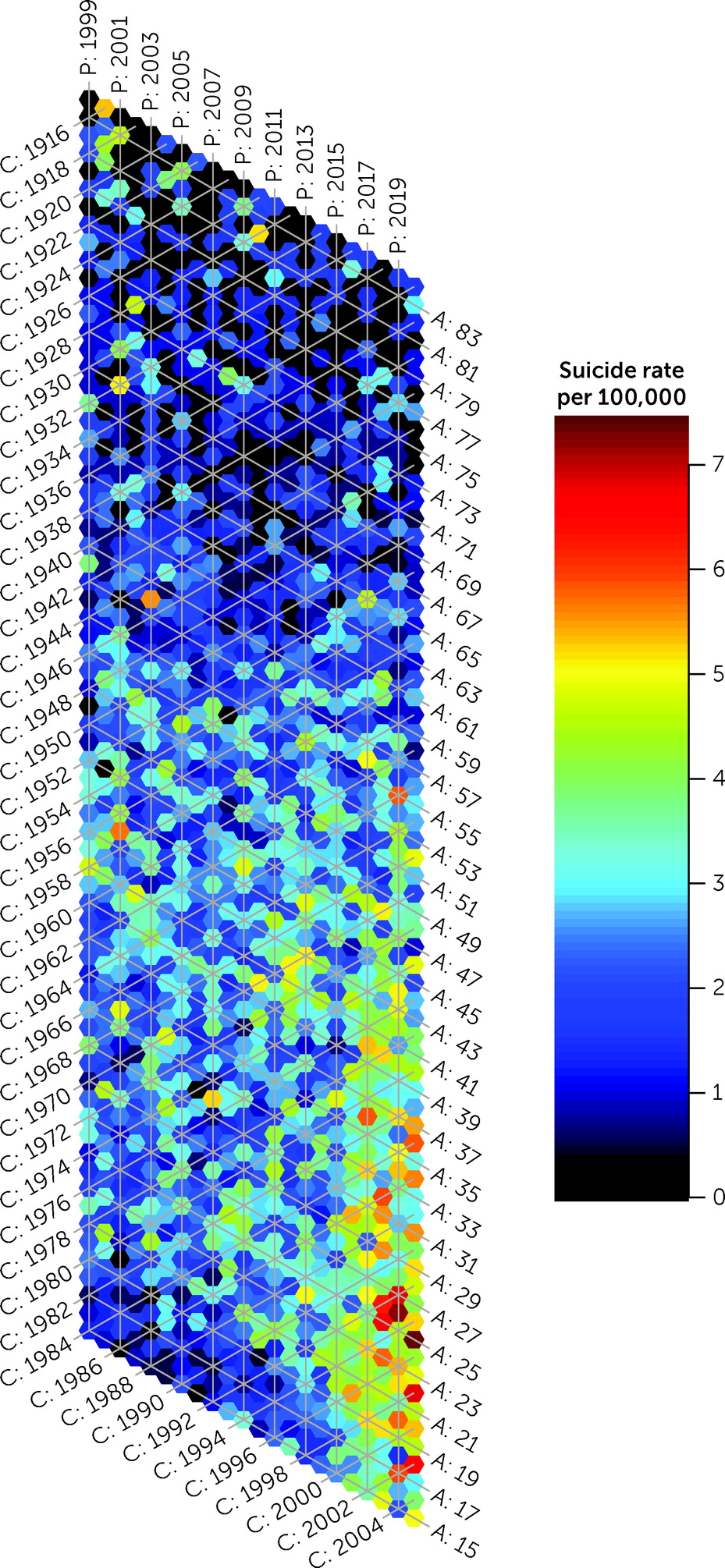
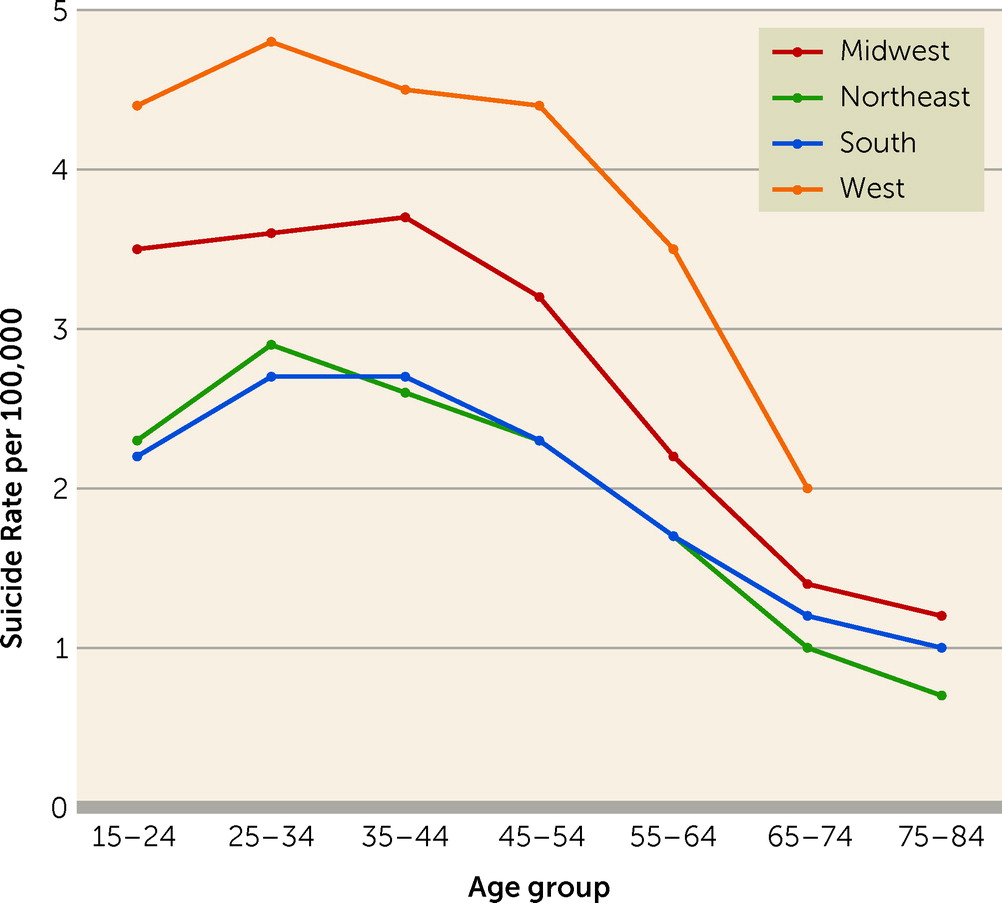
The findings indicate strong APC effects with suicide increasing rapidly among Black females and particularly concerning trends among individuals born in the most recent birth cohorts. In addition, state and regional variation demonstrate that the highest suicide rates were concentrated in the West, with the most deaths occurring in the South (due to higher Black population counts in the South).
Our findings are in line with evidence that suicidal behaviors are increasing among minoritized youth (
15). Importantly, interventions targeting certain stressors may be particularly salient for young Black females, with evidence indicating that cyberbullying and online racial attacks toward Black female youth are on the rise (
16). Access to help during suicidal crises is a critical component of suicide prevention efforts (
17); however, structural racism—the ways in which values are assigned, maintained or codified in law based on racialized group membership (
18)–can reduce access to care of Black youth due to experiences of stigma and mistrust of support systems. For example, this may hinder use of police-led crisis intervention teams in the context of heightened awareness regarding police brutality toward Black individuals. Findings also highlight high rates among those aged 25–27 years, suggesting that this age may be a developmental period for Black women with particular need of additional support. Women in their late 20s may be entering early adulthood in full time work, thus introduced to workplace discrimination (
19) or receiving maternal health stressors (
20) via entering parenthood and enduring childbirth, during which Black women have increased morbidity and mortality (
21). Given these patterns, additional research on early adulthood stressors among Black women is warranted. Furthermore, intimate partner violence, neighborhood violence, and poverty also contribute to poor mental health outcomes and limited treatment access, and are overrepresented risk factors among Black girls and women in some areas (
22,
23). Factors such as feelings of worthlessness and diminished verbal affirmations from parents may also increase suicide risk among Black adolescent girls (
24) and are important foci for further research. Reducing barriers in access to care via implementation of community-based, culturally competent care programs is an urgent public health need (
25).
To our knowledge, this is the first study to examine the epidemiology of suicide among Black females in the U.S. by geographical region. Limitations include potential administrative misclassification of suicide mortality (
26). Furthermore, death certificates only include data on sex assigned at birth, and do not include information on prior suicide attempts, psychiatric disorder history, or mental health service use; more in-depth psychological and social autopsy studies of suicide deaths in the United States with such information would add considerable value to research in this field. Future research should consider state level trends and analyses among various ethnicities and gender identities.