Major depressive disorder is a prevalent and debilitating condition treated with two equally efficacious first-line treatments: antidepressant medication or evidence-based psychotherapy, such as cognitive-behavioral therapy (CBT) (
1). The goal of the acute phase of treatment for major depression is remission (
2), which reflects a return to a high level of psychosocial functioning and is associated with a reduced risk of depressive relapse (
3,
4). CBT and medication treatment of outpatients with major depression yield similar overall remission rates, but there are clearly individual patients who respond to one form of treatment but not the other (
5,
6). Although the two forms of treatment are conceptualized to yield improvements via highly differing actions in the brain (
7), there is a dearth of empirical data relevant to and supporting these hypothesized models. Only a few small studies have contrasted the changes in brain metabolism or blood flow associated with the two treatments (
8–
11). Improved understanding of treatment-specific effects will help personalize treatments for major depression and inform its longitudinal management.
The past decade of neuroimaging research has revealed distributed brain networks whose activity is associated with specific functions. Four specific networks have been consistently implicated in the pathophysiology of major depressive disorder (
12). The default mode network (DMN) primarily comprises the medial prefrontal cortex (mPFC), posterior cingulate cortex (PCC)/precuneus, and bilateral inferior parietal lobes; it is the dominant network during internally focused activity (
13–
16). The executive control network (ECN; also known as the cognitive control network or fronto-parietal network) includes the dorsolateral prefrontal cortex (DLPFC), anterior cingulate cortex (ACC), and posterior parietal cortex (
13). The ECN is engaged during externally focused tasks and is believed to contribute to regulation of emotion through control over limbic regions (
17). The salience network (SN) (broadly similar to the ventral attention network) comprises the ACC, anterior insula, and several subcortical regions, including the amygdala, hypothalamus, ventral striatum, thalamus, and specific brainstem nuclei involved in emotion processing and regulation. This network detects behaviorally relevant stimuli, including ascending interoceptive signals processed through the posterior and mid-insula, which are integrated in the fronto-insular cortex (
18). The SN coordinates neural responses to salient stimuli by directing the switch between ECN- and DMN-predominant activity (
19) and regulating viscero-autonomic activity (
20) through descending projections to nuclei in the brainstem and spinal cord (
21). Finally, the subcallosal cingulate cortex (SCC), part of the affective (limbic) network (AN), is a key hub for the processing of affective states and is structurally connected to the ventral striatum, midline thalamus, dorsal raphe, ACC, mPFC, and hippocampus (
22,
23).
Using seeds for the DMN, ECN, SN, and AN, we addressed the following questions regarding change in rsFC from baseline to week 12:
Discussion
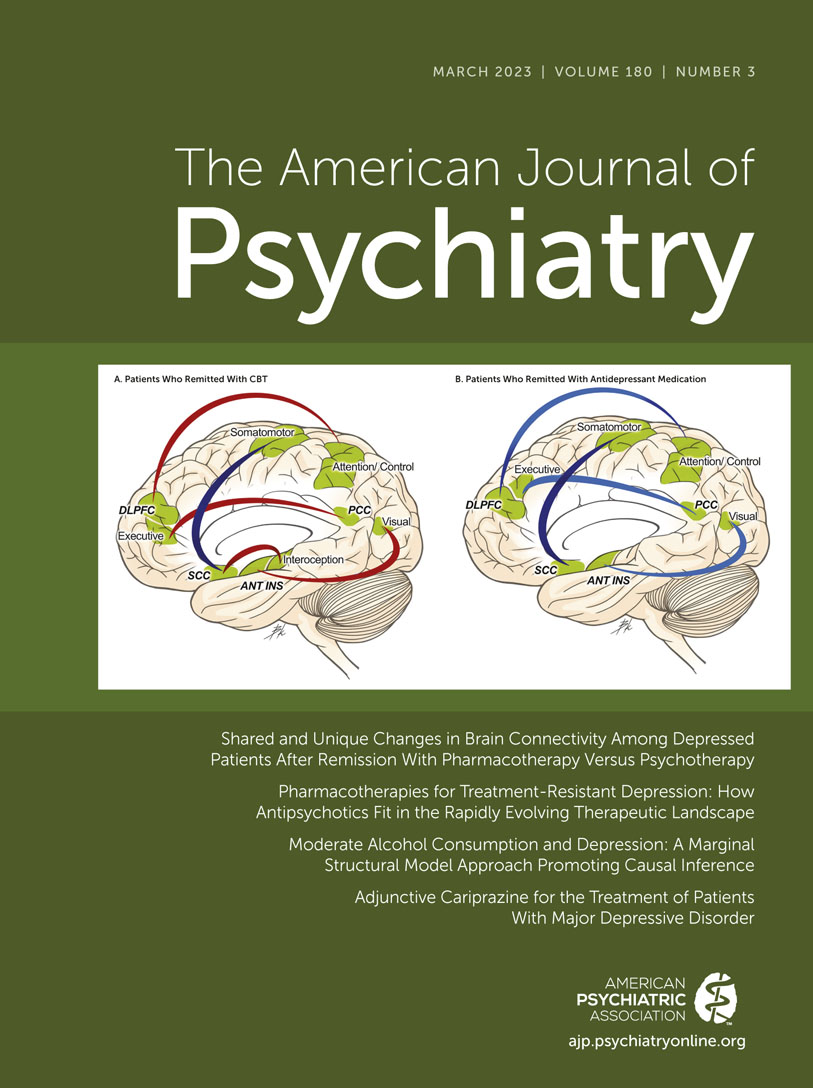
This study directly compared the changes in brain network connectivity in patients with major depressive disorder who were successfully treated to remission with antidepressant medication or CBT. The only statistically significant shared change among remitters regardless of treatment was a reduction in rsFC between the AN and the somatomotor network, particularly the medial aspect of M1 in the trunk section of Penfield’s original homunculus (
37). In contrast, the two treatments differed significantly in their effects on patterns of rsFC of the ECN, AN, and SN. Most notably, CBT remitters demonstrated enhanced connectivity of the ECN with attention regions, which did not occur in medication remitters, a change consistent with theorized mechanisms of action of CBT on the brain (
7). Additionally, whereas CBT remitters acquired greater connectivity of the AN to the posterior insula, and of the SN to the precuneus and occipital visual regions, medication remitters evinced reduced strength of these regions’ connectivity.
Figure 2 presents a schematic of the differential change patterns among CBT remitters and medication remitters.
It is important to recognize that our pre-post resting-state fMRI analyses cannot prove directionality or causality of rsFC effects. While acknowledging that caveat, the difficulty patients with major depression report in converting thoughts into physical actions (e.g., getting out of bed) may reflect a limbic inhibition of motor activation, and the finding of reduced SCC-somatomotor connectivity in remitters suggests the potential importance of reducing limbic input to motor regions as a mechanism for recovery from major depression. The primary motor cortex, including medial M1, is one of the “rich club hubs” in the brain, a moniker referring to its dense interconnectivity to hubs of other functional resting-state networks (
38). The primary motor cortex contributes to the integration of information between segregated functional domains, including the affective network. Moreover, recent work has found that primary motor neurons and the SCC both project to the adrenal medulla, potentially representing the “central command” for preparing the body to meet anticipated metabolic needs in the face of stress (
39). The colocalization of the control of this visceromotor function with skeletomotor function facilitates their coordinated responses, potentially linking the affective, motor, and neuroendocrine disturbances observed in major depression (
40). The importance of these findings for major depression is further supported by recent breakthroughs demonstrating that the motor cortex in primates, particularly medial M1, has undergone major organizational changes through evolution to achieve greater connections with the mid-cingulate cortex (
41), itself an important network hub involved in cost-benefit computations about potential physical actions (
42). The reduction in rsFC between the AN and the medial motor cortex observed in patients who remitted with both treatments suggests that reducing limbic input to motor regions may be a crucial aspect of recovery from major depression.
Other pre-post fMRI studies of improvement with medication have also identified reduced activity within the somatomotor network, including the bilateral precentral gyrus (M1) with serotonin-norepinephrine reuptake inhibitors (SNRIs) (
43), as well as reduced somatomotor network connectivity with other networks after treatment with a selective serotonin reuptake inhibitor (SSRI) (
44). Korgaonkar and colleagues (
45) recently demonstrated that
increased somatomotor–ventral attention network rsFC occurred only in patients who were nonremitters with SSRI or SNRI treatment. A recent study of rsFC change in CBT-treated patients with major depression (
46) found that treatment reduced connectivity between the SCC and the paracentral lobule, which includes motor and premotor regions. Although that study reported no significant SCC rsFC change pattern associated with symptom improvement, a secondary analysis using a more relaxed threshold found a correlation between reduction in symptom severity and reduction in SCC–supplementary motor area rsFC. Another study of 20 sessions of intermittent theta burst stimulation (
47) found that only responders demonstrated significant reductions in rsFC between the SCC seed and the premotor cortex of Brodmann area 6. It is also possible that the efficacy of exercise as a treatment for major depression involves this network (
48), although no imaging data have addressed this question. Taken together, the evidence indicates that across multiple types of treatment, reduced limbic-motor connectivity is a generalized aspect of improvement in depressive symptoms.
Our hypothesis that CBT would increase ECN rsFC was supported by the most robust findings from this analysis: large and extensive CBT-specific increases in connectivity occurred between the DLPFC and parietal regions involved in cognitive control and attention (
49), consistent with the importance of this network for major depression (
12). Furthermore, when evaluating across all CBT completers regardless of outcome, we found a significant positive correlation between percent reduction in HAM-D score and increase in ECN rsFC with the left superior parietal lobule (see Figure S2 in the
online supplement) (
3), a finding that indicates that clinical improvement is proportional to the degree of engagement of this network. Other groups have demonstrated left ECN engagement during active reappraisal of emotional meaning while attending to negative stimuli (
50,
51); reappraisal is a core component of CBT (
33). These imaging findings align well with the cognitive theory of depression, which considers impairment in control over mood-congruent material to be a core deficit of major depression that sustains the depressed mood (
52). Poor inhibition of or disengagement from negatively valenced material in working memory is believed to contribute to the negative attention bias, negative memory bias, and maladaptive coping strategies that are common in patients with major depression (
53). Taken together, these data suggest that CBT cognitive restructuring procedures enhance the connectivity of the brain networks thought to underlie these core clinical features and that lower ECN rsFC may be an intervention target for CBT. It is also notable that at week 12 of our study, compared with healthy control subjects, CBT remitters had significantly greater rsFC between the ECN and inferior parietal attentional regions. This result may reflect the effect of repetitive practice of cognitive restructuring exercises, or that patients who are capable of remitting with CBT have inherently greater connectivity than healthy control subjects between these networks when not depressed, which is only revealed upon restoration of wellness. Additional studies comparing healthy control subjects and patients with major depression who had previously remitted with CBT could further inform this question.
Patients with major depression also demonstrate greater rsFC within the DMN and between the DMN and the ECN than healthy control subjects (
12,
54), informing our second hypothesis that remission with antidepressant medication treatment would be associated with reductions in DMN within-network rsFC (
25–
28). As have other investigators (
44,
45), we found that improvement with medication was associated with broad reductions in rsFC within and between multiple networks. However, we found little evidence for a medication effect on reducing intra-DMN rsFC, although rsFC between the DMN and ECN was reduced in medication remitters. This null result is consistent with larger and more recent studies that have also failed to find significant reductions in intra-DMN rsFC among medication-treated patients (
44,
45,
55–
57). The preponderance of evidence now suggests that although increased intra-DMN rsFC distinguishes depressed individuals from healthy control subjects (
12), neither medication nor CBT significantly changes connectivity within the DMN. If this conclusion is accurate, then heightened activity in the DMN may be a trait rather than a state marker and possibly a vulnerability factor for major depression.
The finding that the rsFC of visual processing areas with the SN changes as patients achieve remission may reflect changes in the biological systems underlying the negative bias observed in patients with major depression (
58). The changes in visual cortex connectivity are consistent with rodent research demonstrating that fluoxetine enhances experience-dependent plasticity in the visual cortex; this enhancement is associated with the SSRI’s modulation of both the concentrations of brain-derived neurotrophic factor and the cortical excitatory/inhibitory balance, important regulators of neuronal plasticity in adult humans (
59,
60).
There are few published studies evaluating pre-post rsFC changes associated with improvement with other forms of depression treatment, such as ECT (
61), repetitive transcranial magnetic stimulation (rTMS) (
62), and ketamine (
63), and almost none of these studies have evaluated changes in SCC connectivity in treatment remitters. Our finding of treatment-specific effects within the ECN for CBT and antidepressant medication raises the question of whether rTMS, a treatment targeting the DLPFC, induces rsFC changes within this network; however, a recent review found no significant pre-post rTMS ECN changes across several studies (
62). In contrast, studies have demonstrated reduced SCC-DLPFC and SCC–dorsomedial PFC rsFC after response to rTMS (
62). A complicating factor for studies using highly targeted treatments, such as rTMS and deep brain stimulation, is that rsFC changes may vary with the accuracy with which the targeted region is stimulated, which can be inconsistent even with the use of fMRI-defined targeting methods (
64).
The present study has several strengths, including the large sample size comparing two first-line treatments for major depression and whole-brain voxel-wise analyses. A potential limitation to generalizability is that the sample was treatment naive. The study lacked a placebo arm, which could have informed the degree to which the rsFC changes represent inactive treatment effects. Another limitation, affecting most individual-level fMRI studies, was the inability to assess the stability of the FC mapping (
64), which might be addressed in future studies through use of emerging techniques, such as multi-echo fMRI (
65). Our analytic method employed an exploratory whole-brain analysis using nodes that are important for specific brain functions relevant to the symptomatology of major depressive disorder (
12). Future analyses could adopt a hypothesis-driven approach evaluating the degree to which CBT and antidepressant medication impact the connectivity within and between these nodes. Such an approach may reflect correction or “normalization” of aspects of abnormal connectivity believed to differentiate patients with major depression from healthy control subjects.
This work advances our understanding of how the brain changes as it emerges from depression, and it demonstrates the unique, treatment-specific changes in rsFC that are associated with remission after treatment with medication or CBT. The findings provide biological support for the common evidence-based clinical practice (
5,
6) of combining medications and CBT and of switching between modalities. It is likely that failure to engage the ECN during CBT will predict failure of that treatment modality; how soon such engagement could be evaluated to justify a change of treatment is a future research question. The differential changes between CBT and medication remitters in connectivity of the insula with the SCC and dorsal attention networks are consistent with our previous work implicating the activity of the anterior insula with differential outcomes with the two forms of treatment (
34). Finally, when considered along with the preliminary findings of functional connectivity changes occurring with other forms of treatment, such as rTMS (
62) and ketamine (
63), there is an emerging case to be made that any particular form of treatment can only work effectively (i.e., induce changes in brain function leading to remission) if the brain state at baseline is appropriate for that treatment (
34). The findings that all remitters showed lower SCC-mM1 rsFC at week 12 than healthy control subjects, and that CBT remitters specifically had higher week-12 ECN rsFC than healthy control subjects, may suggest that patients with remitted major depression do not necessarily return to a “normal” level of connectivity but rather enter an adaptive state within certain networks. Deeper understanding of these unique treatment-specific baseline and change signatures may enable further progress in personalizing treatment for major depression.