Ethical questions in treating women with psychiatric disorders often arise in relation to reproductive planning. Decisions regarding treatment during pregnancy or the postpartum period can affect multiple individuals within the family. Ideally, the patient's preferred treatment plan includes the preferences or interests of the fetus/infant, the patient's partner, important family members, and mental health providers. However, in clinical practice, what is best for the patient may not always incorporate the interests of family and caregivers. Concerns for other family members' well-being or preferences can heavily influence a woman's decisions about treatment during pregnancy and breastfeeding and even whether to pursue pregnancy at all.
The psychiatrist's responsibility is ultimately to the patient. However, women seeking care during pregnancy often prefer to discuss treatment options that also incorporate the well-being or preferences of other family members. To optimize the treatment plan in alliance with the patient, the psychiatrist should pay close attention to the particular nuances of a patient's values, illness, and capacity for decision-making, as well as the influence of other family members. The clinician should be up-to-date in his or her understanding of the objective data in the medical literature and should pay attention to his or her personal biases. A collaborative approach to decision-making between psychiatrist and patient, which includes creative problem-solving, managing anxieties around uncertainty, and clarification of priorities guided by informed consent, can assist a patient in arriving at a treatment plan.
Clinical issues in the treatment of women with psychiatric conditions
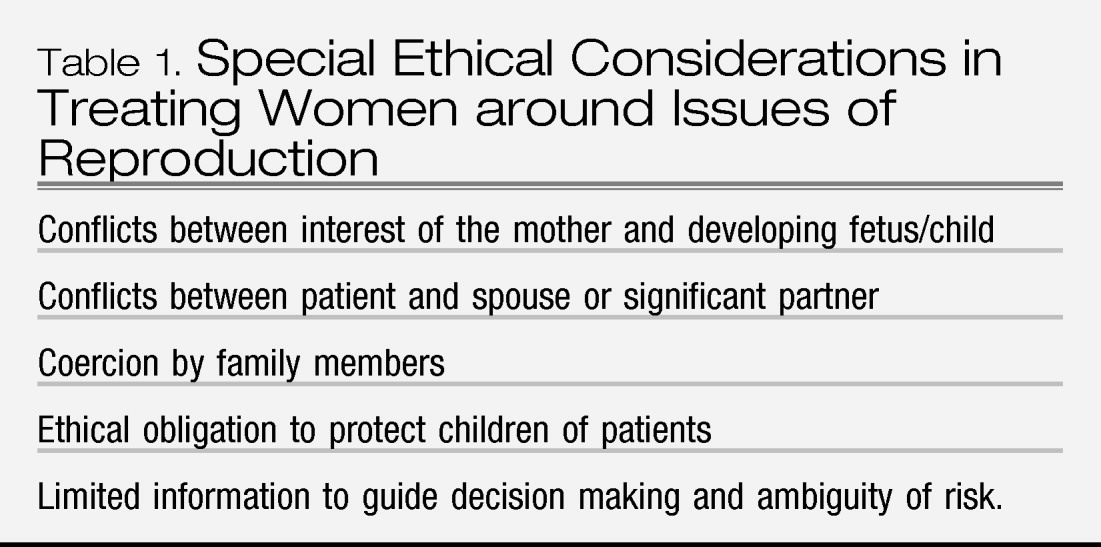
Ethical questions that arise in the overlap between psychiatric illness and reproduction may be uncovered during discussions of medication management (
Table 1). Women with mental illness who become pregnant must often face the difficult decision of whether to take medications that may be helpful or necessary to treat their condition during pregnancy and during the postpartum period. Discontinuing medications during the perinatal period is associated with risks for psychiatric decompensation (
1,
2). However, in utero exposure to psychotropic medications may also pose medical risks to the developing fetus (
3,
4). The postpartum period represents a particularly high-risk time for psychiatric decompensation (
5), in some cases calling for initiation of medication or increased dosages. Current recommendations encourage breast-feeding in the postpartum period for its numerous benefits to the infant (
6). However, psychotropic medications commonly pass into the breast milk and to the breastfed infant in some amount (
7). Women may find it difficult to choose between taking medications that are helpful for their condition, but may have deleterious effects on their developing infant through exposure in utero or through breast milk. A thorough discussion of risks and benefits of medication use is required in such situations
Current data regarding risks of in utero exposure to psychotropic medication are limited, leaving women to make difficult decisions about medication use without a complete knowledge of risks (
4). Patients may often find themselves unable or unwilling to make complicated medication decisions and may rely heavily on the psychiatrist to advise them. Such dynamics place pressure on the patient's sense of autonomy and may lead to ongoing internal struggles for the patient or power struggles around medication with her provider. Extra resources such as longer or multiple appointments, recruitment of family support, and consultation with other physicians may be required to allow patients the time and information to arrive at their own decision.
Conflicts may also occur between the values of mothers and other significant family members, such as spouses. For example, consider a woman who has been treated for severe anxiety with a selective serotonin reuptake inhibitor (SSRI) for several years who wishes to continue the medication during pregnancy; her husband, however, is opposed to in utero exposure to any medication. Such a conflict may lead to marital discord, putting the patient at further risk for perinatal mood symptoms (
8). Moreover, a woman may choose not to reveal to her spouse that she is using psychotropic medication during pregnancy to avoid such conflict, which may lead the patient to feel unsupported and isolated. Women who are pregnant may have a greater sense of obligation to follow the wishes of their partner or family members regarding treatment of their mental illness and may be vulnerable to coercion. Discussion of risks and benefits of medication use during pregnancy, with attention to a patient's worries of pursuing treatment or not pursuing treatment, often allow psychiatrists to uncover ongoing conflicts in the patient's relationships. The psychiatrist may consider recommending individual or couple's counseling to improve communication skills and bolster the patient's capacity for conflict resolution. In addition, individual psychotherapy may be an effective and adequate treatment for psychiatric symptoms and allow for reduced use or discontinuation of medication during pregnancy (
9).
Women with mental illness are vulnerable to decompensation in the postpartum period (
5), which, if untreated, may interfere with child care. It should be noted that women with psychiatric illness, particularly when symptoms are in remission, do not necessarily provide poorer child care. Remission of psychiatric illness in mothers is associated with improvements in behavior and functioning of children (
10). Therefore, psychiatrists should be vigilant about monitoring for untreated symptoms that may lead to an erosion of self-care or insight, placing children at risk for abuse or neglect. Such situations place psychiatrists in the difficult position of advocating both for child and patient and may necessitate notifying outside agencies of child welfare concerns.
Inquiry into a patient's mental health symptoms may include the patient's current functioning and capacity to care for her child, as well as requests to collect collateral information from family members or other health professionals involved in the patient's care. Such inquiries should be handled with compassion emphasizing the patient's functioning and well-being. Highly anxious or paranoid patients seeking care in the postpartum period often fear that they are not doing a good enough job in their new role and sometimes can interpret inquiries into the infant's well-being as accusations of poor mothering.
Informed consent and treatment of psychiatric illness during pregnancy
The treating psychiatrist may find himself or herself in the unique position of guiding patients through decisions regarding treatment during pregnancy and may rely on an understanding of the components of informed consent to shape such discussions. Although informed consent may have already been established at the initial prescribing of medication, the details and stakes may change during pregnancy, calling for a revisit to the discussion of risks, benefits, and alternatives to medication use.
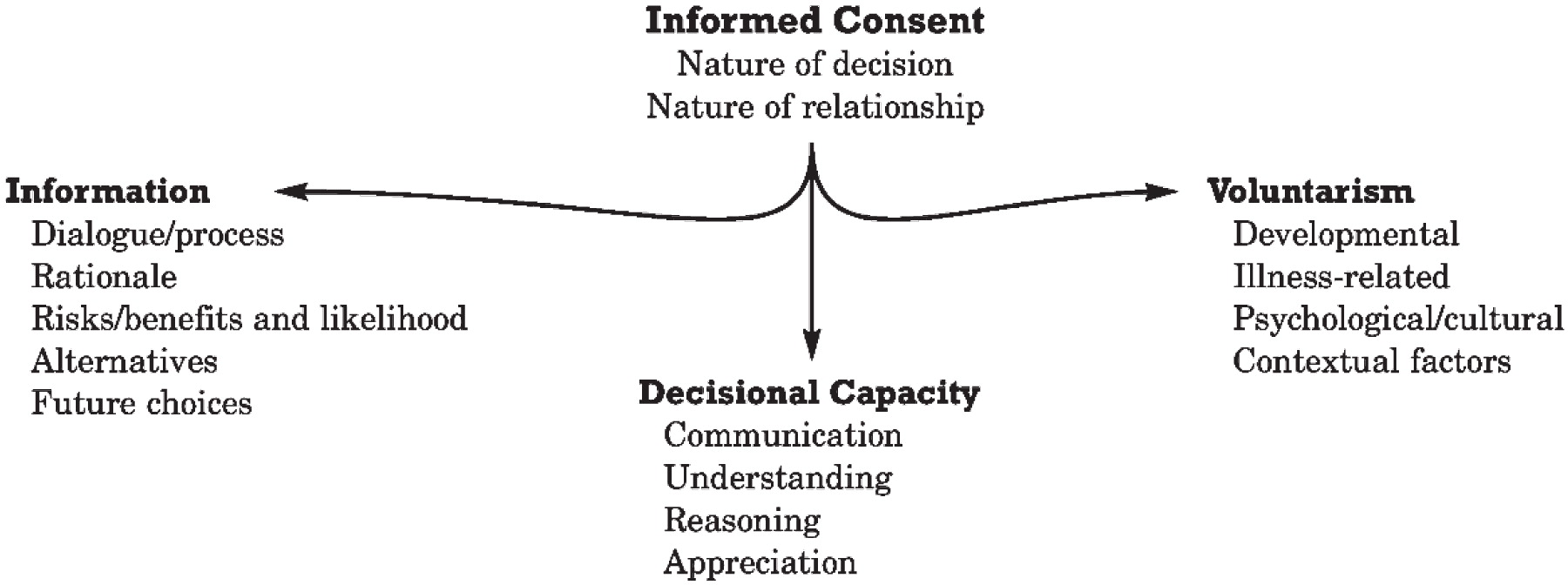
The informed consent process (
Figure 1) is built upon the foundation of a positive patient-doctor relationship. The consent/refusal decision in clinical situations occurs in the context of a relationship that has the well-being of the patient as its fundamental aim. Recommendations will be built on the basis of the medical and psychosocial issues of the patient and will seek optimal outcomes for the patient (
11). The following components are essential to the informed consent process:
1.
Information. The patient should be provided with accurate information regarding the risks, benefits, and expected outcomes of a treatment and available alternative treatments. The amount of detail of information should be tailored to what would be useful for the patient for the purposes of making a decision. The clinician may sometimes have to limit information to incremental, “digestible” amounts of data but should not purposefully omit data to mislead the patient (
11). Clinicians should also point out to patients when objective data about risks and benefits of treatment are limited. This is often the case in treating patients during pregnancy because of the ethical limitations of conducting research with pregnant women.
2.
Decisional capacity. Decisional capacity is based on a person's ability to express a preference, understand relevant information, think through a choice in a way that is rational and deliberate, and make meaning of the decision and its consequences within the person's life (
11).
3.
Voluntarism. Voluntarism encompasses a person's ability to act in accordance with what is both true to and best for one's needs (
11).
In working through the informed consent process with patients, the psychiatrist is inevitably challenged to apply principles of medical ethics, particularly beneficence, nonmaleficence, autonomy, respect for persons, confidentiality, compassion, and veracity (
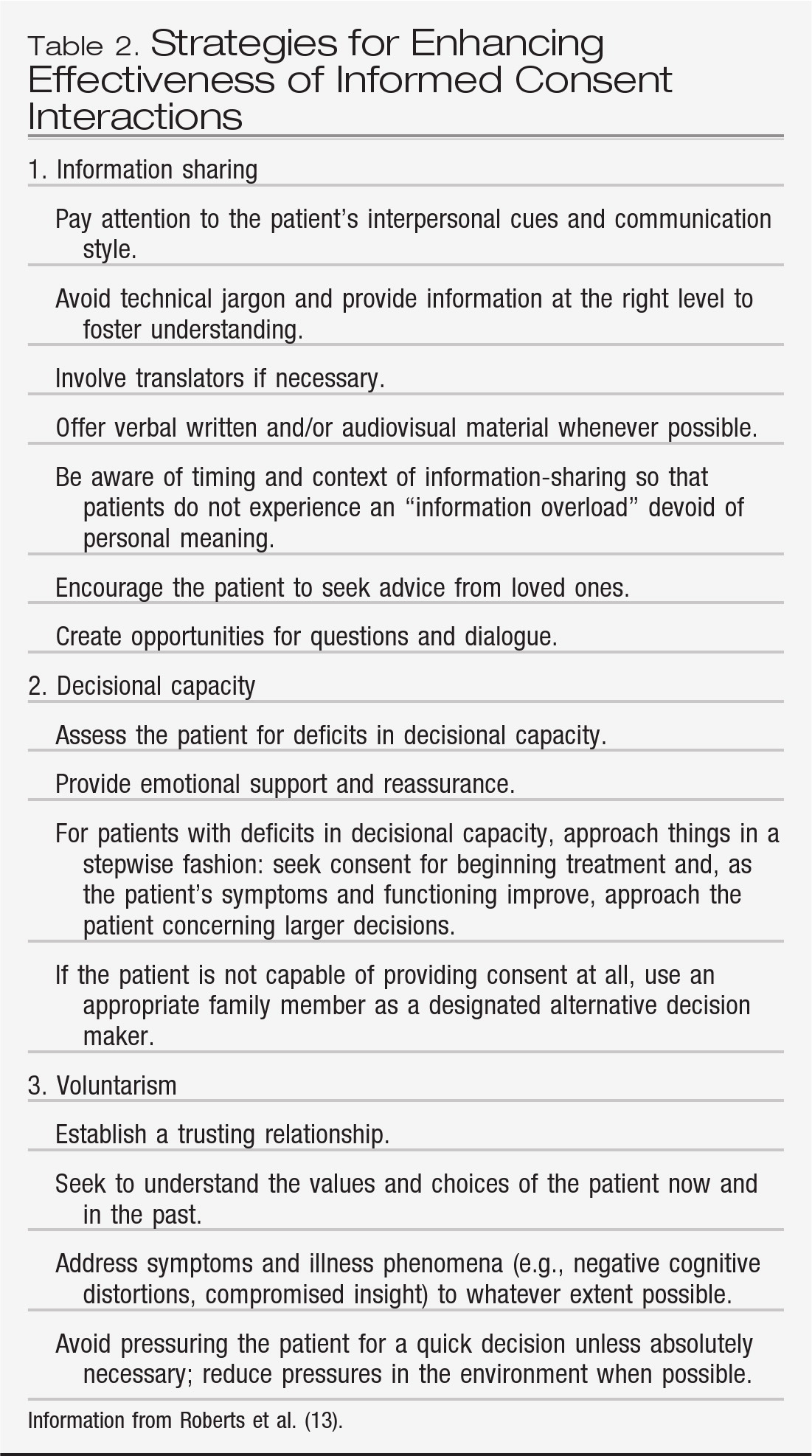
12). Specific strategies for enhancing the informed consent process can be helpful (
Table 2). The following case illustrates some ethical quandaries faced by mental health providers treating a woman with severe and persistent mental illness who is considering pregnancy.
Case 1
Mrs. A is a 30-year-old woman from Asia presenting to a mental health clinic with her husband to establish care. The couple is particularly interested in discussing the safety of psychotropic medication use during pregnancy. Mrs. A has been diagnosed previously with schizoaffective disorder and an unspecified disorder of developmental delay. She has been treated with an atypical antipsychotic at a subtherapeutic dose for the past 10 years, and her husband reports that it has been very helpful in managing difficult outbursts and chronic paranoia. For the past month, Mrs. A has refused to take the medication because she would like to get pregnant. She and her husband report that she has not been attending to her hygiene or eating as regularly since she stopped taking the medication. Mrs. A reports she is feeling increasingly “sad” and “lonely” and that she wants to have a baby to help her feel less lonely. She tells the psychiatrist that she will only take the medication if it is guaranteed to be safe during pregnancy.
The informed consent process is built upon the foundation of a therapeutic patient-doctor relationship. In this case, the relationship is relatively new and may pose challenges to the process of informed consent. The psychiatrist is aware that the patient is at risk of further psychiatric deterioration off medication and would have the additional risk of illness exacerbation that can occur postpartum. The psychiatrist may have concerns about whether Mrs. A can be a competent parent, given current concerns with self-care, and may be tempted to discourage pregnancy altogether. The psychiatrist may also have a negative countertransference to the patient's personal belief that having a child will help ease her feelings of loneliness. Concern for the patient's and future infant's well-being must be balanced with the ethical principles of respect for persons and autonomy, which hold that Mrs. A. has intrinsic value and therefore is entitled to pursue her own choices without prejudice. Nonetheless, the risks of medication discontinuation and postpartum mood exacerbation and the challenges of raising a child should be considered important information to share with the patient as part of the informed consent process. The psychiatrist may also consider treatment options for the patient to address her feelings of isolation, such as individual or group psychotherapy and parenting supports, which would probably benefit the patient and her family.
The psychiatrist informs Mrs. A and her husband of the risk for continued deterioration of her condition off medication and postpartum exacerbation and known and unknown risks associated with in utero exposure to atypical antipsychotics. The psychiatrist also discusses alternative medications and their risks, but when the psychiatrist suggests that there is not a guaranteed “safe” alternative medication during pregnancy, the patient becomes angry and accuses her husband and the psychiatrist of trying to prevent her from having a baby. The patient states that she no longer wishes to continue the appointment and leaves the room. She does allow her husband to remain and requests that he discuss the situation with her further in their native language when they return home.
At this point, the primary basis for the informed consent process—the therapeutic relationship—is compromised. Mrs. A either does not feel comfortable that the psychiatrist is working alongside her to further her own goals or is unable to tolerate the cognitive and emotional demands of the discussion as it has been presented to her. The psychiatrist may opt to spread out the discussion over several appointments to build trust and dispense information slowly, in a way Mrs. A can tolerate, and may also consider using an interpreter. Mrs. A has given her husband permission to gather information for her. Her capacity to fully participate in the informed consent process at this time may be compromised by a language barrier, cognitive limitations to process conflicting information (e.g., risks of continuing medication versus risks of discontinuing medication), emotional limitations to tolerate complicated decisions with unknowns, and psychiatric limitations brought upon by her worsening illness. In this case, her husband may be a reasonable partnered or alternative decision maker for both gathering information and making a final decision if the patient is unable to do so.
The psychiatrist completes the discussion of risks, benefits, and alternatives of psychotropic medication treatment during pregnancy with Mrs. A's husband, who supports Mrs. A's interest of pursuing a pregnancy but is concerned about her clinical deterioration off medication. He asks the psychiatrist to bring back Mrs. A and tell her that no risks are associated with medication use during pregnancy.
The psychiatrist may be tempted to simplify or overstate the safety of the medication to encourage the patient to continue taking it in support of the ethical principle of beneficence: to help the patient and to protect her from deterioration of her condition. However, the ethical principle of veracity suggests that every attempt should be made to clearly state the risks and benefits of the medication to both the patient and the potential fetus.
Mrs. A returns to the consultation room, and her husband and the psychiatrist together explain her treatment options during pregnancy allowing Mrs. A ample time to ask questions and express her understanding of the information provided. They decide not to make a final decision at this appointment. Mrs. A and her husband will return for a follow-up appointment, at which an interpreter will be present. In addition, the psychiatrist refers Mrs. A for individual counseling.
Conclusions
Treating women with mental illness in relation to reproduction can create numerous ethical tensions for the patient and the psychiatrist, often related to conflicting interests between the patient, child, and/or family members such as spouses. Guiding patients through decisions about treatment and family planning requires a steadfast commitment to the informed consent process. Such decisions are often complicated by limited information and by patient-specific capacities to manage the complexities of the information and consequent un-certainty. The psychiatrist plays a pivotal role in guiding patients through such complicated decisions.