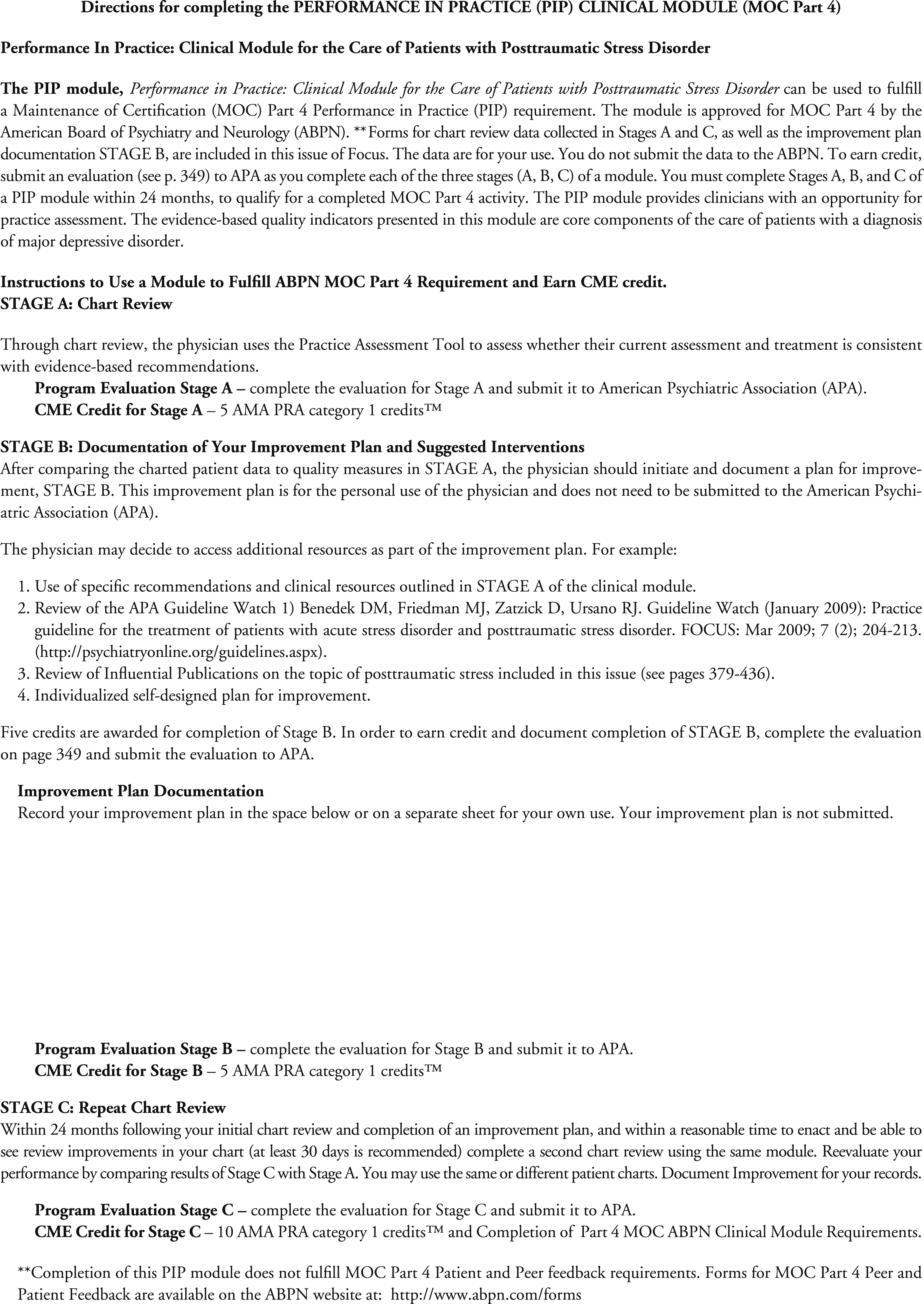
The American Psychiatric Association’s (APA) Performance in Practice (PIP) clinical modules are designed to meet the requirements of the American Board of Medical Specialties (ABMS) and American Board of Psychiatry and Neurology (ABPN) Part IV of Maintenance of Certification (MOC), which will be in full effect by 2017. Part IV of the MOC, Practice Performance Assessment, is intended to assist in physicians’ evaluation of the quality of care provided in their practice, compared with peers and national benchmarks, and to facilitate practice improvements through the incorporation of best evidence or consensus recommendations to improve patient care. Physicians are required to complete one PIP unit every 3 years. There are two components for each PIP unit: the Clinical Module, consisting of chart reviews of at least five patients in a specific category; and the Feedback Module, requiring collection of feedback surveys from at least five peers and five patients. The chart review displayed below is designed as a Clinical Module to facilitate physician practice assessment. The peer and patient feedback modules are beyond the scope of this report.
There are three stages involved in each PIP unit [ABPN 2013 – (
1)]:
•.
STAGE A, the baseline retrospective chart review of at least 5 patients in a specified category, which is then compared with “published best practices, practice guidelines or peer-based standards”
•.
STAGE B, the design and implementation of a clinical practice improvement plan
•.
STAGE C, subsequent remeasurement via a second chart review of 5 patients within the same category within 2 years after the initial chart review. Although the MOC program requires the review of at least five patients as part of each PIP unit, it is important to note that larger samples, i.e. reviews of more than 5 charts, will provide more accurate estimates of quality within a practice.
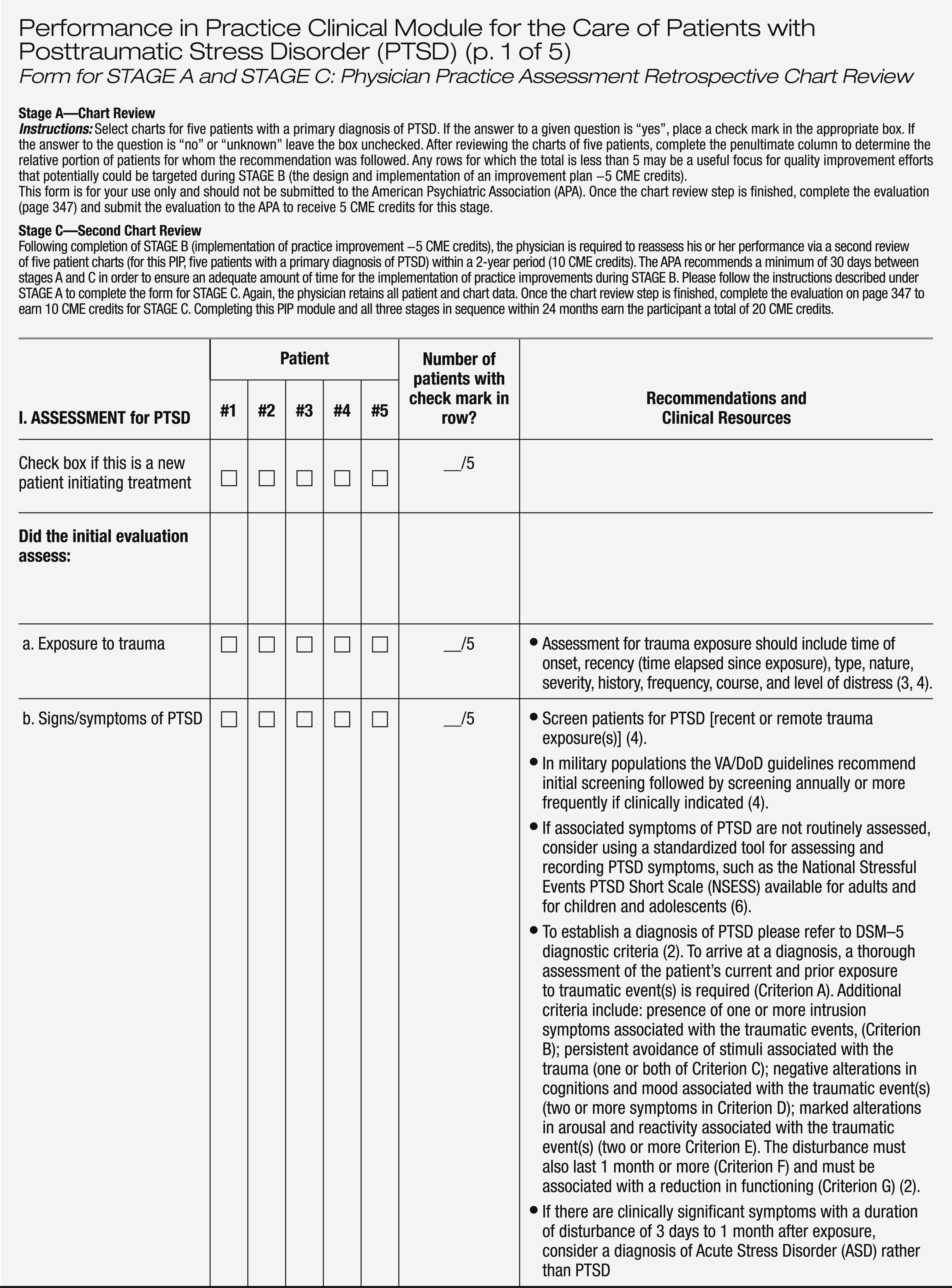
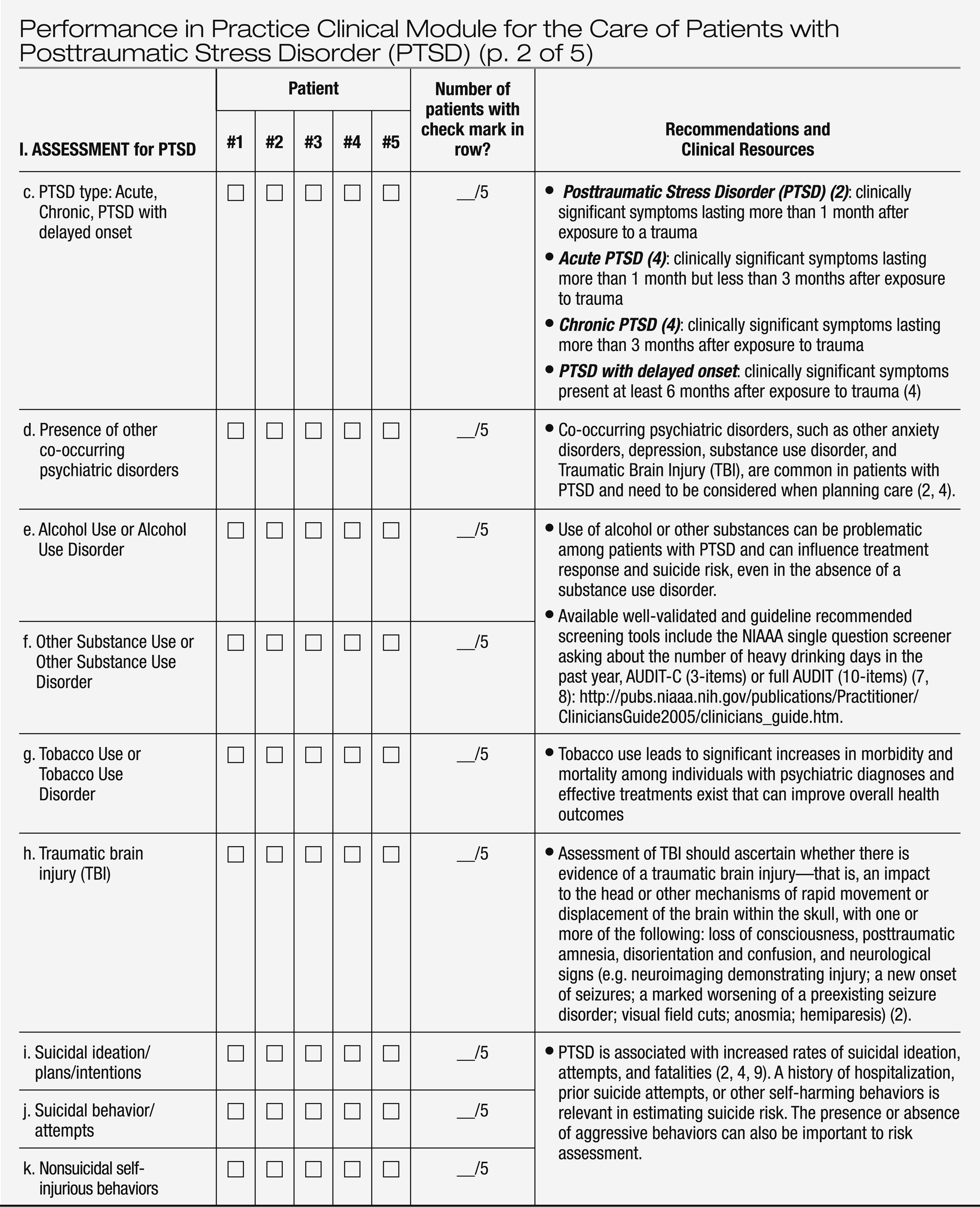
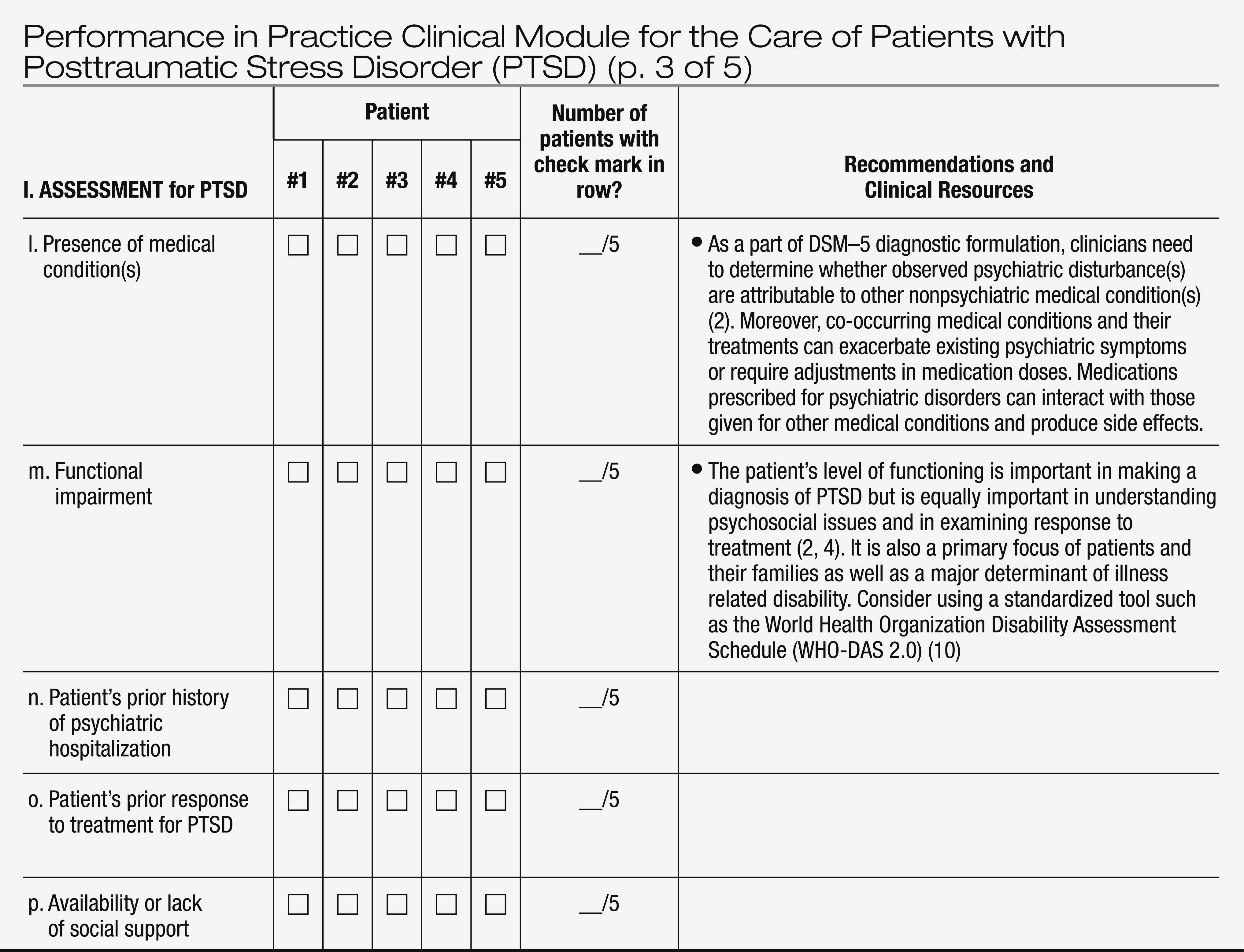
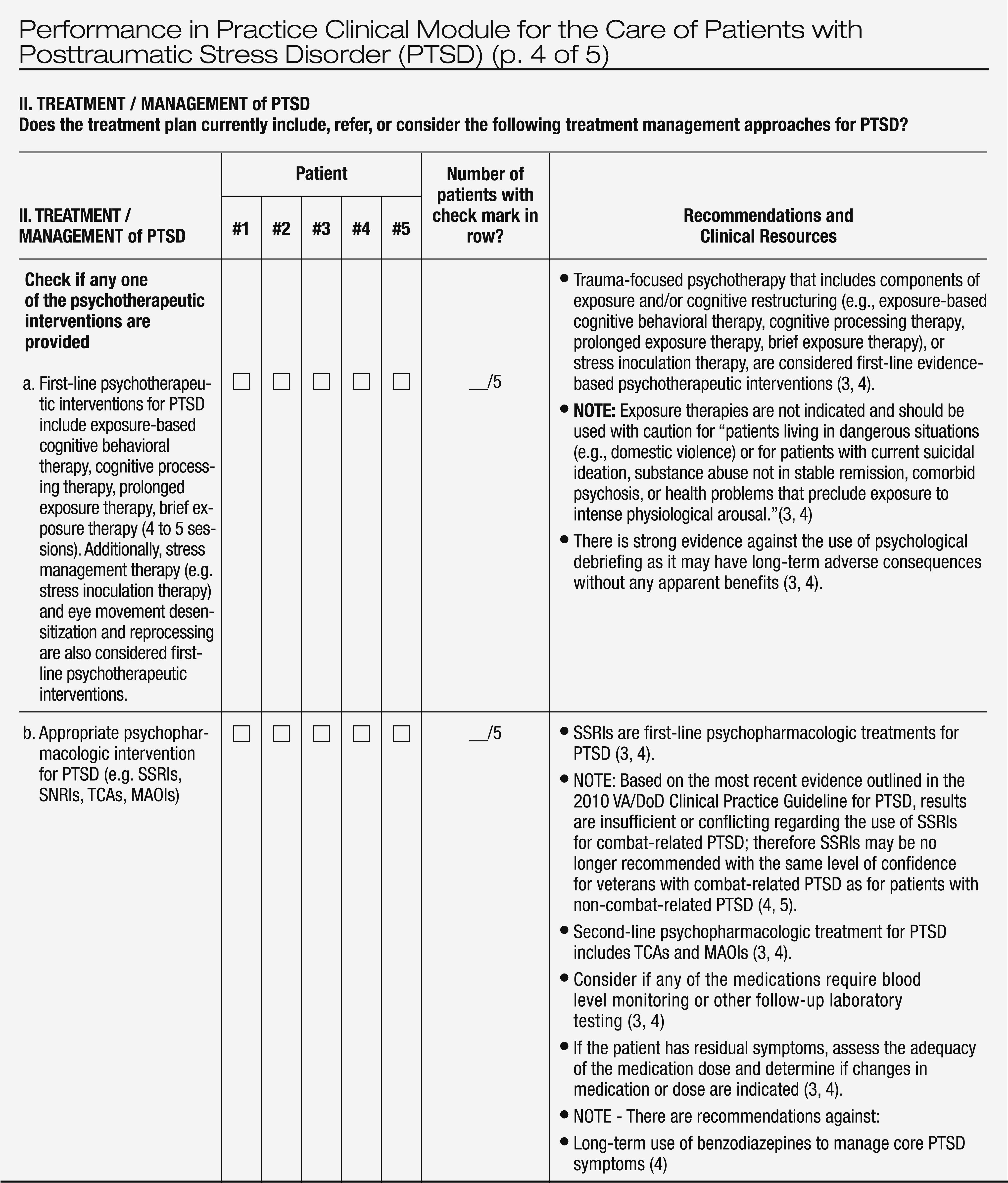
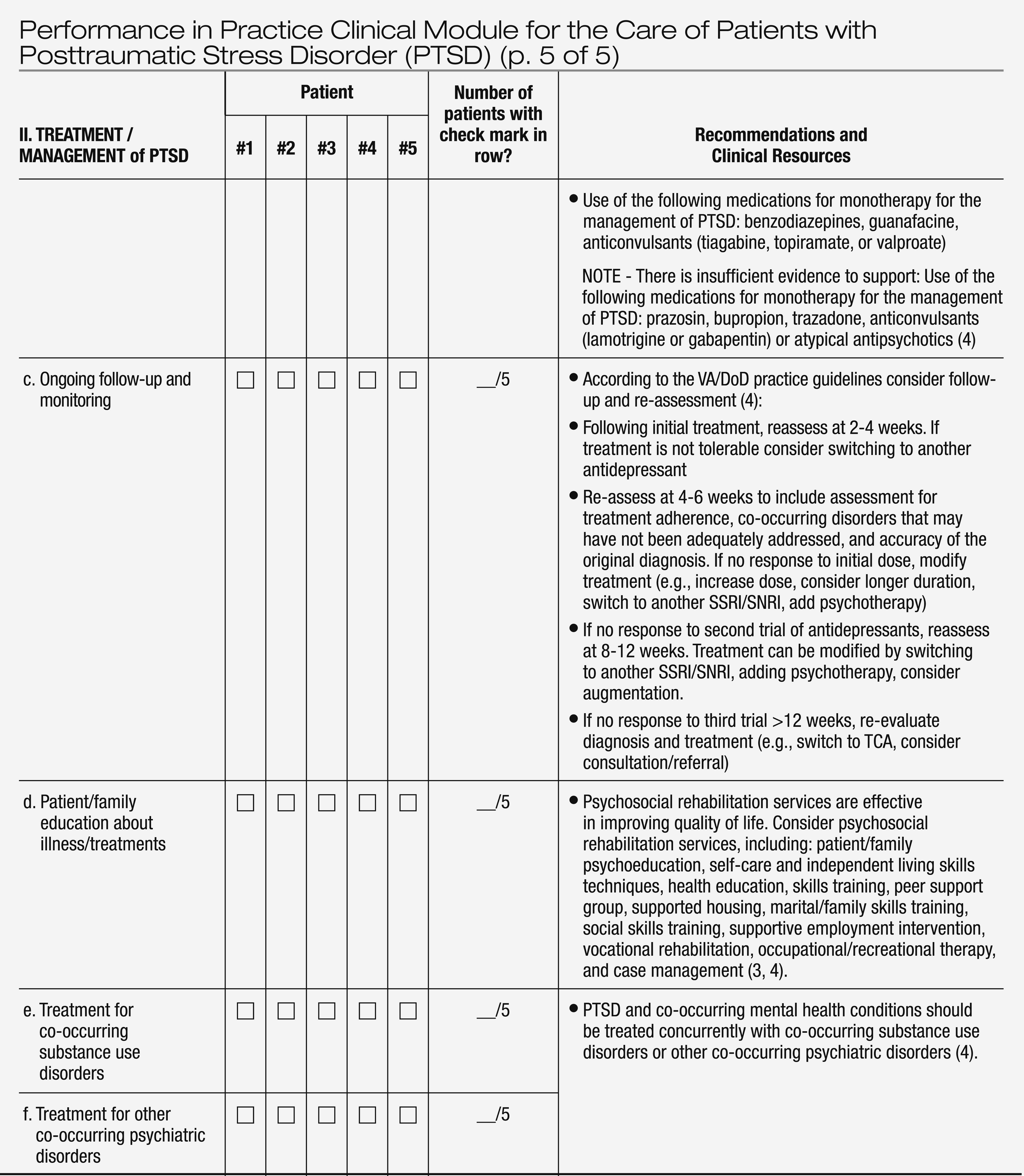
The PIP module presented in Table 1 provides STAGE A, retrospective chart review for the assessment of care given to patients who meet DSM−5 criteria for posttraumatic stress disorder (PTSD) or other trauma and stressor-related disorders (
2). The measures included in this module are based on recommendations of the 2004 APA Practice Guideline for the Treatment of Patients with Acute Stress Disorder and Posttraumatic Stress Disorder (
3), the 2010 U.S. Departments of Veterans Affairs and Defense (VA/DoD) Clinical Practice Guideline for the Management of Post-Traumatic Stress Disorder (
4), and the 2009 APA Guideline Watch for PTSD (
5). The selected practice guideline recommendations that are endorsed with moderate-to-substantial levels of clinical confidence (
3), and those endorsed at evidence-rating levels A and B (
4) have been highlighted in this module.
The PIP module for PTSD has been designed to be relevant across clinical settings (e.g. inpatient, outpatient), straightforward and easy to complete, and usable in a pen-and-paper format to aid adoption. As with other retrospective chart reviews, some questions on the form relate to the initial assessment and treatment of patients, whereas others relate to subsequent care. In general, treatment options for newly diagnosed patients who are being treated for the first time should judiciously follow the first-line evidence-based treatment recommendations. On occasion, however, there may be appropriate clinical reasons for deviation from recommended care, including patient preferences, co-occurring psychiatric or medical conditions and therapeutic benefits or side effects of prior treatments.