Case Vignette
Barbara is a 46-year-old biracial female (African-American mother and Caucasian father) who was referred to you by her oncologist after “depression,” “memory issues,” and other problems emerged following the diagnosis and initial treatment for breast cancer.
She reported to you that she first found a lump in her left breast through breast-self-exam about 15 months ago; she had performed BSE and had had periodic mammography “religiously” because a maternal aunt had died from breast cancer when Barbara was a child and her primary care physician had informed her that she may be at elevated risk. As part of the work-up at the time of diagnosis, she had undergone lumpectomy and lymph node dissection; this revealed that the neoplasm had spread to one node. She subsequently had local radiation therapy and systemic chemotherapy and completed her last cycle about 6 months ago.
She reported that hearing the diagnosis was “probably the most stressful thing” she had endured as an adult. Her husband and her 20- and 18-year-old daughters had been both distraught and supportive, per her report. Her husband was able to take time off from his work and her daughters had taken turns coming home from college on the weekends to help her whenever she had a chemotherapy cycle, because she felt “totally wiped out” for about a week after each cycle. She found that some friends “really came together” to support her. Things had not been as great at the small nonprofit where she had worked as Director of Programs; they had given her the maximum amount of time under FMLA but when she tried to return to work, she found that her mind was “foggy” and that she was making errors in executing her daily tasks. On one particularly challenging day, she reported that she had a “melt-down” at work when she realized that she had failed to complete the payroll filing correctly (none of her staff would get their paycheck on-time that month) and dissolved in tears. She and the group’s Executive Director agreed that she should “take some time out on disability” to try to “get things back together” and that was what led her to seek referral to you from her oncologist.
You asked her about specific symptoms, and she endorsed a chief complaint of “my mind is not working right,” by which she meant difficulties with memory, organization, planning, and decision making. “My brain’s not firing on all cylinders.” While this had been most apparent in the workplace, she acknowledged that she had been having trouble at home as well; for example, her elder daughter was in her final year of college and had been accepted into medical school, so Barbara had wanted to arrange a special celebration, but had found the complexities of planning to be too much for her. In daily matters, her husband has taken the lead in planning most of the tasks needed to keep the household running, a role she had previously performed before becoming ill. She reported feeling deeply sad, with moments where she will burst into tears “for no good reason.” She reported that she has “not had a good night’s sleep in I don’t know how long,” with difficulties falling asleep, staying asleep, and awakening “like I’ve got an alarm clock in my head” at 4 a.m. most days. She endorsed pronounced fatigue, loss of appetite with weight loss confounded with the chemotherapy side effects, feeling tense, and some psychomotor agitation. She reported that she thought a lot about death and how it would impact her family if she were to die, adding “I don’t know how much time I have…there’s so much I want to be here for, and it makes me angry that I might not be around to see my daughter become a doctor, or to grow old with my husband – it’s not fair.” She adamantly denied any thoughts of suicide or self-injury. She said that she still enjoyed activities and friends, but with a melancholy tinge because “I never know if this might be the last time.”
Consideration Point A
At this point in the patient’s history, your differential diagnosis includes
| A.1_____ | Major depressive disorder, single-episode |
| A.2_____ | Adjustment disorder, related to breast cancer |
| A.3_____ | Bipolar disorder, depressed phase |
| A.4_____ | Cognitive disorder NOS |
| A.5_____ | Substance-induced mood disorder |
Vignette Continues
You explored any past episodes of mood or anxiety disorders, and the patient reported that she had been doing well until the diagnosis and treatment for breast cancer. You inquired about any past treatments from her PCP, to which she responded with anger “that pompous idiot – when I first found the lump, the first thing he told me ‘first you must mourn for yourself’ even before I had the biopsy and knew it was cancer. I still have nightmares about him and then about having that biopsy – my heart stopped from some reaction to a medication during the procedure and they nearly lost me in the operating room! Whenever I was back at the medical center for my outpatient chemo, I took the long way from the parking lot to the chemo center so I wouldn’t have to go anywhere near that surgery area.”
As you inquired more about the patient’s history, she denied any prior times with experiences of depressive, manic or hypomanic symptoms, obsessive thoughts or compulsive behaviors, hallucinatory experiences, or delusional thoughts.
As you inquired about her early life history, you learn that the patient’s childhood was marked by a close-knit family of origin in which she was the middle of three children (older sister and younger brother). She recalled being close to her grandparents and to her mother’s sister, the aunt who died from breast cancer when Barbara was 10 years old. She recalled some challenges being one of the few biracial children in the first school she attended, but said that things got better when her family moved and she attended a new school where she felt accepted and supported. She did well in high school and college, earning a B.A. in history and a master’s degree in public administration. Socially, she and her husband have been married for 22 years and have two daughters. She is active in their church, and she had been active in the PTA before her children went to college. She had worked until taking time off for her medical treatments and then returning before the “melt-down” incident noted earlier.
The patient reported never using drugs of abuse or smoking tobacco. She reported occasional consumption of wine, estimated as one glass of wine over dinner with her husband, roughly 3 nights out of the week.
In reviewing her medical history, the patient denied having major medical conditions other than breast cancer. When you evaluated her, she reported taking no routine prescription medications but did endorse taking a set of vitamin supplements and some herbal products she got from a herbalist she was introduced to by friends from her yoga class.
On examination, she was pleasant and cooperative with the interview, neatly attired in casual slacks and blouse, and with very short-cropped hair (a style she’d adopted since her chemo-induced hair loss). There was mild psychomotor agitation noted. Eye contact was adequate, with occasional tearfulness (related to her fears of foreshortened future). Speech was of slowed rate and hypophonic volume, but normal prosody. Affect was constricted and unhappy. Mood was endorsed as sad and worried. Thought process was slowed, generally linear and coherent, but at times with more difficulty following the conversation than you expected given her educational and occupational background. Thought content was without hallucinations, delusions, or current suicidal or homicidal intent. Cognitively she was awake, alert, and oriented to self, place, date, and circumstances. Memory registration was intact with 3/3 stimuli, and recall after delay was 2/3 items but after a painfully slow delay. Recalling recent U.S. Presidents was a challenge; she could name Obama and Bush but could not recall Clinton even with clues. Some similarities were concrete (chair/table = “things you find in the dining room”) while others were more abstract (apple/orange = “fruit;” watch/ruler = “measurement tools”). Insight was adequate, in that she recognized she was not doing well and needed mental health care. Judgment currently was adequate, in that she was open to considering all options for treatment. Neurologically, gait stride length was normal, as were arm swing and turning, and rapidly-alternating movements. You detected no focal neurological deficits. Her score on the self-rated PHQ-9 instrument was 17, in the moderately severe range, with endorsement of the “nearly every day” response (3 points) for sleep, energy, concentration, and self-critical items.
Consideration Point B
At this point, the treatment options you consider with this patient include which of the following
| B.1_____ | Start a sedating antidepressant and have her return in 2 weeks |
| B.2_____ | Refer her for psychotherapy |
| B.3_____ | Continue to monitor the patient for another 4 weeks without an intervention |
| B.4_____ | Start an anticonvulsant mood-stabilizing agent and have her return in 2 weeks. |
Vignette Continues
After discussion of the options for treatment, the patient accepted your recommendation to start with treatment with a low dose of a sedating antidepressant to address her sleep and mood symptoms. She wished to wait on the psychotherapy option: “I don’t have the energy to talk just now.”
She returned after 2 weeks, reporting that her energy and outlook on life were much better; while she could fall asleep more easily, she was still awakening most nights. She described that she awakened with nightmares about her experiences early in her treatment for breast cancer.
Consideration Point C
Given all the details of the case, your next therapeutic step(s) is/are
| C.1_____ | Increase the dose of the antidepressant as tolerated |
| C.2_____ | Start prazosin |
| C.3_____ | Start an atypical antipsychotic agent |
| C.4_____ | Start a psychostimulant agent |
Vignette Concludes
The patient agreed to increasing the antidepressant dose and adding prazosin. She returned in another 2 weeks with further symptom improvement in sleep (far fewer nightmares; fewer early morning awakenings), energy, outlook on the future, and tension. She reported that she was still having difficulties with decision making and “keeping track of a million little details.” She accepted your recommendation to start a trial of a psychostimulant.
She returned 2 weeks later. Her PHQ-9 had fallen to 3 (2 points for the cognition question and 1 point for sleep). She reported that she had more “zip” and that she could make decisions faster, but that she still was having some memory issues and would forget things that then made her frustrated with herself. She still avoided the surgical wing of the medical center, but reported feeling “less freaked out” when near it.
The possibility of “chemo brain” remained on your problem list. Because of the cardiac arrest and resuscitation, you were also suspicious of a potential anoxic brain insult, and ordered an MRI scan to detect possible ischemic damage, because that may moderate the expectations you and the patient may entertain for possible improvement. You and she discussed referral to a neuropsychologist for more extensive cognitive testing, now that her depression was in remission and PTSD symptoms were better contained, and were less likely to confound detection of other cognitive disturbances.
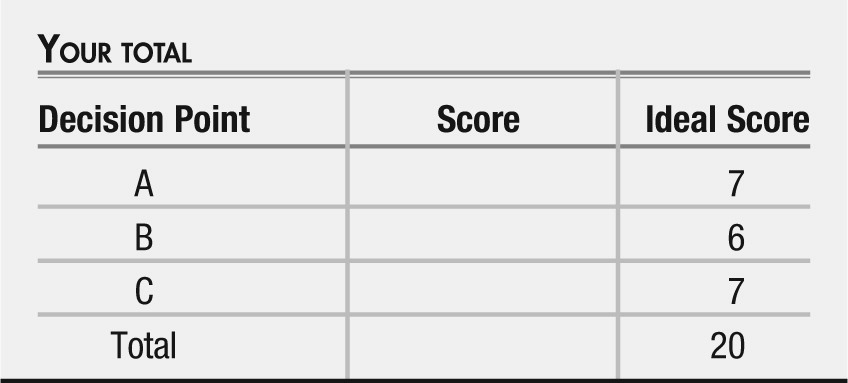
Answers: Scoring, Relative Weights, and Comments
Consideration Point A
| A.1_____ | (+3) Major depressive disorder, single episode. The patient has endorsed symptoms consistent with the DSM criteria for major depressive disorder and has no past history of prior episodes (1). |
| A.2_____ | (0) Adjustment disorder, related to medical illness. This patient has experienced a set of stressful circumstances related to the diagnosis of cancer, but that occurred over a year ago. Given the range of symptoms and impairments, and their duration, major depression is probably a more parsimonious characterization (1). |
| A.3_____ | (+1) Bipolar disorder, depressed phase. While you do not have evidence of manic or hypomanic symptoms in the past, it is premature to exclude this diagnosis until you have specifically ruled-out a past history of mood elevation and related symptoms (1). |
| A.4_____ | (+2) Cognitive disorder NOS. The patient has prominent cognitive symptoms that resulted in her taking a leave from work, but whether this is a part of a mood disorder or an independent condition is not yet clear (1). |
| A.5_____ | (+1) Substance-induced mood disorder. Overt or covert substance use can lead to mood problems, either in intoxicated or withdrawal states (e.g. psychostimulants, alcohol), and always merits some consideration since it can occur covertly in otherwise seemingly “upstanding citizens” (1). While you have no specific data to support this diagnosis at this point in the narrative, collecting more history will be important to help rule this out. |
Consideration Point B
| B.1_____ | (+3) Start a sedating antidepressant and return in 2 weeks. An antidepressant choice can target sleep symptoms as well as other major depressive disorder symptoms. The dose of the medication should be selected to be consistent with evidence-based practice guidelines (2). |
| B.2_____ | (+3) Refer her for psychotherapy. Several forms of psychotherapy are evidence-based practices for depression (2) |
| B.3_____ | (−2) Continue to monitor and return in 4 weeks. In a patient with clear symptom burden and disability, more active management and more frequent follow-up would be consonant with evidence-based practice (2) |
| B.4_____ | (−2) Start an anticonvulsant mood-stabilizing agent and have her return in 2 weeks. While the use of anticonvulsant mood-stabilizing agents in bipolar depression is supported by the evidence base (3), there is no evidence of bipolar disorder in this patient’s past or present. |
Consideration Point C
| C.1_____ | (+3) Increase the dose of the antidepressant as tolerated. Dose optimization is an evidence-based practice in MDD (2). |
| C.2_____ | (+2) Start prazosin to target the nightmares. Research with this agent has shown that it can be effective in some patients in addressing the nightmares of posttraumatic stress disorder (an off-label use) (4). The patient exhibits nightmares, a foreshortened sense of her future, and avoidance symptoms, all arising after her near-death experience during her biopsy procedure, all of which can be evidence of PTSD (1, 5). Patients can develop PTSD from medical procedures intended to help them but which are painful, frightening, and life-threatening themselves (6). This response is weighted “2” because the evidence is not as strong as for item C.1. |
| C.3_____ | (−2) Start an atypical antipsychotic agent. Dose optimization of an antidepressant agent should precede adding a second agent for major depressive disorder (2). When a large trial of an atypical antipsychotic agent (risperidone) found that it was no better than placebo for PTSD symptoms (7), the routine use of atypical antipsychotic medications was removed from the VA standards for PTSD. |
| C.4_____ | (+2) Start a psychostimulant agent. Psychostimulant medications that are approved for ADHD treatment are sometimes used off-label to help with fatigue in cancer (8) and also with cognition in patients with cognitive symptoms related to medical illnesses (9, 10). Since this was her chief complaint, her degree of impairment may decrease with this addition. This response is weighted “2” because the evidence is not as strong as for item C.1. |