Management of Complex Co-occurring Psychiatric Disorders and High-Risk Behaviors in Adolescence
Abstract
Clinical Context
Background
High-Risk Behaviors
Substance Use
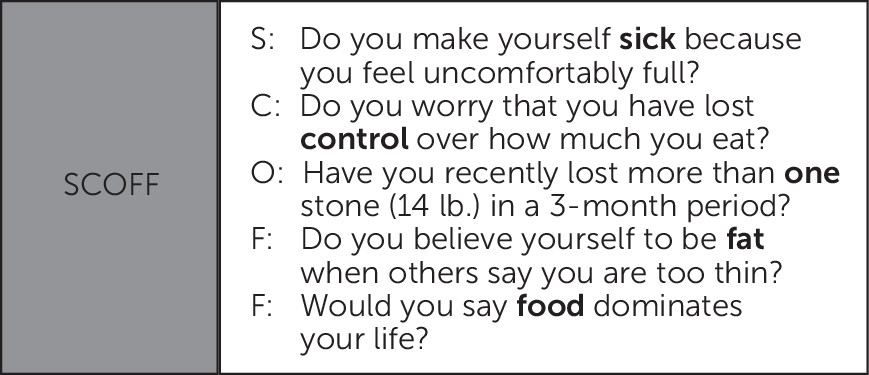
Disordered Eating
Sexual Behaviors
Suicide and Self-Harm
| Risk factor for suicidal ideation | Risk factors for suicide attempts | Risk factors for suicide completion |
|---|---|---|
| Presence of a mood disorder | Suicidal ideationb | Firearms in the homeb |
| Self-harm | Self-harmb | |
| Hopelessness | Substance use (including cannabis use)b | |
| Minority sexual or gender status | Environmental exposure to self-harm | |
| Psychosis | Family history of suicide | |
| Males | Suicide capabilityb | |
| Media exposure to suicide | Impulsivity | |
| Bullying (victim or perpetrator) | Excessive use of internet or social media | |
| Excessive use of internet or social media | ||
| Parental mental illness |
Treatment Strategies and Evidence
Assessment
Treatment Approaches
Suicide and Self-Harm
Substance Use
Disordered Eating
Sexual Behaviors
Questions and Controversy
Prescribing Antidepressants for Youths With Depression and Risk of Suicidality
Use of Off-Label Antipsychotics for Youths
Use of Mood Stabilizers for Youths
Case Discussion
Recommendations
Screen for Co-occurring Disorders
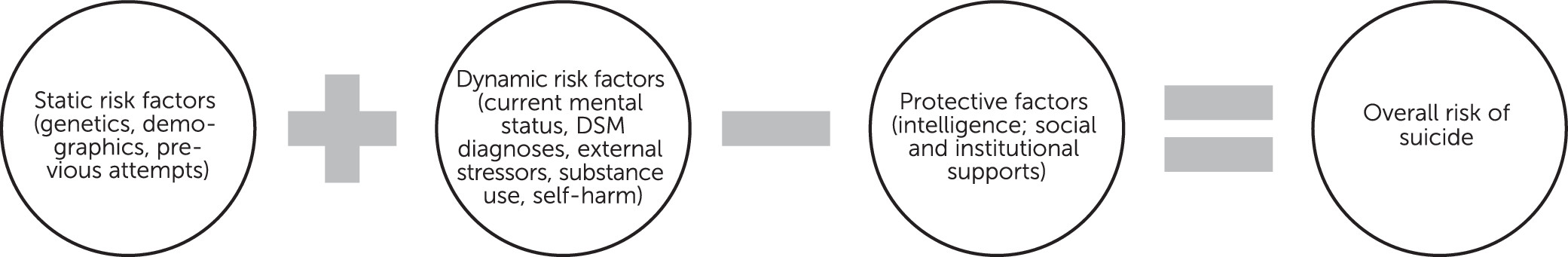
Understand Dynamic and Static Risk Factors for Youth Suicide
Reduce Access to Means for Suicide Completion
Monitor Social Media Usage by Youths at Risk for Suicide
Treat Mood Symptoms and Substance Use Concurrently
Create Treatment Teams and Psychoeducational Practices for Patients With Disordered Eating
Offer Sexual Health Psychoeducation and Regular STI Screening to Adolescents
Future Directions
References
Information & Authors
Information
Published In
History
Keywords
Authors
Competing Interests
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBLogin options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).