Dandy-Walker complex (DWC) was first described by Dandy and Blackfan in 1914; however, the exact description of the characteristic features, by Hart et al.,
1 did not occur until 1972. The Dandy-Walker complex is a rare posterior-fossa malformation, usually observed during the prenatal period or early infancy. It is characterized by hypoplasia or agenesis of the vermis, enlargement of the fourth ventricle in continuity with a posterior fossa cyst, and usually, although not exclusively, hydrocephalus.
2The etiology is not yet clearly defined. Genetically, there is a frequent association with trisomies on 3q, 6p, 9p, as well as chromosomal translocations. More crucial is the apparent correlation of the malformation with two coupled genes, ZIC1 and ZIC4, which are involved in the formation of the cerebellum. Mice with heterozygous deletions of these two linked genes have a phenotype that closely resembles the Dandy-Walker malformation (DWM).
1 DWM is thought to develop between the 7th and the 10th week of gestation; early descriptions of the syndrome propose that the main pathogenic mechanism was the failure of the foramen of Magendie and Luschka to open through embryonic life, specifically at the end of the 4th fetal month.
1,3Previous research postulates that a cystic malformation in the posterior fossa due to the defective assimilation of the area membranacea anterior within the tela choridea produces secondary abnormalities in cerebellar structures, while the foramen of Magendie remains patent. Various predisposing factors have been reported, such as infection, cranial trauma, chronically disturbed cerebrospinal fluid pressure, persistence of embryonic vestige, vascular lesions, teratogenesis, and maternal diabetes.
2Based on the type or severity of neurodevelopmental abnormalities, three main types of DWC have been identified: DWM, which is characterized by an enlargement of the posterior fossa, large cystic dilatation of the fourth ventricle, total or partial agenesis of the vermis, and a highly-positioned tentorium with elevated straight sinus; Dandy Walker variant (DWV), which includes a cystic dilatation of the fourth ventricle and hypoplasia of the inferior portion of the vermis without enlargement of the posterior fossa; and Mega Cysterna Magna, where the compressive atrophy of the vermis is associated with cystic enlargement of the cisterna magna, communicating freely across the foramen of Luschka and Magendie with the fourth ventricle and subarachnoid space.
2The severity of the symptoms depends on the extent of the above-described three main features of the DWC. Affected patients generally present with developmental motor delays; signs of increased intracranial pressure, including irritability; and signs of cerebellar dysfunction, including ataxia, decreased muscle coordination, hypotonia, and nystagmus.
2 Hydrocephalus is the most common symptom and is found in approximately 90% of cases; consequences of this increased intracranial pressure lead to additional symptoms, such as vomiting, lethargy, and abnormal enlargement of the head. Also, it may manifest with mental retardation, hearing and/or visual difficulties, poor fine motor control, spasticity, and seizures. DWC may also be asymptomatic. Additional neurodevelopmental issues, including agenesis of the corpus callosum, lissencephaly, and cortical dysplasia, can affect the severity of the above symptoms, as well.
1The relationship of DWV and psychosis has not been well studied in the literature, possibly because of the rarity of this condition. A few case reports have hypothesized a relationship between psychosis and DWV; however, these were all reported in adult patients, with only one reference to pediatric psychiatric conditions, as noted by Sasaki et al.
4 We report here psychotic symptoms in an adolescent patient with DWV.
Case Report
A 14-year-old Asian adopted girl with no previous psychiatric history was brought for outpatient psychiatric evaluation to assess “paranoid ideas and her misperception of reality.” She had been attending a summer camp when she developed acute feelings of severe anxiety. She reported having a headache, “feeling faint” with tingling and numbness in her arms,” and feeling “cold and clammy.” These symptoms lasted for a few minutes and she reported feelings of impending doom. She could not relate a precipitating event to these symptoms and reported that the ominous feelings persisted after the physical symptoms subsided. She became preoccupied that “bad things were going to happen.”
She was assessed by her pediatrician, who noted elevated heart rate but normal electrocardiogram and laboratory work-up. Several days after this initial complaint, the child reported to her parents that the faces of her friends were “colored red,” and she reported feelings of paranoia regarding people staring at her. Her pediatrician referred her to a child psychiatrist, who initiated a trial of risperidone, titrated up to an oral dose of 2.25 mg daily.
During the titration period, she continued to express paranoid ideation that people were hiding behind trees to spy on her and that her parents were going to kidnap her. She expressed to her parents that she heard a voice talking about a dead body and referenced that she understood this to mean that she was going to die or should die. She expressed fears that the police had come into her home and “moved words around in magazines” and had plans to arrest her for viewing internet pornography. She admitted that she had been viewing pornographic material, which she originally disguised as “health issue websites” for over a year and felt an enormous amount of guilt over this. Her mother described her thought-process as “loose and disconnected.” She admitted to feelings of racing thoughts, difficulty concentrating, excessive worry, and difficulty falling asleep secondary to this. She also expressed ideas of reference that patients in the waiting room of her appointments were all there because of her. She also had thoughts of self-doubt and low self-esteem. She denied use of drugs, alcohol, or tobacco; denied suicidal or homicidal ideations, and was able to articulate her paranoid ideations. She was referred for a more comprehensive psychiatric evaluation and psychological testing.
The child was adopted at the age of 2 from an Asian orphanage; she weighed only 17 pounds at the time of adoption and was delayed with regard to developmental milestones; however, with proper care, nutrition, and support, she was able to recover fully and continued to reach subsequent milestones at the appropriate ages. Her menses started at age 13. No family history is available for her; her adopted sister, also from Asia, is of no biological relation.
On initial interview with the current psychiatrist, she was quiet, shy, appeared younger than stated age, was well-groomed, and wearing appropriate clothing. She was cooperative, with normal speech and fair eye contact. She had no trouble separating from her parents, but did appear slightly anxious at times. Her affect was blunted, and she repeated that her mood and thoughts were “much better” with the medication. She admitted to previous feelings of agitation and anxiety. She endorsed feelings of sadness, decreased concentration, increased “thinking;” she denied hopelessness or helplessness, admitted to auditory hallucinations as previously noted; denied thought-broadcasting or thought-insertion. She endorsed difficulty with sleep, specifically, trouble falling asleep and early awakening. Her insight was fair, and her judgment was impaired. She exhibited low self-esteem and overwhelming guilt regarding her internet activities and believed that she needed to be punished. Review of her personal journal entries exhibited mood-congruent beliefs of self-reproach, guilt, poor self-esteem, and paranoid thinking. She was referred to a psychologist for psychological testing, with the following results:
Carroll Depression Rating Scale
The patient had a total score of 12.
5 Scores above 10 are consistent with clinically significant depression.
Kaufman Brief Intelligence Test
The patient had a verbal score of 98, nonverbal score of 94, composite score of 96, estimated to perform better than 45% of children her age.
6Bender Gestalt II
Her scores fell in the above-average range. She performed better on copying figures than on drawing from memory (copying score was greater than 94%, and recall score was greater than 72%, as compared with individuals in her age category).
7Millon Adolescent Clinical Inventory
The patient exhibited a personality characterized by dependency and social inhibition, motivated by feelings of insecurity and inadequacy. It is believed that adolescents with this personality type have learned to find security in others, as they believe they are unable to meet their own needs or ensure their own safety; they have adopted passive roles and avoid their own emotions to avoid rejection or abandonment and suppress their own emotional reactions to avoid disappointing or causing negative reactions in others.
8An electroencephalogram (EEG) was performed and showed normal results during wakefulness, with persistent eye-blinks and muscle artifact which, however, did not significantly obscure the recording. There was a significant amount of beta activity, suggesting sedative medication effects. No epileptiform features were noted. Laboratory data, including screening for autoimmune diseases such as lupus, and complement DNA antibodies; all were negative. Thyroid-function tests, rheumatoid factor, cardiolipin antibodies, immunoglobulin-G, immunoglobulin-M, immunoglobulin-A, Lyme disease titers, and Epstein-Barr virus titers were all negative as well. Erythrocyte Sedimentation Rate and vitamin B12 levels were normal.
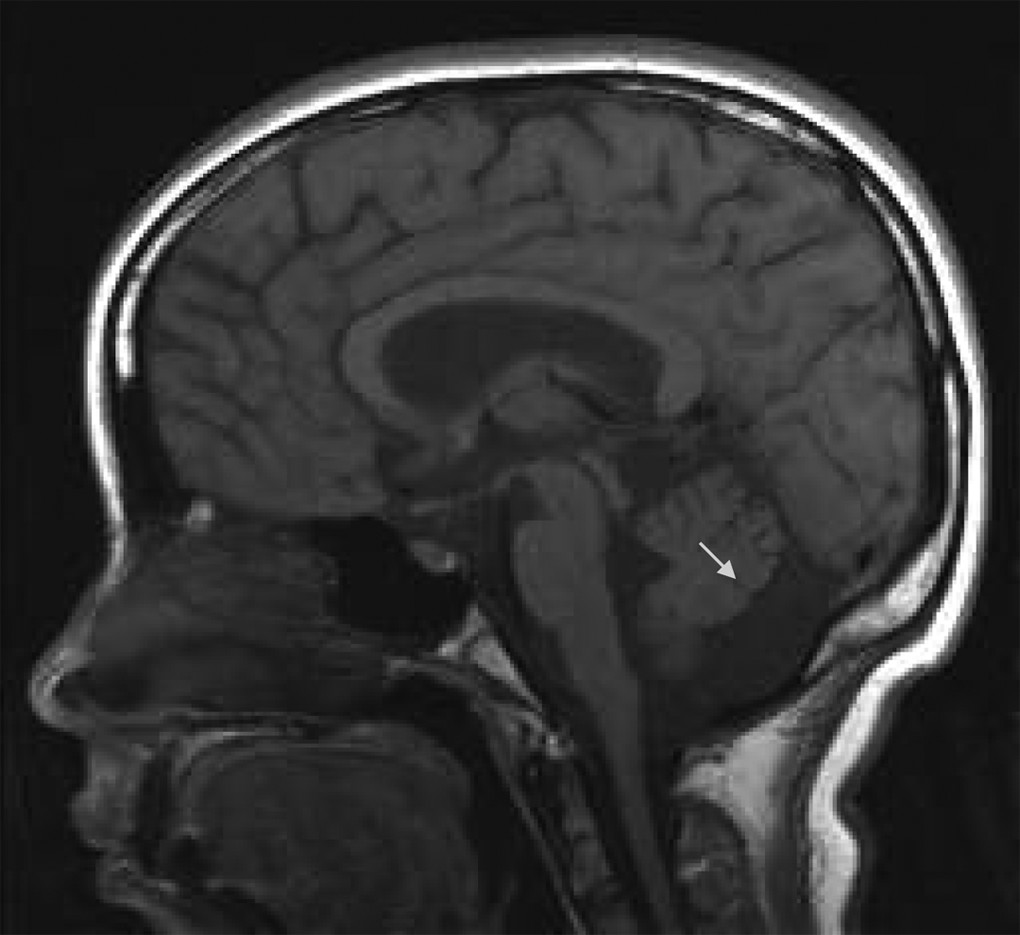
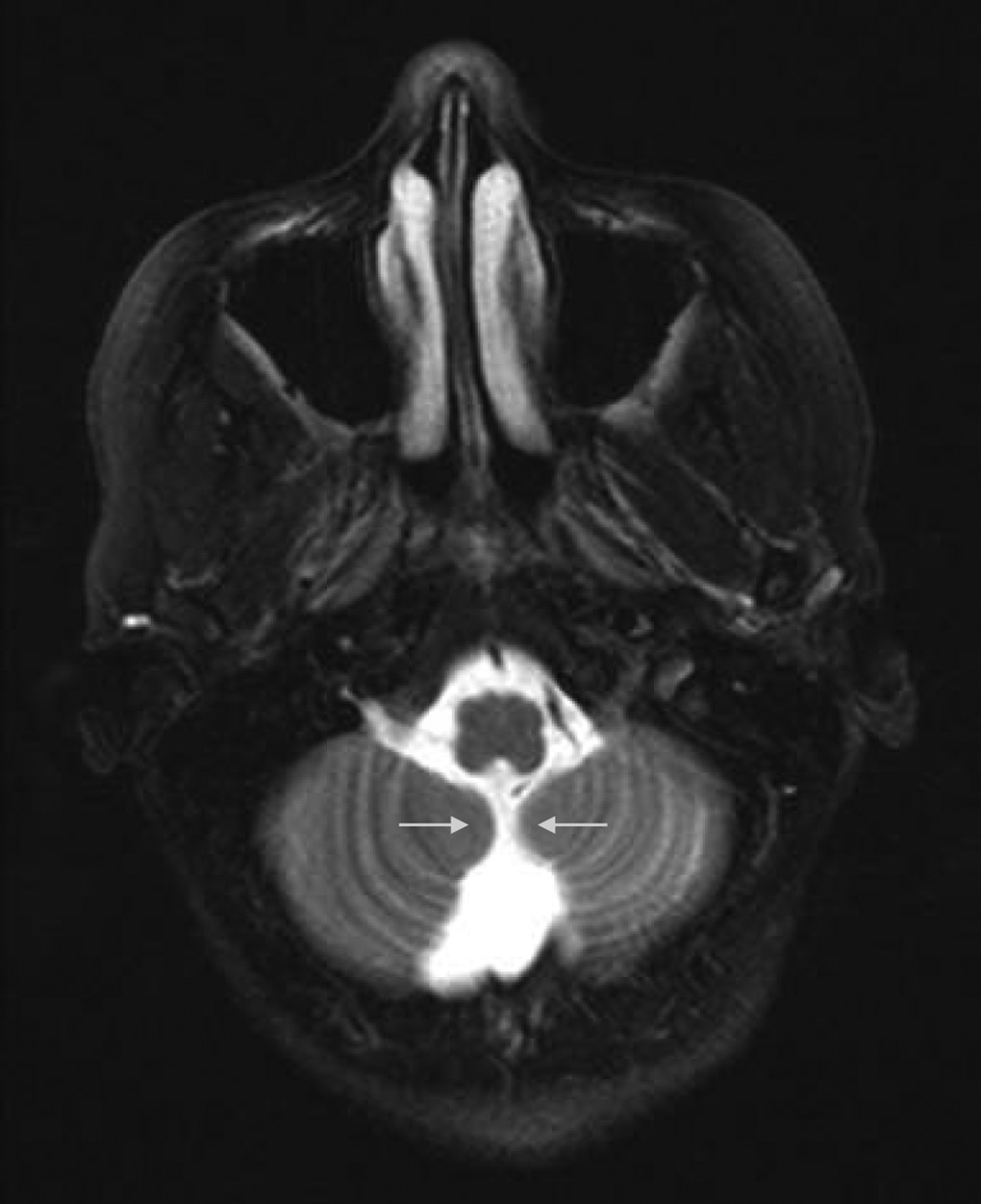
MRI (see
Figure 1) showed ventricular size to be at the upper limits of normal or mildly dilated for age. There was prominence of basilar cisterns and a prominent cerebral spinal fluid space dorsal and inferior
1 to the cerebellum (
Figure 2), suggestive of a mild form of DWV. There was no intracranial hemorrhage, edema, or mass effect and no abnormally restricted diffusion.
During the first few weeks of treatment, a trial of escitalopram was initiated but was rapidly discontinued secondary to side effects. There were no further complaints of depression or sadness. Subsequently, during a 10-month follow-up period, the child and family reported complete resolution of the psychotic symptoms while she was being treated with risperidone 1.75 mg–2 mg daily, stating that she exhibited no paranoia, hallucinations, or psychotic symptoms. She denied any issues with sleep, appetite, guilt, or energy during this time. On two separate occasions, however, when the dose of the antipsychotic was lowered to 1.5 mg–1.6 mg per day, her symptoms returned. During her symptom-free months, she completed the Kovacs’ Children’s Depression Inventory, with a total score of 4.
9 Retrospective analysis of how she felt while exhibiting psychotic symptoms produced a score of 10, with significant scoring in the areas of negative mood and anhedonia.
Biweekly psychotherapy sessions were initiated with this patient and her family to further decrease what presented as persistent symptoms of depressed mood. These symptoms appeared to be characterized primarily by negative views of self and a strong need for acceptance, challenged by underdeveloped interpersonal skills. A cognitive-behavioral psychotherapeutic approach served as the basis for her treatment, with the primary goal of helping her develop both cognitive and behavioral protective factors against recurring symptoms.
Cognitive-restructuring techniques were focused on modifying the maladaptive automatic thought process that directly affected her emotions and unnecessarily reinforced negative beliefs about herself and others. Behavioral techniques (i.e., problem-solving and social-skills training) were used to further help her more effectively interact socially with others while learning to better manage potential challenges that present themselves in daily life. The patient’s family remains an integral part of ongoing treatment, as they continue to serve as her primary support system.
The patient responded positively to treatment and began showing signs of improvement after approximately six sessions, at which point frequency was decreased to biweekly appointments. She continues to receive maintenance treatment on a biweekly-to-monthly basis to continue challenging negative thoughts and reinforcing interpersonal skills introduced during the initial stages of treatment.
Discussion
The concept of psychosis, as applied to children, is very challenging in many aspects. Children’s concepts of reality change over the course of normal development, and mature adult conceptualizations of reality are achieved only as an adolescent. Many children have normatively appropriate beliefs in fantasy figures, which would not, in themselves, suggest psychosis. It is important to note that comorbid associations with conditions such as mental retardation or other developmental disorders might pose additional problems in assessing psychotic process in children.
10Many children who develop psychosis have disturbances of behavior and cognition before onset of symptoms and marked delays in motor and verbal milestones. Such children also have impaired social skills and school achievements. Symptoms frequently seen in children with psychosis are the following: speech disturbances, inability to distinguish dreams from reality, visual and auditory hallucinations, vivid and bizarre thoughts and ideas, diminished interest, confused thinking, extreme moodiness, odd behavior, stereotypy, disinheriting, ideas that others are “out to get them” (paranoia), confusion of television with reality, and severe problems making and keeping friends.
11As referenced earlier, there are few cases of DWV associated with psychiatric symptoms in the literature. Turner et al.
12 reported the first case of schizophrenic-like psychosis in association with DWV. An 18-year-old woman presented with paranoia and hallucinations; subsequent computed tomography (CT) scan showed Dandy-Walker variant with hypoplasia of cerebellar hemispheres and vermis without evidence of hydrocephalus or supratentorial abnormalities. Her symptoms resolved without treatment. The authors were careful to note that the patient’s symptoms of psychosis and the presence of Dandy-Walker variant may have been coincidental, as they were also unable to rule out the possible concomitant use of illicit drugs.
12A second reported case of psychosis and DWV was described by Papazisis et al.
13 in a 20-year-old man who was diagnosed with early schizophrenia and comorbid obsessive-compulsive disorder. CT scan showed DWV with hypoplasia of the cerebellar vermis, dilation of the fourth ventricle and mild enlargement of the rest of the ventricular system without enlargement of the posterior fossa. Papazisis et al.
13 suggest evidence for the direct relationship between cerebellar abnormalities and psychosis, specifically involving higher-level cognitive deficits, such as impaired judgment and abstraction, mental arithmetic, and immediate and recent memory loss.
13 Before this proposal, Andreasen et al.
14,15 had suggested an elaborate model involving the frontal, cerebellar, and thalamic regions of the brain, connected through cortical-subcortical-cerebellar circuitry.
14,15Langarica and Peralta
16 also report a case of a 52-year-old woman with no past psychiatric history, who presented with paranoia, thought-withdrawal, and psychosis. On the basis of her brain CT scan, a diagnosis of Mega Cisterna Magna was confirmed. She was treated effectively with olanzapine (7.5 mg daily) and had no reported acute exacerbation on 1-year follow-up.
16In a case unrelated to psychosis, Prakash et al.
17 report on a 14-year-old young man diagnosed with hyperkinetic conduct disorder and mental retardation who was found to have imaging reports consistent with Dandy-Walker malformation.
17 This is an example of a psychiatric disorder associated with brain-imaging abnormalities, but confounded by the diagnosis of mental retardation and presumed developmental delays.
The relationship between schizophrenia and cerebellar malformations has been documented in previous research studies.
18 In a controlled study, the authors examined brain-imaging on over 50 patients and concluded that patients diagnosed with schizophrenia presented with significantly lower volumes of the entire vermis. Specifically, the posterior vermian area was smaller for participants with schizophrenia. This is consistent with findings in patients who presented with cerebellar lesions affecting affect; thus, the conclusion that these specific cerebellar lesions are noted in patients diagnosed with negative and positive symptoms of schizophrenia.
18 Abnormalities of the cerebellum, especially in the vermis, have been linked with the pathophysiology of schizophrenia and are detected not only in chronic patients but at the time of onset of this condition.
19,20Even though this patient’s MRI does not demonstrate abnormalities in the cerebellar vermis, we cannot exclude the possibility that the enlarged lateral ventricles and the enlarged inferior areas of the cerebellum are contributing to the psychotic symptomatology, including negative symptoms, such as blunted affect and anhedonia. Treatment with antipsychotics has ameliorated her paranoid and psychotic symptoms, but every time the antipsychotic medication dose is reduced, her symptoms return. Continued treatment with regard to her Dandy-Walker variant condition may include shunt placement, but it is mainly focused on treating the developmental problems, with physical or occupational therapy as well as ongoing supportive psychotherapy to improve self-esteem and general coping skills.
Despite the listed findings, further research is necessary to fully understand the possible correlation between the development of the brain, specifically the cerebellum and posterior fossa, and psychosis. The importance of recognizing new-onset psychosis and its potential relation to malformations in the brain needs to be addressed. With the malformation present since birth, early detection is vital to understanding the manifestation of psychotic symptoms and tailoring treatment options accordingly, as well as educating providers and parents about the possibility of developing future psychiatric disorders. This review highlights the necessity for a complete evaluation, including imaging studies, when presented with a child or adolescent with psychosis. At the root of the issue is a need for more research on the relationship between Dandy-Walker syndrome and psychiatric illness.