Chronic traumatic encephalopathy (CTE) is a neurodegenerative disease associated with exposure to repetitive head impacts (RHI) and is uniquely characterized by a perivascular deposition of hyperphosphorylated tau (p-tau) at the sulcal depths.
1–3 Although clinical research criteria for the in vivo diagnosis of CTE have been proposed,
4 currently CTE can only be diagnosed based on neuropathological examination using recently defined criteria.
1,3 The clinical presentation of CTE is heterogeneous and manifests as two variants (or a mixed combination): 1) initial behavioral/mood changes at a mean age of approximately 35, with later progression to cognitive deficits, and/or 2) initial cognitive impairment at a mean age of approximately 60, progressing to dementia.
5Age at symptom onset in CTE is variable, even in cases with similar neuropathological severity.
5 One factor that may affect age at onset in CTE is cognitive reserve (CR). The CR theory posits that individuals with high reserve enlist pre-existing cognitive processes or compensatory strategies to cope with neuropathological insult.
6 CR has been theorized to account for interindividual variability in the clinical course of normative aging and Alzheimer’s disease (AD), with higher CR associated with delayed onset of cognitive impairment and incident dementia.
7,8 Although CR has traditionally been linked to cognitive impairment in AD, CR has been associated with reduced behavioral disturbances in frontotemporal dementia.
9There has been recent interest in the role of CR in the manifestation of CTE symptoms
10 due to findings that higher education decreases vulnerability to cognitive dysfunction
11 and facilitates recovery following traumatic brain injury (TBI).
12 In our study examining the clinical presentation of neuropathologically confirmed cases of CTE without comorbid disease, two of three asymptomatic subjects with stage II CTE neuropathology had advanced graduate degrees (the third subject was 17 years old and had stage I CTE), raising the possibility of a CR effect in CTE.
5 No study has empirically tested the role of CR in the clinical expression of CTE. This study conducted a preliminary examination on the association between CR (operationalized by years of education and occupational attainment) and age at reported cognitive and behavioral/mood symptom onset in former professional American football players with neuropathologically confirmed CTE. The sample was restricted to subjects with stage III or IV CTE disease severity in order to limit differences in age at symptom onset due to variability in neuropathological severity. We hypothesized that higher occupational attainment and greater years of education would predict later symptom onset.
Discussion
The current study is the first to show that CR (i.e., occupational attainment) is associated with later symptom onset in a sample of former professional American football players with neuropathologically confirmed CTE stage III or IV. Occupational attainment and not years of education predicted age at symptom onset. These reserve proxies have been suggested to contribute to CR through independent paths,
19 and the discrepant findings in this study may be related to the sampling of elite athletes. Educational attainment in this sample of mostly professional football players may be more reflective of athletic prowess. The limited variability in education may also explain non-significant effects. It is possible that occupational attainment may capture those subjects who continued academics post-football, those who remained mentally and physically active throughout their life, and/or those with a high innate intellect to achieve a high occupational status.
Higher CR was associated with onset of behavioral/mood and cognitive symptoms more than 10 years later in this sample of neuropathologically confirmed cases of CTE. The relationship between CR and cognitive outcomes is consistent with the AD literature that shows CR attenuates and delays onset of cognitive impairment.
8 In addition to cognitive impairment, behavioral/mood symptoms are core features in CTE,
4 and we found a significant CR effect for behavioral/mood disturbances in CTE. Because nearly all subjects had both cognitive and behavioral/mood symptoms, the distinct influence of CR on each symptom profile is unclear. One study found higher CR attenuates behavioral disturbances (e.g., disinhibition) in frontotemporal dementia,
9 but minimal research has examined the relationship between CR and behavioral/mood symptoms. CR may mitigate the clinical phenotype associated with a specific neurodegenerative pathology, even if it is not cognitive in nature.
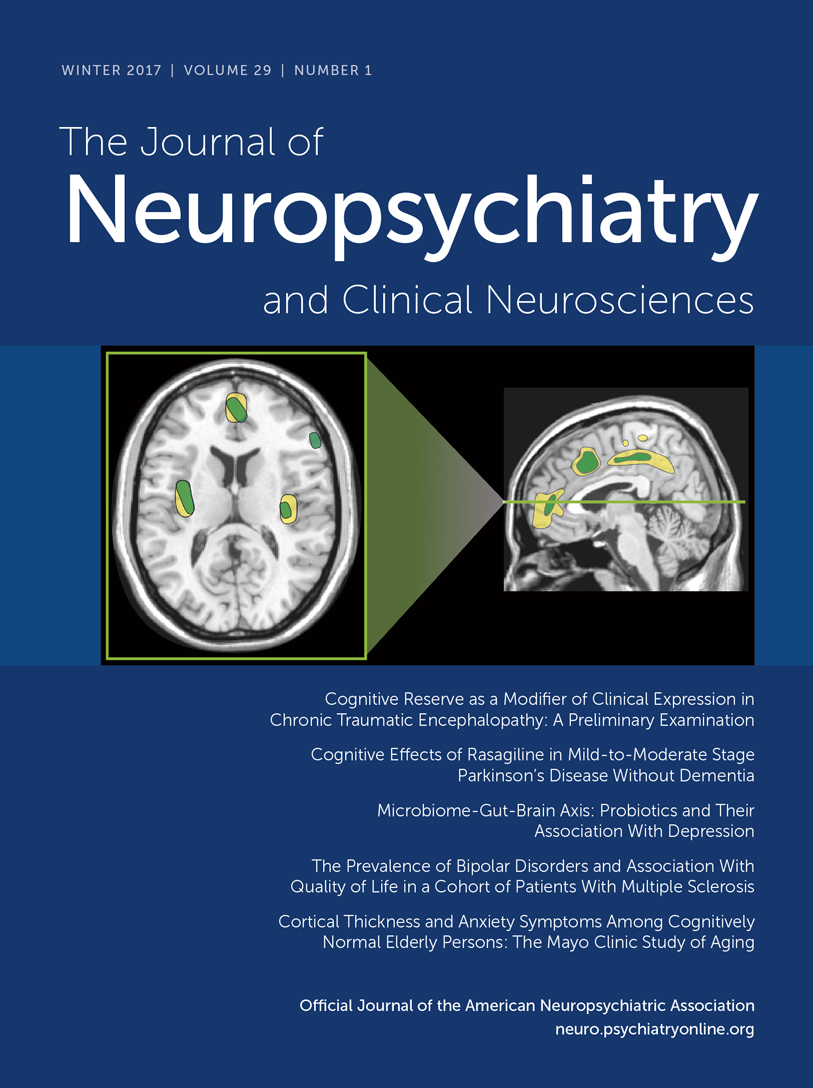
CTE is characterized pathologically by an accumulation of p-tau in neurons and astroglia distributed around small blood vessels at the cortical sulcal depths and in an irregular pattern.
1–3 As the disease progresses, p-tau accumulates in widespread cortical regions, medial temporal lobe structures, the diencephalon, and brainstem. In advanced disease, cortical atrophy is severe, and there is marked neuronal loss in the hippocampus.
1–3 Other microscopic alterations include axonal loss and white matter degeneration, chronic neuroinflammation, microvascular dysintegrity, and TDP-43 inclusions. Amyloid beta is found in approximately 50% of CTE cases and associated with age and the
APOE ε4 allele.
20 The pathological substrates underlying behavioral/mood and cognitive changes in CTE are unknown, and may involve multiple pathologies, including regional axonal damage, neuronal loss, p-tau, and TDP-43 accumulation. Based on evidence in AD, CR may modulate the clinical effects related to the neuropathological load in CTE. In a sample of 130 older Catholic clergy who underwent autopsy, greater years of education diminished the negative impact of neuritic and diffuse plaques on cognition proximate to death.
21 Past work among 165 autopsy subjects from the Rush Memory and Aging Project revealed that reduced neuronal reserve (neuronal density) in the locus coeruleus and brain stem neurofibrillary tangles (NFT) and Lewy bodies predicted rate of cognitive decline, even after controlling for pathologic burden elsewhere in the brain.
22 Such findings are noteworthy given the brainstem, especially the locus coeruleus, raphe nuclei, and substantia nigra, show high NFT density in CTE.
1 CR may also attenuate the impact of pathology on clinical expression in CTE. Investigation of CR using ex vivo neuropathological data has well-defined methodological limitations.
23 Currently, we are conducting prospective studies with objective assessments proximate to death to formally test CR as a modulator of CTE pathology. In addition, CR may also attenuate the impact of RHI on the severity of cognitive impairment,
24,25 and longitudinal research in living subjects work will examine this possibility using validated metrics of RHI exposure.
26Lastly, longer duration of football play correlated with earlier age at cognitive symptom onset. Duration of football play has been associated with CTE stage,
1 and may thus be a critical marker of RHI exposure. Notably, we did not find a relationship between duration of football play and behavioral/mood symptom onset. Different types of RHI exposure (beyond duration; e.g., specific types of hits) may differentially contribute to symptom phenotypes. Moreover, the relationship between RHI and CTE is complex and, risk factors beyond RHI exposure, including genetics, are likely critical in the pathogenesis of CTE.
The current study is preliminary, and the generalizability of our findings is limited in several ways. Our study includes a restricted sample of deceased professional football players without any other sport history and with only neuropathologically diagnosed stage III or IV CTE. Although this methodology limits confound from differences in athletic and RHI exposure and increases generalizability to CTE, the external validity of our findings, in general, and to the larger contact sport athlete population, in particular, is limited. Once sample size permits, our findings will need to be replicated in a larger sample of former athletes with various sport (e.g., soccer) and athletic backgrounds (e.g., level played) who were neuropathologically diagnosed with CTE. Even though our study did not recruit brain donors based on the presence of symptoms, the sample may demonstrate selection bias because family members are more likely to donate if their loved ones were symptomatic. A recent study from the Mayo Clinic Jacksonville neurodegenerative disease brain bank reviewed medical records and brain tissue slides of more than 1,700 male brain donors and found that 21 of 66 contact sport athletes had evidence of CTE pathology.
2 Their approach reduces ascertainment bias; thus, replication of our results in other non-CTE autopsy series would be a critical next step in the examination of a CR effect in CTE. Similarly, drawing upon other brain banks with data on sport participation history will allow for utilization of comparison (e.g., AD) and control groups (e.g., former non-contact sport professional athletes without RHI exposure) to better understand the role of CR in CTE.
Retrospective interviews introduce self-report biases (e.g., memory lapses, subjectivity). However, this approach has been shown to be reliable and valid in other dementia autopsy studies.
27 We are currently conducting longitudinal studies in living former contact sport athletes who have agreed to brain donation, and, in the future, we will examine the relationship between antemortem CR and objective test data in subjects with neuropathologically confirmed CTE. There is a lack of consensus regarding the operationalization of CR.
28 We chose educational and occupational attainment to define CR based on epidemiological evidence that they are robust markers of CR.
8 Reliability and validity of these indicators in elite athletes is unclear. In particular, there are multiple potential confounds associated with the use of occupational attainment to define CR. First, occupational attainment may be biased by athletes who died at a young age. Second, low occupational attainment may be a consequence of CTE, particularly for those with earlier onset of symptoms, rather than low cognitive reserve. Beyond these limitations, the retrospective nature of the study design precluded detailed history of lifetime occupational status (e.g., degree of responsibility). Nevertheless, this study provides initial evidence for a possible CR effect in CTE, and this finding needs to be replicated with future, prospective research studies that incorporate other proxies of CR, such as socioeconomic status or engagement in social and intellectual activities. Estimated premorbid intelligence as a proxy for CR in CTE may be problematic due to the potential negative impact of childhood RHI on intellectual and brain development.
29 Recent research highlights the potential utility of residual memory variance (i.e., residual variance in episodic memory after controlling for demographic factors and brain pathology) as a potential marker of CR
30. Our center is currently conducting prospective research to identify in vivo biomarkers of CTE (e.g., normal amyloid beta; elevated p-tau/tau ratio; PET tau specific ligands, e.g., [F-18]-T807), and once validated, we will utilize the residual memory variance approach (and others) to examine CR in subjects with “probable CTE.” Such longitudinal work will also be critical to elucidate the symptom course of CTE and whether CR attenuates decline.