When the first DSM was published in 1952, mental disorders were divided in two major groups: “disorders caused by or associated with impairment of brain tissue function,” and “disorders of psychogenic origin or without clearly defined physical cause or structural change in the brain.” The first category, referred to as “organic syndromes,” included symptoms caused by infection, intoxication, or trauma; the second category included depression, the personality disorders, and schizophrenia. As reviewed by Bürgy,
1 these categorizations were in turn based on a tradition dating back to the work of Möbius, who made a distinction between “endogenous” and “exogenous” psychoses in 1892. This distinction was maintained by authors such as Kraeplin, Jaspers, and Boenhoeffer and then crystalized by “Bumke’s equation of exogenous and somatogenic.”
In the DSM-II and DSM-III, this dichotomization between so-called “organic” and “functional” brain disorders persisted. However, defining psychiatric disorders as being nonorganic is, if one takes the meaning literally (and notwithstanding the acknowledgment of possible undiscovered causes), the equivalent of postulating that they are unrelated to the dysfunction of an organ (the brain).
2,3 As a result, there was a move by some psychiatrists to abandon this terminology. In 1992 Spitzer et al. argued for the elimination of the organic diagnostic category, calling it “familiar but now anachronistic.”
4 Neither the DSM-IV nor the DSM-5 has included the category of “organic mental disorders.”
However, organicity has remained a part of the ICD-10 classification. It is fairly common to read, “Rule out organic causes,” or, “Rule out organicity,” as part of the differential diagnosis in a psychiatrist’s report or as the reason for a consultation by psychiatry to internal medicine or neurology. This term is also pervasive in the medical literature.
5–7 When psychiatrists write, “Rule out organic causes,” they mean that it is important to rule out nonidiopathic causes—for example, hypothyroidism or other medical conditions that cause fatigue—before concluding that a given patient suffers from major depression. Using this terminology creates a duality: It casts the malfunctioning thyroid as a cause of the fatigue that can be tied to the biology of an organ, while implying that depression is not tied to the dysfunction of an organ. Without invoking mind-brain duality, it is difficult to justify categorizing symptoms resulting from malfunctioning thyroid as being more rooted in dysfunction of an organ than symptoms caused by psychiatric illnesses, such as depression. Psychosocial factors can cause or modulate these symptoms, but they do so by interacting with the experiential organ—the brain—through complex mechanisms.
One also wonders whether this antagonism between psychiatry (nonorganic) and medicine (organic) contributes to persisting stigma. There is still significant stigma associated with the diagnosis of mental illness, and psychiatry as a profession is stigmatized, at times by other members of the medical community.
8–10 There is often a sense among psychiatrists and psychiatry residents that other health professionals view psychiatry as being something different than “real medicine.”
11 If distinctions between psychiatry and so-called “physical medicine” underlie at least some of the stigma directed against psychiatry, why would psychiatrists use terminology that reinforces mind-brain duality?
There are no studies, to our knowledge, that have explored psychiatrists’ perspective on this term and the reasons underlying the persistent use of “organic cause.” To address this, we designed and conducted a quantitative and qualitative survey of Canadian psychiatrists and psychiatry residents. Understanding how psychiatrists perceive the organic-nonorganic dichotomy and why they continue to use the term “organic causes” may provide valuable insight into how psychiatrists view their practice and its relationship to the rest of medicine.
Methods
Participants
All psychiatrists, psychiatry residents, and psychiatry fellows currently practicing in Canada were eligible to participate in the survey. A total of 391 residents, fellows, and psychiatrists agreed to participate. Demographic characteristics of the study participants are summarized in
Table 1.
Survey
An electronic survey was developed by two coauthors (DB, SD). It was initially written in English and then was translated into French by two native French speakers (SD, VJP). The survey consisted of 29 items. The first 11 items were demographic questions. The next five items were questions about the participants’ use of the term “organic causes.” The last 12 items were five-point Likert scales reflecting agreement or disagreement with statements hypothesized to be possibly related to the use or “organic causes.” Participants could also leave narrative comments. From September to December 2017, participants were recruited through e-mails sent by the Canadian Psychiatric Association and the four departments of psychiatry in Quebec; the survey was distributed in English and French. This research was approved by McGill University Health Center’s research ethics board.
Statistics
All statistical analyses were performed with SPSS software (IBM SPSS Statistics 24). Descriptive statistics for all demographic variables were obtained. We used one-way analysis of variance (ANOVA) or Student’s t tests to determine whether subgroups of the sample had significantly different use of “organic causes.” We used bivariate correlations to identify items that correlated with use of the terminology; we then used significant items in a linear regression analysis.
We applied Bonferroni correction to an alpha of 0.05 to correct for multiple comparisons. This generated a significance threshold of 0.006 for tests related to demographic variables and of 0.004 for tests related to the Likert scales. We used parametric statistics even though our dependent variable of interest, the frequency of use of “organic causes,” was not normally distributed. We made this decision because the sample size was sufficiently large and tests of skewness and kurtosis were within the range of −1 to 1 (0.657, −0.679, respectively),
12 which allowed the use of parametric statistics.
13Qualitative Analysis
To reduce individual selective perception and blind interpretive bias, three of the authors (DB, VP, AD) independently conducted an inductive thematic content analysis.
14 In the first phase, the analysts open coded the narrative comments and extracted recurring themes. In the second phase, grouping and categorization of the comments led to the construction of a conceptual map of the recurring ideas.
15 After repeating this step twice independently, the authors compared the remaining themes to build the final conceptual scheme discussed below. Specific comments that the authors felt to be either exemplars of a certain viewpoint or representative of the sample as a whole were selected by the three analysts for further discussion below.
16,17Results
Quantitative Results
With respect to age, participants in our survey were in the younger age ranges. Of the 391 respondents, 52.8% were female (
Table 1).
Use of “Organic Causes” and Alternative Terminology
We found that 44.1% of respondents “almost never” used “organic cause.” Of the rest, 17.2% said they used the term monthly, 24.6% weekly, 8.5% daily, and 1.8% several times per day (3.8% were unsure of their frequency of use; mean=2.03 on a five-point Likert scale, SD=1.11, SE=0.06). When we counted those who said that they almost never used the term as “nonusers” and all other respondents as “users,” we found that 55.9% of respondents used the term regularly.
Use of the term was not associated with gender, location of training, or practice of psychotherapy. Residents reported using the term significantly more than staff (one-way ANOVA, p<0.001). Domain of practice was significantly associated with use of the term (one-way ANOVA, p=0.002), with participants in hospital-based practices (especially emergency psychiatry) and general adult psychiatry tending to use the term more. (Subgroup analysis was limited by small numbers of respondents in several groups, however.) This was mirrored by the finding that practicing in a hospital was associated with a higher tendency to use the term when compared with practicing in outpatient clinics (one-way ANOVA, p<0.001). Having shifts in the emergency room (ER) also significantly increased usage of the term (one-way ANOVA, p<0.001). Finally, there was a trend toward researchers being less likely to use the term (one-way ANOVA, p=0.02), which did not survive correction for multiple comparisons.
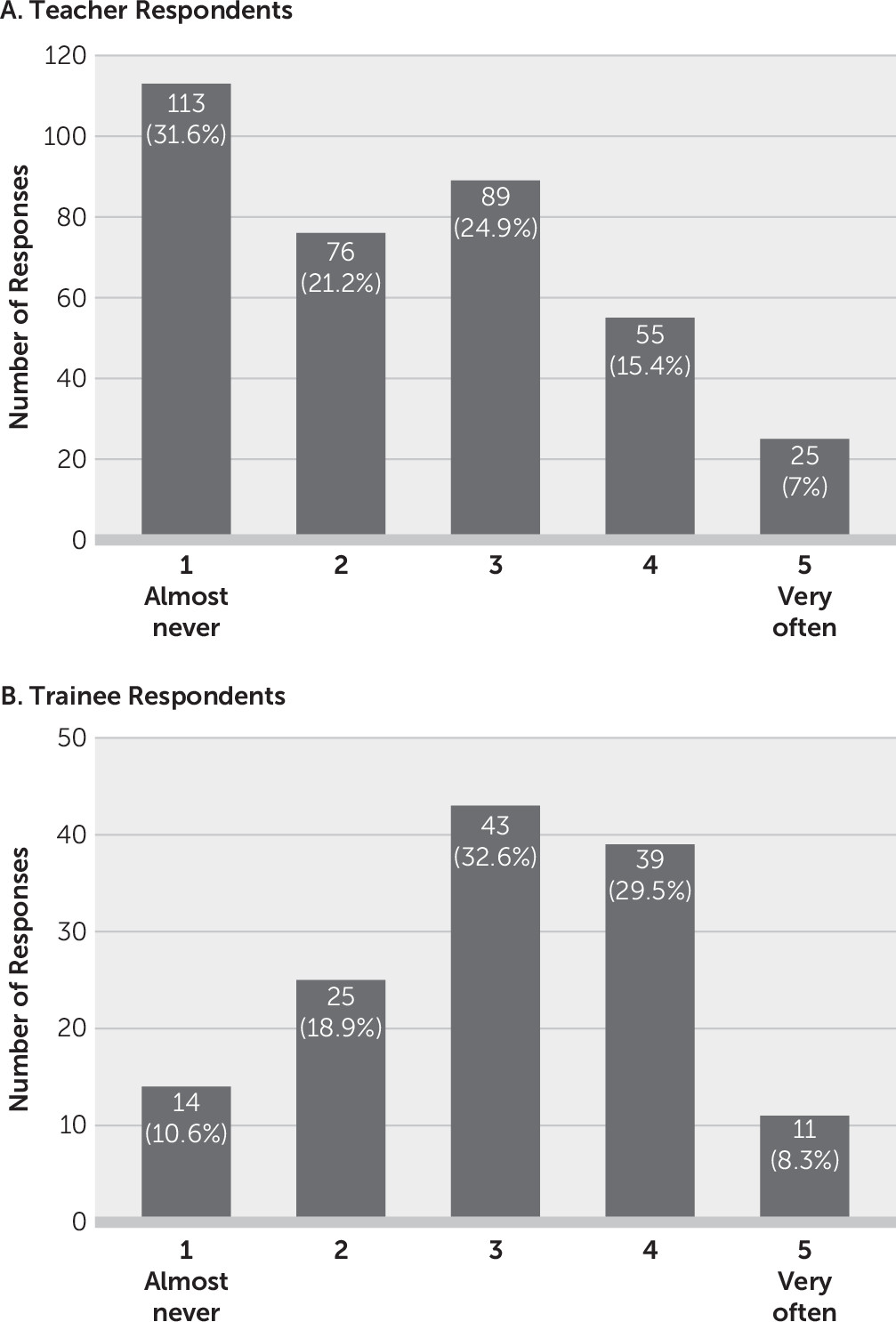
Our results demonstrate that residents seem to hear the term “organic causes” used during teaching more frequently than those teaching believe that they use it (
Figure 1). It is noteworthy that because residents are also teachers, some of the responses are from residents. When asked why they used the term, respondents (N=358) most commonly answered, “It was frequently used during my training” (36.3%), and, “Physicians from other specialties understand it” (34.4%). Results showed that 28.5% of participants found the term appropriate, and 9.6% found the term more convenient to say or write. In addition, 22.9% said they used it because other psychiatrists used it, and 20.1% said it was simply something they had always used.
We also asked participants to identify the DSM-5 terminology used to describe psychiatric symptoms related to an identified medical or neurological etiology. A total of 59.4% answered correctly (i.e., a disorder due to “another medical condition”). Thirty-eight percent answered using the previous DSM-IV-TR terminology (i.e., a disorder due to a “general medical condition”). Another 2.6% of respondents answered, “a disorder due to an organic cause.”
Likert Scales
Respondents answered a series of 12 statements using Likert scales ranging from 1 to 5 (1=strong agreement, 5=strong disagreement). Their answers showed a wide variety of opinions in response to most statements. The respondents’ answers are summarized in
Table 2. There was a tendency to believe that other physicians do not consider psychiatric conditions as having a physiological basis (mean=3.23, SD=1.075, SE=0.055). It is interesting that the tendency for respondents to feel competent investigating other medical causes of psychiatric symptoms (mean=3.34, SD=0.048, SE=0.048) contrasted with a slightly lower tendency to trust colleagues from internal medicine or neurology to exclude other medical causes of psychiatric symptoms (mean=2.89, SD=0.995, SE=0.05). There was not an agreement with the idea that the “organic causes” terminology should never be used (mean=2.82, SD=1.266, SE=0.064).
Predictors of the Use of the “Organic Causes” Terminology
We attempted to find predictors of the use of the term “organic causes.” In addition to the demographic features noted above, we identified bivariate correlations between the frequency of use and several of the Likert scales. Frequency of use showed a positive association with finding that alternative terminologies to “organic cause” are difficult to use (p<0.001).
In addition, frequency of use was negatively associated with the belief that the term “organic causes” undermines the validity of psychiatric diagnosis (p<0.001), the view that “organic causes” should not be used in psychiatry (p<0.001), and age (p<0.001). There were also associations that fell short of statistical significance when correcting for multiple comparisons between the use of “organic cause” and the belief that considering a psychiatric disorder to be present only in the absence of “organic” disease causes stigma (negative association, p=0.03) and with the belief that research will eventually explain the physiological bases of psychiatric disorders (positive association, p=0.04).
We created a linear regression model with all variables significantly (at uncorrected p value) associated with frequency of use (age, status as a researcher, the statistically significant or positively correlated Likert scale questions, the domain of practice and practice environment, and whether the participant had engaged in ER shifts as covariates) to determine the percentage of variance explained by these factors. This linear model explained 37.4% of variance in the use of “organic cause” (r2=0.374), which indicates that other variables that we have not measured might predict the use of “organic cause.” The significant predictors had the following betas and p values: belief that alternatives to “organic cause” are hard to use: β=0.221, p<0.001; age: β=–0.044, p=0.03; belief that “organic cause” should never be used: β=–0.290, p<0.001; doing ER calls: β=–0.322, p=0.01; belief that research will explain the physiological bases of psychiatric disorders: β=0.121, p=0.003.
Qualitative Results
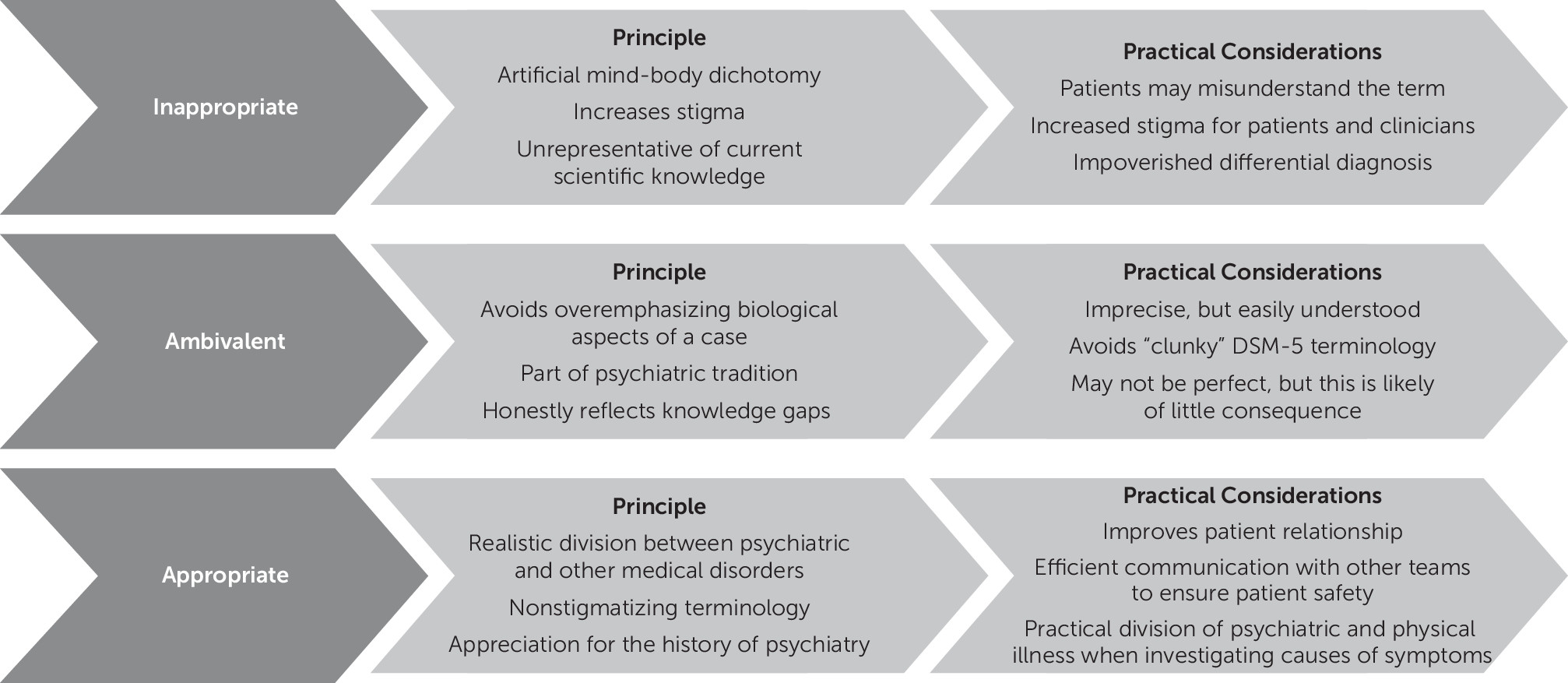
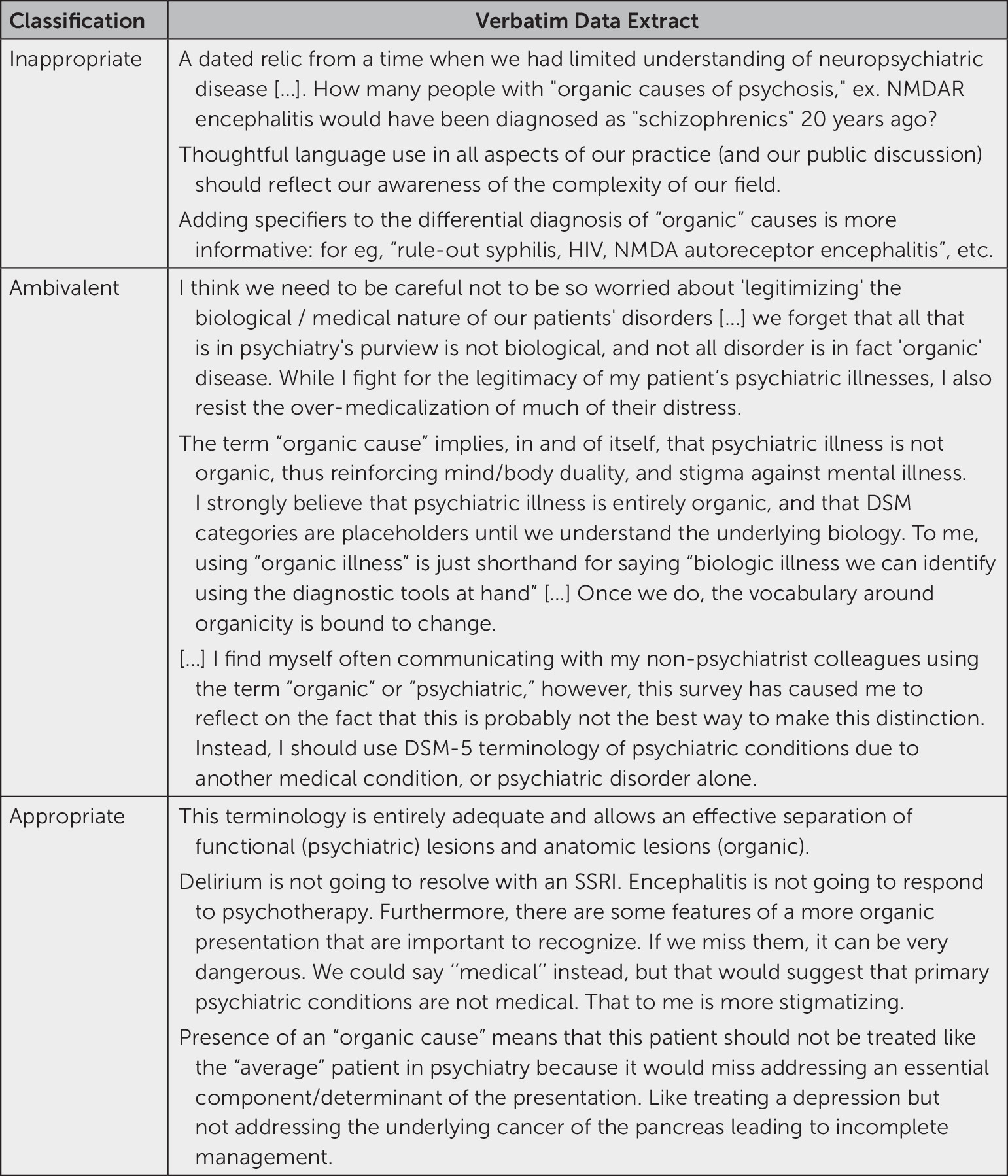
We received 290 narrative comments and analyzed them for recurring themes. Respondents seemed to fall into three groups: those who felt “organic cause’’ is inappropriate, those who were ambivalent, and those who felt it is inappropriate (
Figure 2). In the following paragraphs, each stance is further explored. Comments we felt to be exemplars of each stance can be found in
Figure 3.
Inappropriate.
These participants mentioned that they disliked the term and found it anachronistic or misleading. Many of these respondents also did not approve of the artificial mind-body dichotomy it suggests. For them, this dichotomy results in further stigmatization of psychiatry. In these participants’ opinion, the term does not reflect the current pathophysiological knowledge base. In the same vein, several of these participants reported that the use of “organic cause” led many patients to negate any contribution of physiological causes to their psychiatric illness. This could be, in their opinion, a source of stigma for psychiatric patients and psychiatrists themselves. Finally, they stated that psychiatrists should use more precise language when writing consults or differential diagnoses.
Ambivalent.
Several of these respondents made the point that it is important not to forget the nonphysiological contributors to psychiatric illness and to provide a clear distinction between psychiatric and other medical causes of psychiatric symptoms. Some of these participants leaned toward using the “organic causes” terminology because it is rooted in the history of psychiatry. They further emphasized that the term reflects the currently incomplete pathophysiological understanding of mental disorders. This subgroup of respondents also felt they were using “organic causes” as shorthand for more complicated terms. Many of them saw the DSM-5 terminology as overly cumbersome. They also questioned whether other physicians see psychiatric diagnoses as truly having a physiological basis. Much of the ambivalence in this subgroup originated from the uncertainty of the consequences of the term for their patients—that is, they were not certain about whether this term causes more stigma. Several participants simply thought that reflecting on terminology they use was simply not a priority, because it was unlikely to have any real effect.
Appropriate.
For many of these respondents, the use of “organic cause” was pragmatic; they felt its use did not result in increased stigma for psychiatry or for their patients and therefore did not view the ongoing use of “organic cause” as problematic. Several participants simply endorsed the use of the term or mentioned that they used it out of habit or out of deference to psychiatric tradition. Participants in this group noted that using “organic cause” allowed them to easily communicate with patients at a level the patients understood. This subgroup found it important to be able to use terminology that allows for clear signaling to team members, to other psychiatrists, and especially to other physicians that a patient needs investigation. One striking example relayed by a participant was of a neoplasm that was almost missed because of the reticence of the medical team to test a hospitalized psychiatric patient.
Discussion
We conducted a survey of psychiatrists, residents, and fellows to gain a deeper understanding of how psychiatrists perceive the term “organic causes” and why there is a continued use of the term to refer to other medical causes of psychiatric symptoms. The first thing to note is that the term is in common use, with 55.9% of respondents reporting that they use it at least monthly. However, this also implies that a significant proportion of psychiatrists are functioning without using “organic cause” as a communication tool. Note that we cannot exclude the possibility that a social desirability response bias led to an underestimation of the frequency of use. This is suggested by the discrepancy in the frequency of use reported by teachers versus learners.
Frequency of use of “organic causes” was correlated with some demographic factors, with younger age and practices more closely aligned with hospitals and ER call shifts being associated with more use of the term. The finding that younger age was related to increased use was unexpected, given the fact that the terminology does not appear in the DSM-IV or DSM-5. The finding that more hospital-based practice domains and environments led to increased use of the term could be due to two factors: increased likelihood of encountering rare presentations and other medical causes of psychiatric symptoms (e.g., N-methyl-d-aspartate receptor encephalitis), and more contact with other medical professionals, with whom a common language must be maintained.
Despite its ubiquity, “organic causes” is not a term endorsed by most psychiatrists and residents; less than 30% of respondents felt the term was appropriate. This reflects a discrepancy between attitudes and clinical practice, because it implies that a significant proportion of people who find the term inappropriate still use it on occasion, possibly for pragmatic reasons.
Why would psychiatrists and residents oppose discontinuing usage of a term that does not seem to, on its own, garner their support? A potential answer, echoed in several of the narrative comments, is that the term is seen as being useful to communicate to physicians from other specialties and to members of a team that a psychiatric patient requires investigation for other medical causes of psychiatric symptoms. This conclusion is supported by several findings.
First, 34.4% of respondents reported using the term because clinicians from other specialties understand it. In addition, we have the surprising finding that psychiatrists found themselves competent to investigate other medical causes of psychiatric symptoms at a slightly higher rate than they trusted colleagues from internal medicine and neurology to exclude other medical causes of psychiatric symptoms. Finally, respondents tended to feel that physicians from other specialties operate under the assumption that psychiatric disorders do not have physiological etiologies. When we take these findings together, it appears as though many psychiatrists are very concerned that other clinicians will not take seriously the need to evaluate other medical causes of psychiatric symptoms among psychiatric patients, so they resort to using a term they might not endorse in order to ensure clear communication. This concern for patient safety may be well founded, given that psychiatric patients often receive subpar medical care.
18Habit, often beginning in training, may also explain part of the term’s use. This is supported by the fact that 36.3% of respondents reported using the term because it was used frequently during their training. The complexity of alternative formulations of the “organic cause” terminology may also be a barrier to habit change. This is supported by the fact that feeling that alternative terms were complicated to use predicted being a user of the “organic cause” terminology and by the fact that 19.6% of respondents used the term because it was easy to use or write. In addition, it should be noted that 38% of respondents were still using DSM-IV terminology, which again illustrates how difficult it is to change terminology once it has become ingrained.
What does this say about psychiatry as a specialty? Is it reasonable to use terminology that in some ways maintains the division between psychiatry and the rest of medicine because we are concerned that colleagues will not do right by our patients? Are we correct in our assumptions about the way other specialties view psychiatry and psychiatric patients? These questions may be uncomfortable, but they do invite reflection and the initiation of a conversation between psychiatry and other medical specialties about our concern for our patients’ well-being and the importance of reducing stigma against mental illness within the medical community.
Our study has several limitations. As noted above, the population was skewed toward a younger, urban, and academic demographic. The online survey format allowed for a large sample size but did not allow us to collect more detailed narrative information. Finally, in an effort to keep the survey brief, we only focused on the “organic causes” terminology. This led some participants to note in the narrative comments that they felt as though there were some definite hypotheses being tested, which could have led to underreporting of the frequency of “organic cause” use (social desirability bias). It is also conceivable that those who naturally liked or disliked the “organic causes” terminology might have polarized certain answers in order to support or reduce support for varying hypotheses surrounding the use of this terminology.
Conclusions
In summary, our study identified some reasons for the continued use of the “organic cause” terminology in psychiatry. These appear predominantly to be habit, which begins in residency training, and a concern for clearly communicating to colleagues that a patient needs investigation for other medical causes of psychiatric symptoms. This argues for paying more attention to this aspect during residency training and for providing trainees with a solid basis to identify and investigate nonidiopathic causes of psychiatric symptoms. In addition, many clinicians resort to using “organic cause” because of the complexity of alternative terminology, which prompts a reflection on the appropriateness of current terminology (i.e., “another medical condition”). We hope the results in this article will foster reflection in discussion within the psychiatric community and between psychiatrists and other physicians.
Acknowledgments
The authors thank the Canadian Psychiatric Association for assistance with the distribution of this survey.