Catatonia is a neuropsychiatric syndrome that can mimic or accompany a variety of psychiatric and medical conditions. An etiology is often elusive, especially when patients present with a history with multiple confounding features. Workup for rapidly progressive illnesses such as N-methyl-d-aspartate receptor (NMDAR) encephalitis can involve multiple laboratory tests and brain imaging, such as [18F]fluorodeoxyglucose-positron emission tomography (FDG-PET). However, some catatonic behaviors may confound FDG-PET results and delay appropriate treatment. This case highlights the diagnostic and therapeutic challenges in catatonia and the potential danger of overreliance on imaging before proceeding with symptomatic treatment.
Case Report
“Mr. X” is a 60-year-old Caucasian engineering professor and missionary who presented with rapid decline in functioning over a 3-week period. His past medical history was significant for malaria several months before presentation. His psychiatric history was notable for anxiety as well as major depressive disorder that was managed with bupropion for 15 years, although the medication was discontinued about 10 months before presentation. He had resided in Ghana for the past 10 years. He was functioning normally until he commenced his engineering course. He then experienced a resurgence of depression and anxiety as a result of his fear of not being qualified to teach. Over the course of a couple of months, his minor concerns of intellectual inferiority progressed to overwrought fears of death and “doom,” at which point the patient was medically evacuated from Ghana to the United States and evaluated by an outpatient psychiatrist.
He was started on bupropion, buspirone, escitalopram, and quetiapine. Three weeks later, he was brought to the emergency department for altered mental status, a 10-lb weight loss due to anorexia, agitation, psychomotor retardation, urinary incontinence, and inability to perform activities of daily living. On physical examination, the patient was thin, lethargic, and primarily nonverbal. He had his eyes closed, grunted, and rolled in his urine. His laboratory workup and clinical assessment included a complete blood count, a comprehensive metabolic panel, urinalysis and culture, urine drug screen, blood alcohol level test, EKG, EEG, acetaminophen test, salicylate test, creatine kinase test, peripheral smear, head computerized tomography (CT), and thyroid function test. Results were notable only for mild metabolic acidosis and hypernatremia attributable to dehydration. The patient’s psychiatric medications were discontinued, and lorazepam (administered intravenously as needed) was given for his agitation and catatonic symptoms.
The patient’s working diagnoses included encephalitis and severe major depressive disorder, with psychotic features and catatonia. His 10-year residency in Ghana prompted a thorough investigation to rule out infection, toxic metabolic encephalopathy, nutritional deficiencies, autoimmune limbic encephalitis, prion diseases, and rapidly progressive dementia. Further clinical evaluation included brain MRI, lumbar puncture, electromyogram (EMG), CT of the chest, abdomen, and pelvis, and PET as well as tests for HIV antibodies, cytomegalovirus, Lyme disease, Zika virus, and chikungunya virus and assessment of rheumatoid factor levels, antinuclear antibodies, and vitamin levels. The patient’s CSF was analyzed and assessed for Epstein-Barr virus, enterovirus, herpes simplex virus, varicella zoster virus, toxoplasmosis, and NMDAR antibodies. All results were negative, pending those for NMDAR antibodies, which were examined by specialists from a send-out laboratory (
Tables 1 and
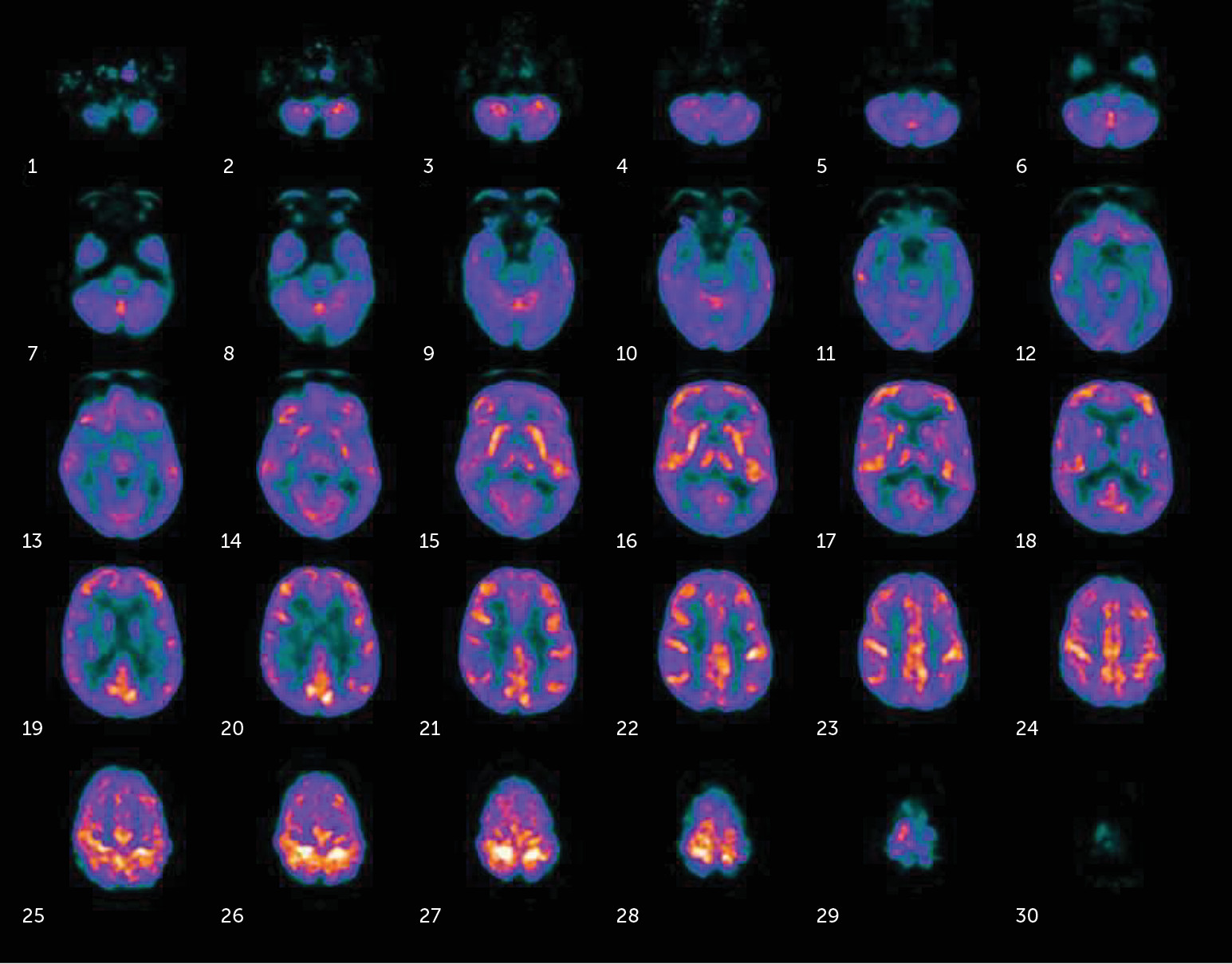
2). The patient’s MRI was unremarkable and showed only mild age-related global cerebral volume loss with mild chronic microvascular ischemic changes. However, his FDG-PET results showed slight hypermetabolism in small areas in the anterior temporal lobe and hypometabolism in the bilateral posterior temporal lobes, parietal cortex, and occipital cortex (
Figure 1).
The patient’s abnormal antero-occipital metabolic gradient raised suspicion for NMDAR encephalitis, although he did not follow instructions to open his eyes during evaluation due to negativism. EMG findings suggested chronic sensorimotor polyaxonopathy. While on the medical floor, the patient demonstrated waxing and waning levels of activity. At times, he appeared selectively mute when asked about stressors and would only follow commands with encouragement. His catatonic symptoms of negativism and mutism improved with lorazepam but only for approximately 15 minutes after administration.
Based on his FDG-PET results, the neurology team proceeded to treat the patient empirically with pulse steroids for autoimmune encephalitis, followed by intravenous immunoglobulin. He was also started on olanzapine, mirtazapine, and desvenlafaxine. His condition continued to worsen with steroid treatment, and he was promptly transferred to inpatient psychiatry to begin ECT for major depressive disorder with psychotic features and catatonia. Upon admission to psychiatry, his Montreal Cognitive Assessment (MoCA) score was 21/30.
He received eight ECT sessions with ketamine augmentation. After the first session, he gradually increased his oral intake of food but continued to be noncommunicative, with severe psychomotor retardation. As his ECT sessions progressed, he was able to ambulate with a walker and converse with hospital staff. Significant improvement was noted following the fifth session. He began attending group sessions, exhibited curiosity about his treatment, asked about the mechanism and history of ECT, and self-reported marked improvement in his depressive symptoms. His cognition improved, with an MoCA score of 26/30, and his score on the Patient Health Questionnaire-9 was 14.
The patient was discharged with prescriptions for mirtazapine, desvenlafaxine, and olanzapine. After his discharge from the hospital, a pan-negative serum and CSF NMDAR antibody panel arrived (
Tables 1 and
2). He completed an intensive outpatient program and was followed up for 2 months. He continued to function well without cognitive deficits, and his outpatient score on the MoCA was 28/30. He was ultimately able to resume his teaching career.
Discussion
The above case demonstrates the multiple challenges in both diagnosis and treatment. The patient presented with rapid and steep decline from baseline functioning over a 3-week period, essentially going from teaching engineering at a university to requiring assistance with all activities of daily living. His psychiatric history was remarkable for depression, which was managed with bupropion. He was in remission for several months after discontinuing the medication. In the context of having been a professor of mathematics and computer science for years, the stressors of teaching his first engineering course appeared to be minor. However, he resided in Ghana for 10 years and received treatment for malaria months before he started teaching, which raised suspicion for toxic and infectious causes of encephalopathy. While in the emergency department, he showed minimal improvement with lorazepam, for only minutes at a time, which could have easily been attributable to the waxing and waning nature of his delirium. However, a complete encephalopathic workup for toxicity and infectious etiology was unremarkable.
Evidence for NMDAR encephalitis was ambiguous. CSF evaluation was negative for lymphocytic pleocytosis and oligoclonal bands.
1,2 Brain CT and MRI were also unremarkable, but the results were not reliable given that more than 50% of patients with NMDAR do not have abnormal findings.
1,3 The patient’s EEG was normal, without slowing or epileptic activity, which would be unusual in autoimmune encephalitis.
1 It is noteworthy that an EMG showed chronic sensorimotor polyaxonopathy and some demyelination predominant in the lower extremities; however, our patient demonstrated lack of cooperation and inability to follow commands. An FDG-PET showed slight hypermetabolism in small areas in the anterior temporal lobe and hypometabolism in the bilateral posterior temporal lobes, parietal cortex, and occipital cortex. Although this pattern is consistent with other cases reported in the literature,
3–5 hypometabolism in the visual cortex also overlaps with findings in Lewy body dementia and could have been due to our patient closing his eyes throughout the procedure. Abnormalities on EMG and FDG-PET in our case highlight how behavior can confound results. Especially during catatonic states, patients are often not responsive to instructions, or they may be oppositional. When our patient was asked to open his eyes for the FDG-PET, he closed them even tighter.
The patient’s condition continued to deteriorate amid deliberation. Despite indeterminate findings in synthesis of the case, NMDAR encephalitis became the most probable cause, since it could not be excluded due to delay in laboratory processing. Unfortunately, steroid treatment was ineffective. Catatonia due to a primary psychiatric illness, a diagnosis of exclusion, was the remaining possibility. In review of various interactions with team members, signs of depression became apparent. At times, the patient’s behavior appeared volitional, because he followed one-step commands only with encouragement. He had lucid moments in which he communicated that he was hospitalized for depression, but he would close his eyes and grunt when asked about specific stressors. Also, he exhibited nihilistic and parapsychotic features before admission, believing that he was dying and incapable of eating or drinking and expressing a sense of “impending doom.” The case literature examining the psychological state of patients with catatonia illuminates similar themes of death and fear of impending danger and overwhelming defeat. Some patients have described preoccupation with haunting images and thoughts while in a catatonic state.
6 It is possible that our patient’s worry about inferiority and failure evolved into an overwhelming fear of death that precipitated and sustained catatonia. On the other hand, reports of catatonia secondary to NMDAR encephalitis often include physical symptoms such as convulsions, headache, and dyskinesias, which were not present in our patient.
7,8 Future studies may stratify symptoms of catatonia on the basis of etiology, which could be helpful in narrowing the differential diagnosis.
Our patient’s marked improvement with ECT was expected given the high rate of response from clinical experience. However, despite presenting with catatonic symptoms, he did not receive ECT until 7 days after admission. His physical deterioration was mostly a result of his refusal to eat or drink. To reduce risk of developing further complications, he may have benefited from an earlier course of ECT while undergoing medical evaluation.
9,10 Furthermore, case review suggests that ECT may be safe and effective in patients with suspected NMDAR encephalitis, regardless of immunotherapy, especially among patients with catatonic symptoms.
7The above case demonstrates several obstacles encountered when evaluating a patient with catatonia. The patient’s complicated social history led to an extensive investigation with confounding results. Although FDG-PET is valuable in detecting NMDAR encephalitis, patients with catatonia who exhibit various behaviors may have a false-positive result that can obstruct clinical judgment. Regardless of etiology, ECT is safe and effective in alleviating acute symptoms and should be strongly considered during medical evaluation and treatment.